| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 13, Number 1, January 2022, pages 31-35
Change in Pelvic Incidence Associated With Sacroiliac Joint Dysfunction: A Case Report
Eric Chun Pu Chua, c , Arnold Yu Lok Wongb
aNew York Chiropractic and Physiotherapy Centre, Hong Kong, China
bDepartment of Rehabilitation Sciences, The Hong Kong Polytechnic University, Hong Kong, China
cCorresponding Author: Eric Chun Pu Chu, New York Chiropractic and Physiotherapy Centre, Hong Kong, China
Manuscript submitted October 14, 2021, accepted December 23, 2021, published online January 17, 2022
Short title: Change in PI in Sacroiliac Joint Dysfunction
doi: https://doi.org/10.14740/jmc3816
| Abstract | ▴Top |
The sacroiliac joint (SIJ) is designed primarily for stability with minute motions. SIJ dysfunction refers to improper movement of the SIJs. Diagnosis and evaluation of SIJ dysfunction are difficult, with use of physical maneuvers and image-guided anesthetic injection. This case report describes a 47-year-old female who experienced right buttock pain and painful limp for approximately 2 months. Standing radiographs revealed inflammatory sclerosis surrounding the right SIJ. Physical examination found tenderness over the right SIJ and positive results in provocation (the distraction, compression, and thigh thrust) tests, compatible with right SIJ dysfunction. Her pain was resolved and gait performance was retrieved following 6-month program of combined thoracolumbar manipulation and rehabilitation exercises. Unexpectedly, change in pelvic incidence (PI) angles was noticed on follow-up radiograph. PI remains more or less fixed throughout adult life since the mobility of the SIJs is considered negligible. The current presentation is designed to explore the significance of PI change. The PI disparity unfolds the possibility of recognizing SIJ dysfunction based on consecutive radiographs.
Keywords: Chiropractic; Pelvic incidence; Sacroiliac joint dysfunction; Spinal manipulation
| Introduction | ▴Top |
Sacroiliac joint (SIJ) dysfunction refers to a state of altered biomechanics of the SIJ [1]. The sacrum does not exhibit much motion with respect to the ilium and SIJs are slackened only during pregnancy. Excessive or restricted motion may affect extra-articular structures surrounding the SIJs (such as the sacrotuberous, sacrospinous, and/or iliolumbar ligaments) and results in pain [2]. SIJ dysfunction can result from repetitive stress, degeneration, lumbar deformities, inflammation and prior lumbar fusion [1, 3]. SIJ dysfunction is difficult to be profiled on radiographic views. Clinical screening usually relies on pain provocation tests and analgesic response to the SIJ injection. Observing aberrant position or movement of the SIJ is the foundation of diagnosing SIJ dysfunction.
Pelvic incidence (PI) is a radiographic parameter describing the relative position of the sacral endplate in relation to the pelvis [4]. PI used to be considered as a constant parameter throughout adult life [4-6]. Minimal PI changes with respect to postural alteration have been described in normal individuals [7], but the implications of PI change under pathological conditions have not yet fully investigated [8-10].
Here we describe our experience in a 47-year-old female with SIJ dysfunction successfully treated with 6 months of chiropractic intervention. Follow-up radiograph showed interval change in all the spinopelvic parameters, including PI. PI disparity between two consecutive radiographs ran contrary to the notion that PI remains more or less constant since the mobility of the SIJs is considered negligible. By exploring the contradictory event, we postulate that PI change would be a potential role for recognizing SIJ dysfunction.
| Case Report | ▴Top |
Investigations
A 47-year-old female investment banker complained of right buttock pain for approximately 2 months. The patient used to participate in marathon races. Six months before her first chiropractic visit, she experienced a right gluteal strain, while she was performing stair climbing exercise. The pain resolved spontaneously after 2 days. During the period of pandemic-related restrictions on mobility, she worked from home and started to frequently experience soreness in her right buttock and lower back, which could be relieved by walking and gentle stretching. However, her right buttock and low back symptoms worsened over the subsequent 2 months. Sitting could aggravate pain and prevented her from using a laptop to work from home. During her first orthopedic workup, lumbar magnetic resonance imaging did not identify abnormalities. The patient was given acetaminophen and ibuprofen for pain relief, while physiotherapy was used for treating right buttock pain. Four weeks later, she sought chiropractic attention because of the worsening of her right buttock ache that shot down her right posterior thigh and a limp on the right side while walking.
Diagnosis
On examination, the patient used a cane for ambulation and had an antalgic gait affecting the right side. Standing posture observation revealed anterior pelvic tilt (PT), right pelvic drop and anterior rotation of the left pelvis. Pain was induced by axial extension, standing or leaning on the right leg. The self-reported peak pain intensity of her buttock and low back pain was 8 - 9/10 on an 11-point numeric pain rating scale, where 0 means no pain and 10 means the worst imaginable pain. Physical examination identified motion restriction at C5/6, C7/T1, T3/T4, L1/L2, and L4/L5 levels, as well as a painful right SIJ. The passive lumbar flexion and extension ranges of motion were limited. Palpation over the right SIJ elicited tenderness. The response of distraction provocation (by applying vertically pressure to the anterior superior iliac spine), compression provocation (by applying pressure to the pelvis over the iliac crest), and the thigh thrust test (by applying an anteroposterior shear force to the SIJ through the flexed hip) were positive in the right SIJ. Muscular hypertonicity was palpated at bilateral upper trapezius, left quadrates lumborum, and right gluteus medius/minimus and hamstrings. Sensory and motor functions were identical and intact bilaterally. Radiographs (Fig. 1a) revealed posterior sacral tilting (counter-nutation), forward left innominate and twisted lumbar spine. An inflammatory sclerosis (black arrow head) on the iliac side of the right SIJ was evident. Her clinical pictures, positivity in three provocation tests and radiological findings were consistent with right SIJ dysfunction.
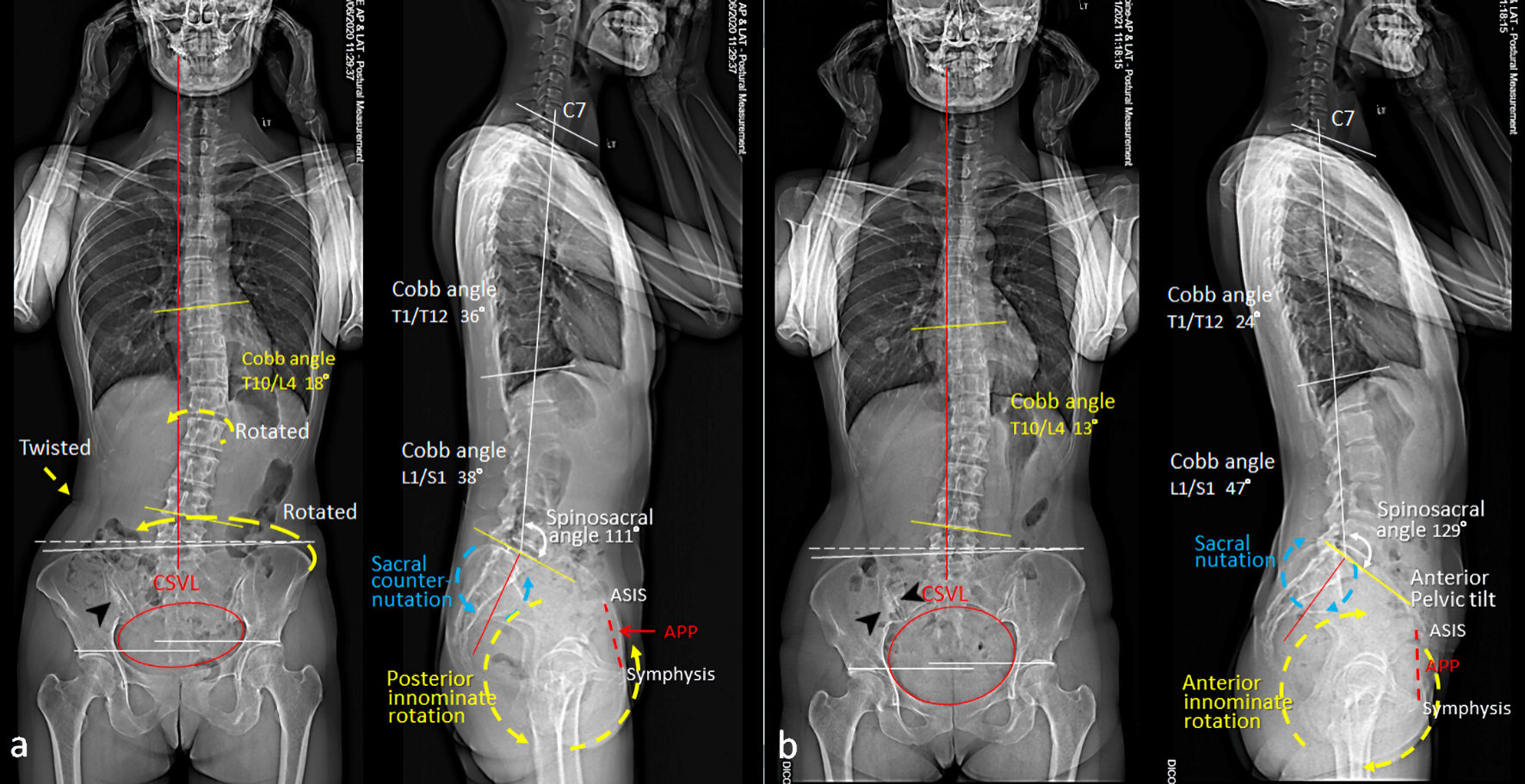 Click for large image | Figure 1. Comparison of standing assessment pre- and post-treatment. (a) Initial radiographs revealed an inflammatory sclerosis (black arrow head) on the iliac side of the right sacroiliac joint (SIJ), sacral counter-nutation (backward rotation, blue circle), posterior pelvic tilt (yellow circle), forward left innominate and twisted lumbar spine. (b) Six months later, radiographs showed dense sclerosis surrounding the right SIJ (black arrow heads), sacral nutation (forward rotation, blue circle) and anterior pelvic tilt (yellow circle). Normally, the range of motion of the SIJ does not exceed 3° and nutation occurs during increased load-bearing situations e.g., standing and sitting. APP: anterior pelvic plane (dashed red line); ASIS: anterior superior iliac spine; CSVL: central sacral vertical line (red line). |
Treatment
The patient underwent chiropractic intervention, which included spinal manipulation to the restricted spinal segments, mobilization of the restricted joints, and therapeutic ultrasound therapy and soft tissue massage to the hypertonic muscles. She was started with three sessions per week. After 1 month, the patient reported buttock and low back pain reduced from 8 - 9/10 down to 2/10 on an 11-point numeric pain scale, where 0 indicates no pain and 10 indicates the worst pain imaginable [11]. She stopped her pain medication and resumed work. Thoracolumbar adjustment along with rehabilitation exercises, including hamstring stretch, gluteal squeeze and squat, were added to correct the spinal alignment and strengthen muscle functions. Treatment frequency was reduced to two times a week.
Follow-up and outcomes
The patient reported complete resolution of symptoms alongside full hip and back mobility 6 months after the beginning of treatments. No adverse events had occurred. Improvements in patient’s physical function were associated with the corresponding changes in the spinopelvic alignments (Fig. 1b) and differences observed in all the radiographic parameters (Fig. 2). The disparity in PI, sacral inclination, sacral slope (SS), etc., between the pre- and post-treatment measurements denoted destabilized condition of the SIJ complex. A comparison of initial and follow-up measurements is summarized in Table 1 [4-6].
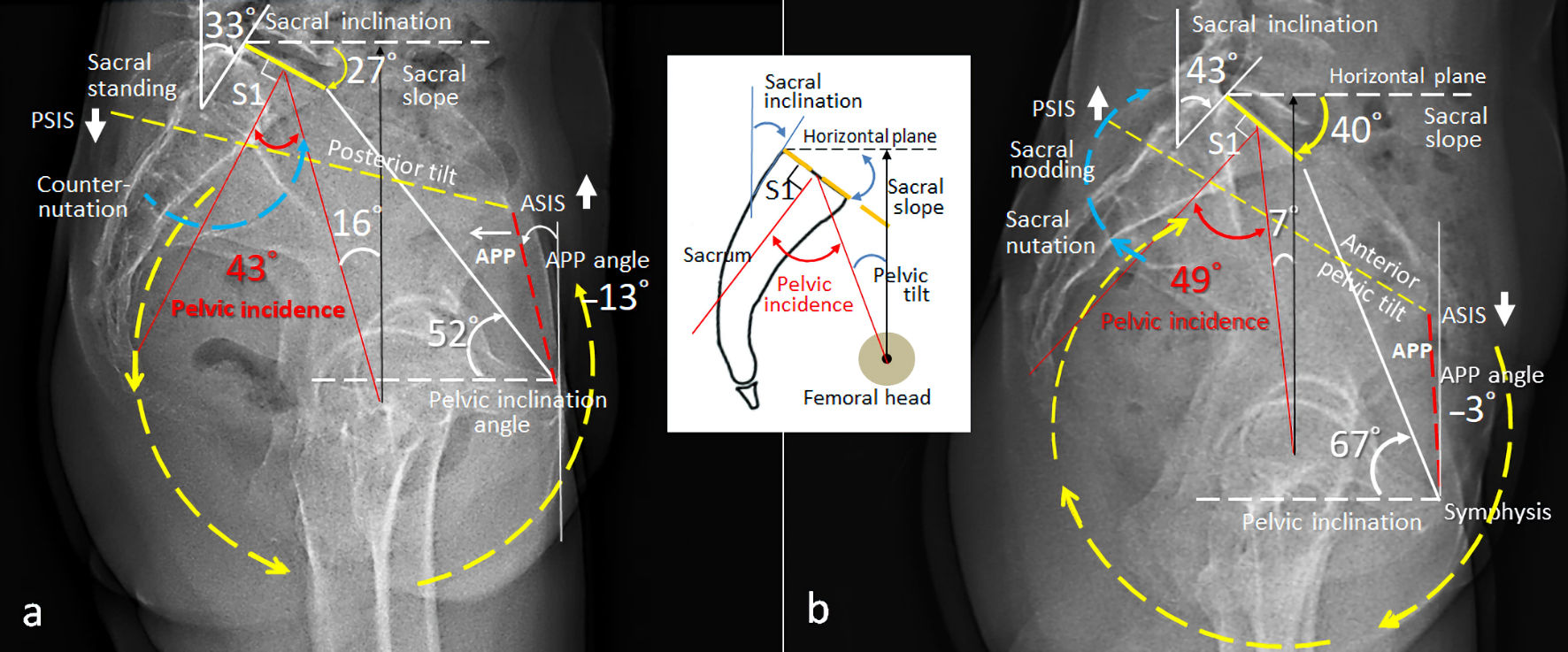 Click for large image | Figure 2. Comparison of spinopelvic parameters measured before and after chiropractic care. (a) Pre-treatment radiograph revealed counter-nutation of the sacrum (blue circle), sacral inclination 33°, sacral slope 27°, posterior innominate rotation (yellow circle), and posterior pelvic tilt (APP angle -13°, pelvic inclination 52°). (b) Six months later, interval change in all the measurements was demonstrated on the follow-up radiograph. Pelvic incidence (PI) has been considered as a static parameter in health individuals. Significant PI change (43° vs. 49°) between two consecutive radiographs is suggestive of sacroiliac instability. APP: anterior pelvic plane (dashed red line); ASIS: anterior superior iliac spine; PSIS: posterior superior iliac spine. A schematic depicting geometries for the pelvic measurements is inserted. |
 Click to view | Table 1. Comparison of Spinopelvic Parameters Before and After Treatment |
| Discussion | ▴Top |
The SIJ, by nature, is not pressure resistant to axial load or rotation in relation to the ilium. Compared to the standing position, sitting brings the lower lumbar segments to undergo flexion, thereby increasing loading on the sacrum [12]. A sedentary lifestyle involving little or no physical activity may generally reduce the translational activity of collagen protein for formation [13], and also affects the tensile strength of the tendons and ligaments, being more prone to injuries [14]. In consequence, the biomechanics of the SIJ will be altered and compromised with regard to its function of load transference and motor control, resulting in SIJ dysfunction [15]. The history of sport-related right buttock pain of our patient could be a risk factor for a repetition of SIJ injury. Joseph et al reported that individuals with SIJ dysfunction had reduced muscle mass of the ipsilateral local and global systems, and proposed the use of exercise therapy and manual therapy for stabilizing and strengthening the muscles surrounding the SIJ [15].
Diagnosis of SIJ dysfunction is often a challenge due to the complex anatomy and biomechanics of the joint [16]. Clinicians typically rely on composites of pain provocation results [17]. These maneuvers include distraction, thigh thrust, compression, sacral thrust, Gaenslen and FABER (flexion-abduction-external rotation) tests [16, 17]. Positivity in three out of six provocation tests was adopted as the criterion [17]. However, positive provocation tests are unable to distinguish between the SIJ and adjacent affected structures, having poor inter-examiner reliability [16]. Anesthetic blocks only identifying the anatomical location of pain do not determine the etiology of SIJ pain [17]. Furthermore, SIJ pain can present through localized and/or referred pain from any stimuli in any structure segmentally innervated by L5 to S3 spinal nerves [18]. As such, the identification of dysfunctional joints requires a reliable modality, with a focus on functional kinematic relations and the integration of structural constructs. The identification of improper sacroiliac motions is the foundation of diagnosing SIJ dysfunction.
Stability and flexibility modes are simultaneously counter-opposing states in the SIJ and place conflicting demands on its joint construction. From Hippocratic times to modern times, one of the most contentious issues in SIJ research has been the mobility of the joint [19]. Amplitudes and nature of sacroiliac motion have been debated and studied extensively. The physiological range of motion of the SIJ does not exceed 3° in rotations and 2 mm in translations along axes [3]. In biomechanical studies, sacral rotation (nutation and count-nutation) in the sagittal plane was mainly investigated to compare with the changes of spinopelvic parameters. A dysfunctional SIJ may result in spinopelvic complex misalignment, including pelvic rotation, pelvic obliquity, lumbar rotation, and painful symptoms [19], as seen in Figures. 1 and 2.
Measuring the radiographic spinopelvic parameters such as PI, PT, and SS has gained importance in reconstructive surgery of the spine [5, 20]. The schematic diagram in Figure 2 depicts geometries for parameter measurements commonly utilized in clinical settings. PI is defined as the angle subtended by a line perpendicular to the midpoint of the sacral endplate and a line from this point to the axis of the femoral head [21]. In geometry, “incidence” refers to a binary relation between different types of object in space [4]. PI angle remains more or less constant throughout adult life since the mobility of the SIJs is considered negligible beyond childbirth [4-6].
There have been a number of studies on the PI change in clinical settings. A retrospective study of 72 patients who had obtained flexion and extension radiographs of the lumbar spine showed that intra-individual PI change from flexion-extension was quite small, with a mean of -0.94° [22]. Researchers [7, 20] observed 84-88% of healthy subjects experienced a change in PI when the subjects varied their pelvic position, with a mean of 2.12° to 2.9° measured on standing radiographs. A computed tomography (CT) study [23] in 24 healthy subjects showed that PI changed by 3.2° when standing and supine positions were compared. X-ray or CT examination itself did not affect the measurements but postural changes were reflected in the results [23].
The angle of incidence is the algebraic sum of two dynamic angles, SS and PT. PI = SS + PT. As the sacrum is the entire weight of the spine to rest on, PI is the angle correlating with lumbar lordosis through SS and consequent spine degeneration [21, 24]. Although PI has been considered as a static parameter in health individuals, it can be seen that when the sacral inclination changes in destabilized conditions, PI changes [4]. The PI correlates strongly with the position of the sacrum in space and could contribute to a marker of SIJ stability.
Studies have found strong association between PI changes and destabilized conditions of the SIJ. Researchers observed the disparity of PI in patients after surgical correction of the fixed lumbar deformities [8, 9]. The disparity in PI after surgery was significantly greater in non-sacropelvic fixation [8]. Sacroiliac fixation could diminish the PI variability [8]. Mikula et al have reported an association between postural PI change and advanced SIJ degeneration [10]. The disparity in PI angle was explained by increasing motion across the SIJ in pathological status [8-10].
Radiographic measurements of PI have been independently utilized by various medical professionals after defining and agreeing to the specific manner of measurement. It should be aware that the spinopelvic parameters are dynamic and change in different positions to a few millimeters or degrees, at most [25]. The implications of a variable PI could have consequences for implant placement, stabilization techniques, classification schemes, as well as for some treatment alternatives [20]. Remarkable PI changes need to be correlated to individual patients to determine if the changes reflect destabilized conditions of the SIJ. Understanding the associations between the sacral motion and pelvic parameters can improve clinical assessment and treatment planning.
Conclusions
As this is a retrospective study, the main limitation is lack of control group. The drawbacks of not having a control can be partially addressed by the key observational point, i.e., PI. PI remains more or less constant throughout adult life since the mobility of the SIJs is considered negligible [4-6]. PI disparity itself between consecutive measurements could be a surrogate measure for the comparison. The other limitation is that PI change was noticed after treatment, not the basis used in making diagnosis of SIJ dysfunction on the first visit. By exploring the contradictory event, we postulate that PI change would be a potential role for recognizing SIJ dysfunction. While it is often difficult to generalize results from a single case to a larger population, further studies are required to corroborate this issue and to determine the optimal interval for repeating radiography.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
The authors declare no potential conflict of interest.
Informed Consent
Informed consent was obtained from the patient for case publication.
Author Contributions
EC was mainly involved in diagnosis and treatment of this patient. AW drafted the report. All authors read and critically reviewed the manuscript, and then approved the final submitted version.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
Abbreviations
CT: computed tomography; PI: pelvic incidence; PT: pelvic tilt; SIJ: sacroiliac joint; SS: sacral slope
| References | ▴Top |
- Wong M, Sinkler MA, Kiel J: Anatomy, Abdomen and Pelvis, Sacroiliac Joint. In: StatPearls. Treasure Island (FL), 2021.
- Boyle K. Conservative management for patients with sacroiliac joint dysfunction. In: Norasteh AA. Low Back Pain. Rijeka, Croatia: InTech 2012. p. 293-332.
doi - Kiapour A, Joukar A, Elgafy H, Erbulut DU, Agarwal AK, Goel VK. Biomechanics of the Sacroiliac Joint: Anatomy, Function, Biomechanics, Sexual Dimorphism, and Causes of Pain. Int J Spine Surg. 2020;14(Suppl 1):3-13.
doi pubmed - Ramchandran S, Buckland A, Errico TJ. Pelvic incidence (PI) is more easily understood as the pelvic base angle (PBA). Spine Res. 2017;3:1.
doi - Le Huec JC, Thompson W, Mohsinaly Y, Barrey C, Faundez A. Sagittal balance of the spine. Eur Spine J. 2019;28(9):1889-1905.
doi pubmed - Pizones J, Garcia-Rey E. Pelvic motion the key to understanding spine-hip interaction. EFORT Open Rev. 2020;5(9):522-533.
doi pubmed - Rezvani M, Tabesh H, Saboori M, Akrami A, Shafiei M, Akrami MR. Pelvic incidence angle in standing, maximal anterior and maximal posterior pelvic rotation in a sample of healthy subjects. Acta Med Iran. 2018;56(12):796-802.
- Lee JH, Na KH, Kim JH, Jeong HY, Chang DG. Is pelvic incidence a constant, as everyone knows? Changes of pelvic incidence in surgically corrected adult sagittal deformity. Eur Spine J. 2016;25(11):3707-3714.
doi pubmed - Kleck CJ, Noshchenko A, Burger EL, Cain CMJ, Patel VV. Postoperative pelvic incidence (PI) change may impact sagittal spinopelvic alignment (SSA) after instrumented surgical correction of adult spine deformity (ASD). Spine Deform. 2021;9(4):1093-1104.
doi pubmed - Mikula AL, Fogelson JL, Oushy S, Pinter ZW, Peters PA, Abode-Iyamah K, Sebastian AS, et al. Change in pelvic incidence between the supine and standing positions in patients with bilateral sacroiliac joint vacuum signs. J Neurosurg Spine. 2021;34(4):617-622.
doi pubmed - British Pain Society and Faculty of Pain Medicine. Outcome Measures. London: British Pain Society and Faculty of Pain Medicine; 2019. p. 7.
- Patwardhan AG, Sielatycki JA, Havey RM, Humphreys SC, Hodges SD, Blank KR, Muriuki MG. Loading of the lumbar spine during transition from standing to sitting: effect of fusion versus motion preservation at L4-L5 and L5-S1. Spine J. 2021;21(4):708-719.
doi pubmed - Dideriksen K, Boesen AP, Reitelseder S, Couppe C, Svensson R, Schjerling P, Magnusson SP, et al. Tendon collagen synthesis declines with immobilization in elderly humans: no effect of anti-inflammatory medication. J Appl Physiol (1985). 2017;122(2):273-282.
doi pubmed - Magnusson SP, Kjaer M. The impact of loading, unloading, ageing and injury on the human tendon. J Physiol. 2019;597(5):1283-1298.
doi pubmed - Joseph LH, Hussain RI, Naicker AS, Htwe O, Pirusan U, Paungmali AP. Pattern of changes in local and global muscle thickness in local and global muscle thickness among individuals with sacroiliac joint dysfunction. Hong Kong Physiother J. 2015;33(1):28-33.
doi - Hamidi-Ravari B, Tafazoli S, Chen H, Perret D. Diagnosis and current treatments for sacroiliac joint dysfunction: a review. CurrPhys Med Rehabil Rep. 2014;2(1):48-54.
doi - Telli H, Huner B, Kuru O. Determination of the Prevalence From Clinical Diagnosis of Sacroiliac Joint Dysfunction in Patients With Lumbar Disc Hernia and an Evaluation of the Effect of This Combination on Pain and Quality of Life. Spine (Phila Pa 1976). 2020;45(8):549-554.
doi pubmed - von Heymann W, Moll H, Rauch G. Study on sacroiliac joint diagnostics. Manuelle Medizin. 2018;56:239-248.
doi - Vleeming A, Schuenke MD, Masi AT, Carreiro JE, Danneels L, Willard FH. The sacroiliac joint: an overview of its anatomy, function and potential clinical implications. J Anat. 2012;221(6):537-567.
doi pubmed - Place HM, Hayes AM, Huebner SB, Hayden AM, Israel H, Brechbuhler JL. Pelvic incidence: a fixed value or can you change it? Spine J. 2017;17(10):1565-1569.
doi pubmed - Chen HF, Zhao CQ. Pelvic incidence variation among individuals: functional influence versus genetic determinism. J Orthop Surg Res. 2018;13(1):59.
doi pubmed - Schroeder N, Noschenko A, Burger E, Patel V, Cain C, Ou-Yang D, Kleck C. Pelvic incidence changes between flexion and extension. Spine Deform. 2018;6(6):753-761.
doi pubmed - Eddine TA, Migaud H, Chantelot C, Cotten A, Fontaine C, Duquennoy A. Variations of pelvic anteversion in the lying and standing positions: analysis of 24 control subjects and implications for CT measurement of position of a prosthetic cup. Surg Radiol Anat. 2001;23(2):105-110.
doi pubmed - Li Y, Sun J, Wang G. Lumbar lordosis morphology correlates to pelvic incidence and erector spinae muscularity. Sci Rep. 2021;11(1):802.
doi pubmed - Haffer H, Becker L, Putzier M, Wietholter M, Ziegeler K, Diekhoff T, Pumberger M, et al. Changes of fixed anatomical spinopelvic parameter in patients with lumbosacral transitional vertebrae: a matched pair analysis. Diagnostics (Basel). 2021;11(1):59.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


