| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 14, Number 9-10, October 2023, pages 322-326
Chronic Pancreatitis-Induced Thrombosis of Celiac and Superior Mesenteric Artery
Harshavardhan Sanekommua, e , Sobaan Taja, Rida Mah Noorb, Muhammad Umair Akmalc, Claudia Ramireza, Pranav Shahd, Mohammad Hossaina, Asif Arifa
aDepartment of Medicine, Jersey Shore University Medical Center, Neptune City, NJ 07753, USA
bInternational University of Kyrgyzstan-International School of Medicine, Eastern Campus, Bishkek, Kyrgyzstan
cKazakh National Medical University, Almaty, Kazakhstan
dDepartment of Radiology, Jersey Shore University Medical Center, Neptune City, NJ 07753, USA
eCorresponding Author: Harshavardhan Sanekommu, Department of Medicine, Jersey Shore University Medical Center, Neptune City, NJ 07753, USA
Manuscript submitted May 10, 2023, accepted July 1, 2023, published online October 13, 2023
Short title: Chronic Pancreatitis and Thrombosis
doi: https://doi.org/10.14740/jmc4112
| Abstract | ▴Top |
Every year, nearly 60,000 hospitalizations occur in the United States due to chronic pancreatitis (CP). CP can cause severe chronic abdominal pain, pancreatic insufficiency, and increased risk of pancreatic cancer. While venous thrombotic complications are common, arterial thrombotic events are rarely reported in CP. This report describes a case of a 43-year-old female who presented with severe worsening abdominal pain due to CP. Diagnostic imaging disclosed thrombosis of superior mesenteric artery (SMA) and celiac artery (CA) with acute bowel wall changes reflecting ischemic changes, resulting in acute-on-chronic mesenteric ischemia. Endovascular stent placement relieved the ischemia with the resolution of pain. Arterial thrombosis should be considered as a diagnostic possibility when patients with CP present with a significant change in symptoms. Importantly, the case demonstrates that endovascular treatment with stent placement can relieve ischemia and resolve symptoms in patients with CP.
Keywords: Pancreatitis; Chronic; Ischemia; Mesenteric; Occlusive mesenteric arterial ischemia
| Introduction | ▴Top |
Chronic pancreatitis (CP) is characterized by chronic inflammation, fibrosis, and scarring of the pancreas, leading to damage and loss of various cells in the organ, including exocrine, endocrine, and ductal cells [1, 2]. This condition is associated with several clinical symptoms such as abdominal pain, pancreatic insufficiency, pancreatic cancer, and other complications. The underlying mechanism for CP is inflammation-led fibrosis. Previously, acute pancreatitis (AP) and CP were considered distinct entities [1, 2]. However, recent research suggests that AP, recurrent AP (RAP), and CP represent a continuum of disease. CP’s etiology is traditionally classified into categories such as alcohol, hereditary, obstructive, hyperlipidemia, and idiopathic. However, recent evidence suggests that most patients have multiple risk factors, and the TIGAR-O classification system groups these risk factors based on modifiers that may interact to produce pancreatic disease [2]. TIGAR-O is an acronym that groups some of the risk factors and etiologies behind CP. As the letter would indicate, it expands into six categories: toxic-metabolic, idiopathic, genetic, autoimmune, recurrent and severe AP and obstructive [2].
CP is associated with splanchnic vein and portal vein thrombosis and can also lead to arterial erosion and rupture of pseudoaneurysm [3, 4]. Arterial thrombosis has been rarely reported. Thus far, a single case report of celiac trunk thrombosis has been documented in the literature [3]. This report presents a case of superior mesenteric artery (SMA) and celiac artery (CA) thrombosis secondary to CP. This article also provides a literature review of arterial thrombotic events related to pancreatitis.
| Case Report | ▴Top |
Investigations
A 43-year-old female with a history of idiopathic CP and juvenile rheumatoid arthritis presented with epigastric pain, nausea, and vomiting for the past 3 days. While she had experienced similar pain from her prior episodes of pancreatitis, this episode demonstrated a significant change in the pain severity. Because of the pain episodes in the past 6 months, she often went days without eating, resulting in significant weight loss. At the time of admission, she was in acute distress due to epigastric pain. Her blood pressure was 142/93 mm Hg with a heart rate of 101 beats per minute. She was breathing at a rate of 22 breaths per minute with saturation of 97% on room air. She was afebrile (37 °C). Abdominal examination revealed epigastric tenderness to light palpation.
Diagnosis
She had a white blood cell count of 16.8 × 103/µL, 84% neutrophil (normal: 4.5 to 11.0 × 103/µL), alkaline phosphatase 149 U/L (normal: 44 - 147 U/L), and lipase 163 U/L (normal: 0 - 160 U/L). With concern for necrotizing pancreatitis, an abdominal computed tomography angiogram (CTA) was obtained. While some calcification at the pancreatic head was present, complete obstruction in the SMA, and severe stenosis in the CA were seen (Fig. 1a, b). Consequently, patient had signs of ischemic small bowel (Fig. 2). There was no evidence of atherosclerotic disease from the imaging. A comparison with CT scan of the abdomen performed 6 months ago did not reveal these findings (Fig. 3). Patient was admitted for acute-on-chronic pancreatitis complicated by arterial thrombosis and stenosis resulting in acute-on-chronic mesenteric ischemia (CMI).
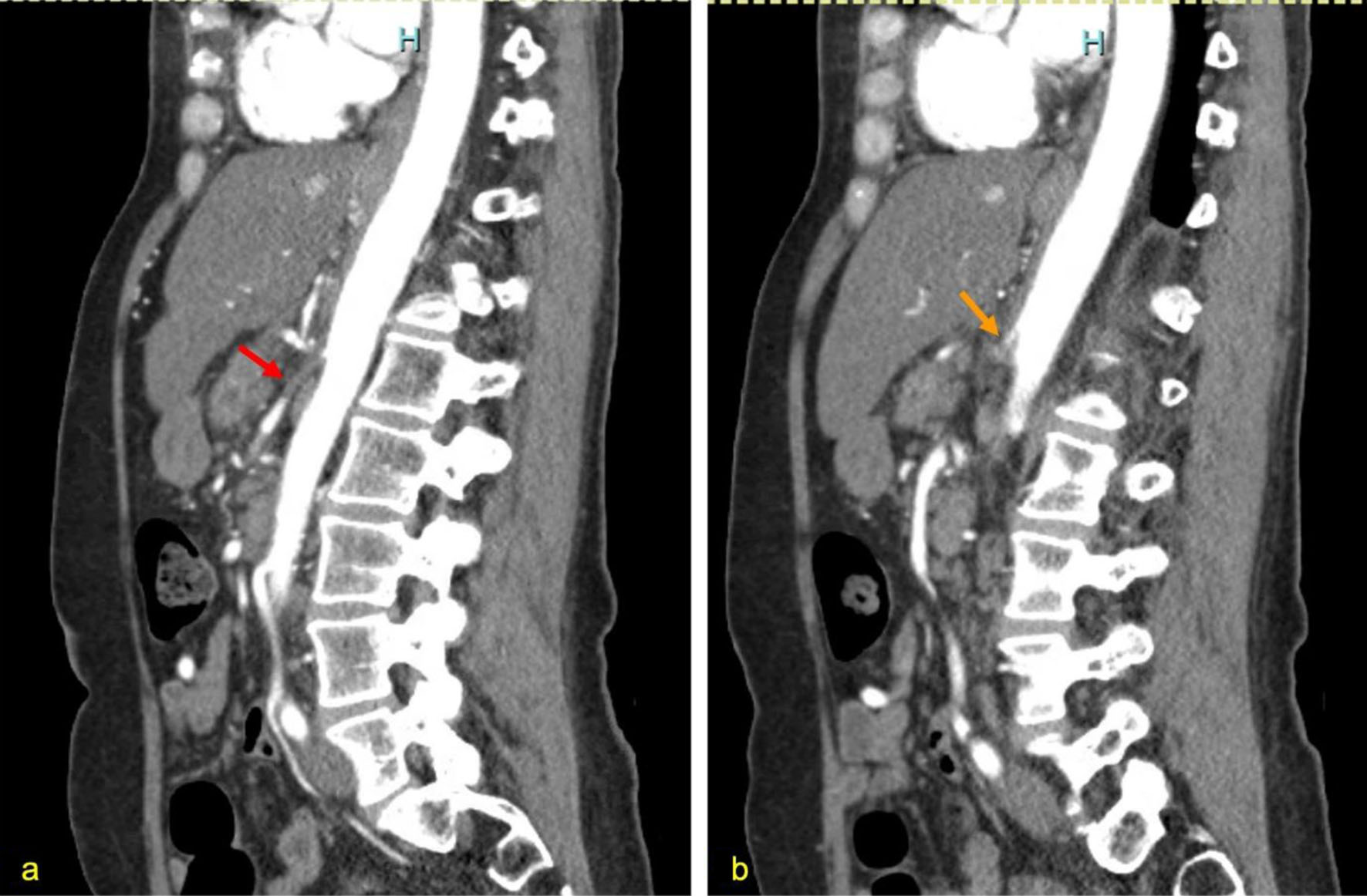 Click for large image | Figure 1. (a) Complete superior mesenteric artery thrombosis (red arrow), indicated by the filling defect. (b) Celiac artery narrowing/stenosis indicating chronic thrombosis (orange arrow). |
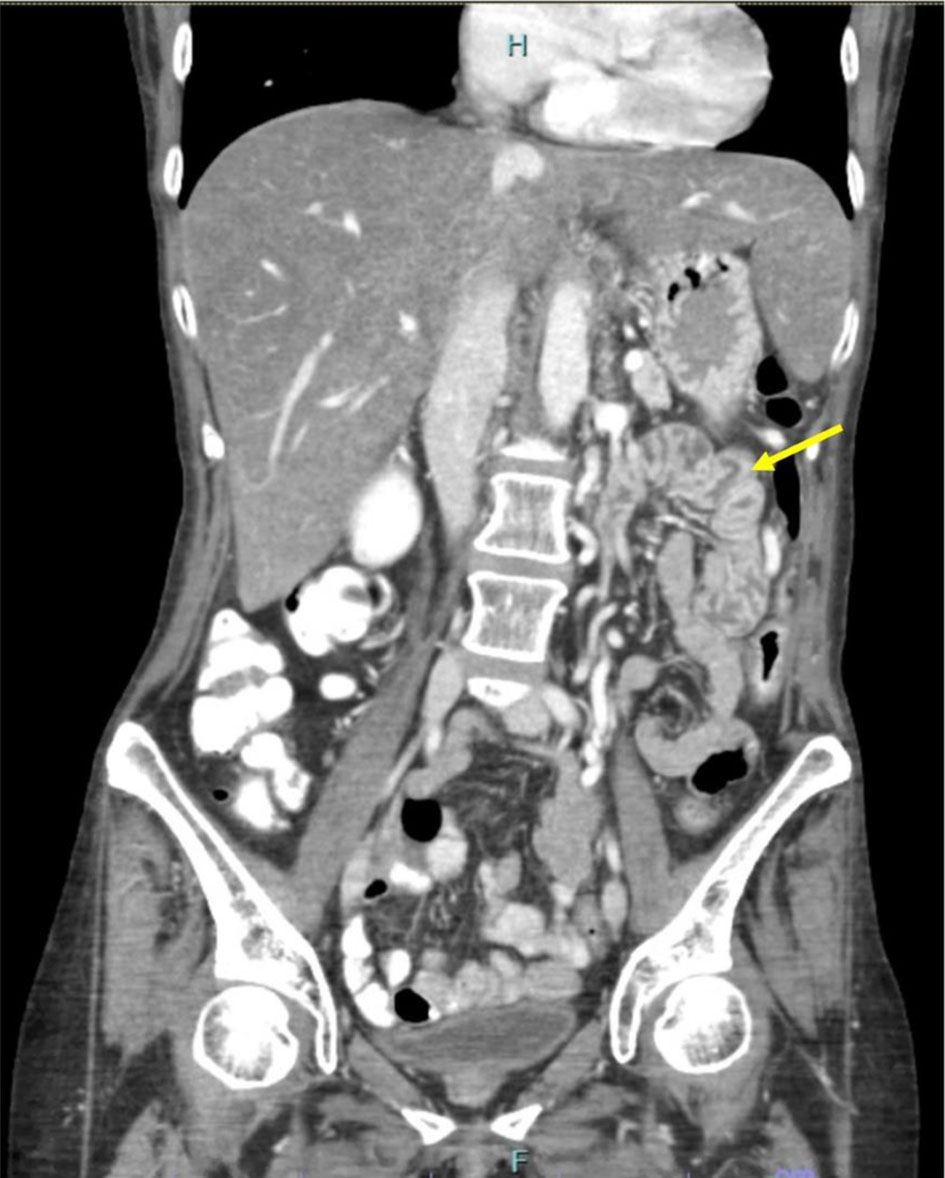 Click for large image | Figure 2. Coronal view of CT of abdomen/pelvis. There is prominent jejunal wall thickening with layers of high and low attenuation indicating submucosal edema from likely from acute ischemia (yellow arrow). CT: computed tomography. |
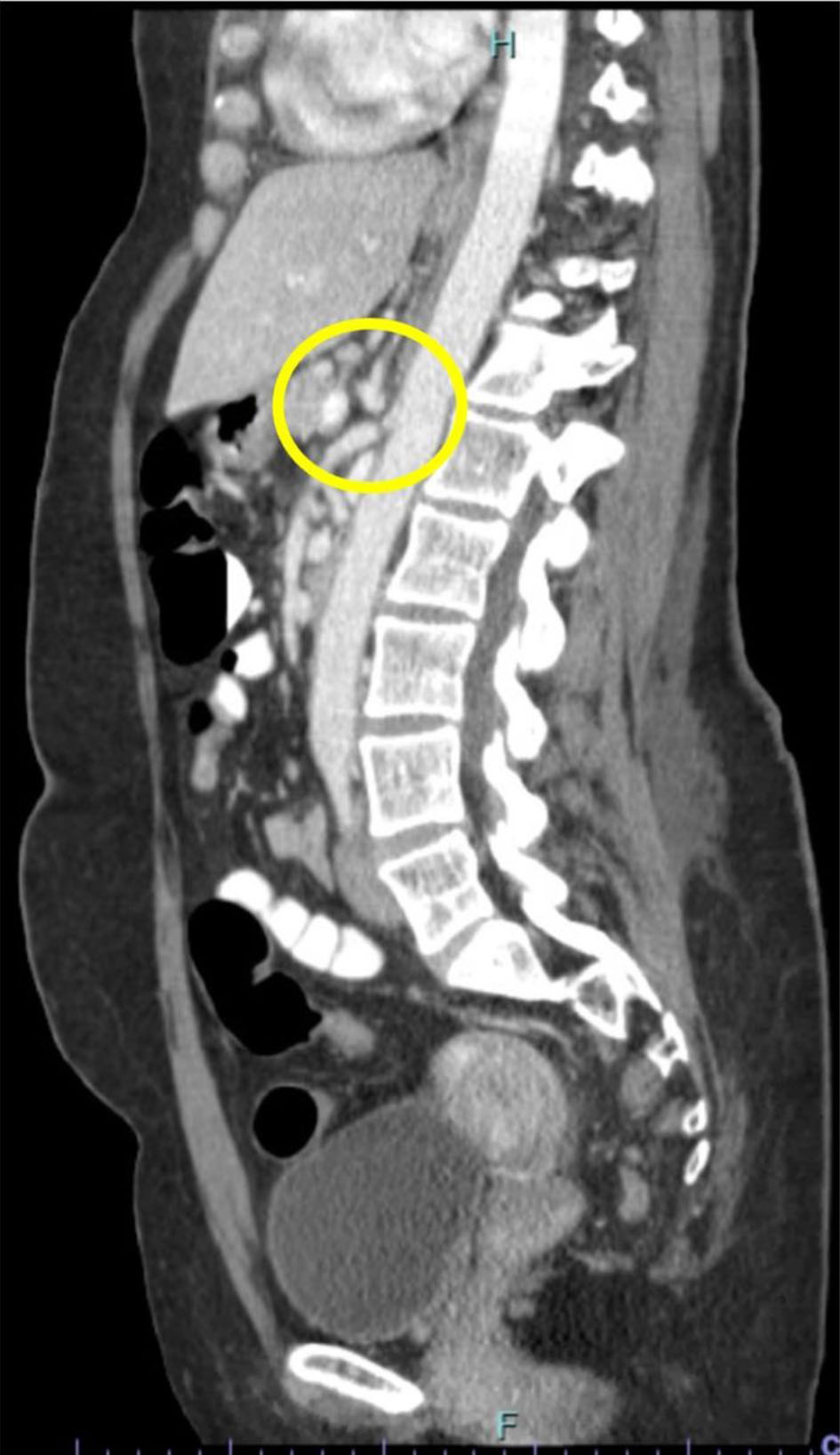 Click for large image | Figure 3. CT of abdomen/pelvis 6 months prior showing patent CA and SMA as they branch from the abdominal aorta (yellow circle). CT: computed tomography; CA: celiac artery; SMA: superior mesenteric artery. |
Treatment
After receiving aggressive intravenous fluids and achieving pain control, she was started on a heparin drip. She was taken to the interventional radiology laboratory and successfully underwent thrombectomy and stent placement of SMA and CA through the transradial approach. Both SMA and CA were stented by a bare-metal balloon mounted stent. The patient’s pain and symptoms improved, enabling her to tolerate solid foods with minimal pain over the next 2 days. She was initiated on oxycodone/paracetamol for chronic pain management and was discharged on apixaban.
Follow-up and outcomes
On an outpatient basis, extensive autoimmune workup, including antineutrophil cytoplasmic antibodies, cryoglobulins, complements, serum protein electrophoresis and immunofixation, urine immunofixation, antinuclear antibody, and rheumatoid factor, was all negative. Similarly, hypercoagulable workup, which included lupus anticoagulant, beta-2 glycoprotein, anticardiolipin antibodies, prothrombin, factor V Leiden, protein C and S mutation, and hepatitis panel was negative. The patient’s arterial thrombosis was attributed to her CP.
Over the next year, the patient had recurrent pain and was found to have stent migration necessitating further vascular procedures. At a follow-up of 1 year, pain is well managed by pain medication.
| Discussion | ▴Top |
CP can lead to vascular complications such as venous thrombosis and arterial pseudoaneurysm [2]. Arterial thrombosis from pancreatitis is rare and often associated with acute necrotic pancreatitis [2]. This article reports a rare occurrence of acute-on-chronic arterial thrombosis and stenosis of the SMA and CA and its management with vascular interventional procedure and stent placement.
AP induces thrombosis through inflammation, compression of surrounding vessels, inappropriate coagulation activation, and tissue factor release [4]. CP also produces a prothrombotic state, increasing vascular complications by three times compared to AP [2]. To the best of our knowledge, arterial thrombosis in CP has been reported in only one case [3]. That patient underwent emergent gastrectomy and splenectomy due to gastric necrosis and splenic infarct. In our patient, chronic thrombosis was diagnosed based on the clinical presentation and development of gradual symptoms over 6 months, consistent with chronic mesenteric ischemia. The CT imaging findings also suggest an acute component of the thrombosis as there is evidence of acute bowel wall changes due to the ischemia. The presence of underlying stenosis in the case presented here provided a strong reason for stasis of blood flow with ensuing thrombosis.
Several risk factors for venous thrombosis and pseudoaneurysms in patients with pancreatitis, including male gender, a history of alcohol abuse, organ failure, and necrosis of the pancreas have been identified [2]. However, many additional risk factors remain unidentified due to the paucity of available information on arterial thrombosis in pancreatitis cases. Among the 10 cases identified, there was an equal distribution of females and males, with an average age of 51.4 years (Table 1 [3, 5-12]). None of the patients had a history of prior thrombosis, and hypertension was the most identified comorbidity. Interestingly, three cases had a history of alcohol abuse [3, 6, 7] and three had a history of abdominal surgical procedures [8, 9]. Sixty percent of the cases had severe necrotizing pancreatitis, while the rest did not specify the severity level. The affected arteries varied greatly, with kidneys being the most affected organ, leading to one patient being fully dependent on hemodialysis [10]. Thrombosis in the SMA was described in two cases [8, 11], while celiac trunk thrombosis was only reported in one case of CP [3]. The earliest reported case resulted in bilateral renal artery thrombosis from necrotizing pancreatitis, leading to acute renal failure and death [6]. None of the cases demonstrated a stenosis in the arterial tree. Our case demonstrated an arterial stenosis in the CA with complete occlusion of SMA and required stent placement.
 Click to view | Table 1. A Summarization of All the Cases of Arterial Thrombosis in the Setting of Pancreatitis |
The management of arterial thrombosis was similar across most cases, IV heparin followed by oral anticoagulation. In severe cases, surgical management was necessary [3, 7, 8]. Our patient received heparin drip initially followed by oral apixaban. The three primary vessels that supply to the large and small bowels are CA, SMA, and inferior mesenteric artery (IMA). CMI is usually asymptomatic until two of the three primary vessels are occluded [13]. Once patients become symptomatic, revascularization is necessary as untreated symptomatic CMI has an extremely high 5-year mortality rate approaching 90-100% [13, 14]. Our patient underwent a revascularization procedure involving stent placement in the SMA and CA due to worsening symptoms including severe abdominal pain.
Conclusion
Patients with CP who present with severe abdominal pain may develop thrombosis and stenosis of the SMA and CA. It is essential for clinicians to identify any change in the frequency or characteristics of abdominal pain, especially in patients who are chronically in pain. If there is a change, a necessary workup, including imaging, should be performed to evaluate not only visceral but also vascular complications that can cause a significant burden in this patient population. In our case, we successfully treated thrombosis of SMA and CA leading to chronic CMI with an endovascular procedure and stent placement. However, clinicians should be aware that migration of a stent can occur, which may necessitate additional procedures. Thus, heightened awareness of this complication is crucial for optimal management of CP patients presenting with severe or worsening abdominal pain.
Learning points
The learning points from this article include that CP can lead to vascular complications, such as venous thrombosis and arterial pseudoaneurysm, and that chronic thrombosis in the SMA and CA is a rare occurrence. Patients with CP are at an increased risk of vascular complications due to the prothrombotic state caused by the condition. Risk factors for vascular complications in patients with pancreatitis include male gender, a history of alcohol abuse, organ failure, and necrosis of the pancreas. The management of arterial thrombosis in pancreatitis patients typically involves IV heparin followed by oral anticoagulation, and surgical management may be necessary in severe cases. Revascularization is necessary once patients become symptomatic, as untreated symptomatic CMI has an extremely high 5-year mortality rate approaching 90-100%.
Acknowledgments
None to declare.
Financial Disclosure
No financial support was given for this paper.
Conflict of Interest
There is no conflict of interest from any of the parties involved.
Informed Consent
Informed consent was obtained from the patient for publication of this case report.
Author Contributions
HS, ST, RMN, and MUA are all the main writers. CR helped in literature review. PS helped identify the radiographical images of significance. MH and AA reviewed the paper and edited it extensively for content and style.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Levy P, Dominguez-Munoz E, Imrie C, Lohr M, Maisonneuve P. Epidemiology of chronic pancreatitis: burden of the disease and consequences. United European Gastroenterol J. 2014;2(5):345-354.
doi pubmed pmc - Vujasinovic M, Dugic A, Nouri A, Brismar TB, Baldaque-Silva F, Asplund E, Rutkowski W, et al. Vascular complications in patients with chronic pancreatitis. J Clin Med. 2021;10(16):3720.
doi pubmed pmc - Challand C, Titcomb D, Armstrong CP. Pancreatic pseudocyst causing celiac artery trunk thrombosis. JOP. 2008;9(4):512-514.
pubmed - G. C. M. A. Pancreas Study Group. Practice guidance for diagnosis and treatment of pancreatitis-related splanchnic vein thrombosis (Shenyang, 2020). J Dig Dis. 2021;22(1):2-8.
doi pubmed - Mishreki AP, Bowles MJ. A case of widespread aortic thrombosis secondary to acute severe pancreatitis. Ann R Coll Surg Engl. 2011;93(4):e17-18.
doi pubmed pmc - Vogel RM, Keohane M. Renal vascular abnormalities in acute pancreatitis. Arch Intern Med. 1967;119(6):610-616.
pubmed - Chong BK, Yun JK, Kim JB, Park DH. Multiple ascending aortic mural thrombi and acute necrotizing mediastinitis secondary to acute pancreatitis. Korean J Thorac Cardiovasc Surg. 2016;49(5):401-404.
doi pubmed pmc - Chait J, Duffy E, Marks N, Rajaee S, Hingorani A, Ascher E. Superior mesenteric artery thrombosis after necrotizing pancreatitis. Ann Vasc Surg. 2019;59:307.e20.
doi pubmed - Hahn TL, Dalsing MC, Sawchuk AP, Cikrit DF, Lalka SG. Primary aortic mural thrombus: presentation and treatment. Ann Vasc Surg. 1999;13(1):52-59.
doi pubmed - Thajudeen B, Budhiraja P, Bracamonte ER. Bilateral renal artery thrombosis secondary to acute necrotizing pancreatitis. Clin Kidney J. 2013;6(5):503-506.
doi pubmed pmc - Garcia-Rodriguez V, Jacob R, daSilva-deAbreu A. A rare case of pancreatitis-induced thrombosis of the aorta and superior mesenteric artery. Methodist Debakey Cardiovasc J. 2019;15(3):220-222.
doi pubmed pmc - Verbeeck N, Cavez N, Plawny L, Weber J, Lens V. Primary aortic thrombosis: role of enhanced multislice CT demonstrated in three exceptional cases. JBR-BTR. 2014;97(2):76-80.
doi pubmed - Campbell EA, Silberman M. Bowel Necrosis. 2022.
- Waack A, Jaggernauth S, Sharma S. Bilateral common iliac vein stent migration. Radiol Case Rep. 2022;17(11):4332-4336.
doi pubmed pmc
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


