| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 3, Number 1, February 2012, pages 84-88
Pediatric Colocolic Intussusception With Pathologic Lead Point: A Case Report
Robert Bradford Abrahamsa, Arie Francoa, b, Kristopher Neal Lewisa
aDepartment of radiology, Georgia Health Sciences University, 1120 15th Street, Augusta, GA 30912, USA
bCorresponding author: Arie Franco
Manuscript accepted for publication October 21, 2011
Short title: Pediatric Colocolic Intussusception
doi: https://doi.org/10.4021/jmc402w
| Abstract | ▴Top |
Intussusception is one of the most common causes of acute abdominal pain in the pediatric population. The majority of cases are idiopathic and ileocolic in location. Colocolic intussusception is an uncommon type of intussusception in children that is usually associated with a pathologic lead point. In this article, a case of colocolic intussusception in a four-year-old male secondary to juvenile polyps is presented followed by a discussion of intussusception and the available imaging modalities used in diagnosis and treatment.
Keywords: Intussusception; Colocolic; Polyp; Juvenile
| Introduction | ▴Top |
Colocolic intussusception is an uncommon type of intussusception in children that is usually associated with a pathologic lead point. We present a case of recurrent colocolic intussusceptions in a 4-year-old male, erroneously thought to be the most common ileocolic type. Following surgery, a lead point was found, juvenile polyps in the transverse colon.
| Case Report | ▴Top |
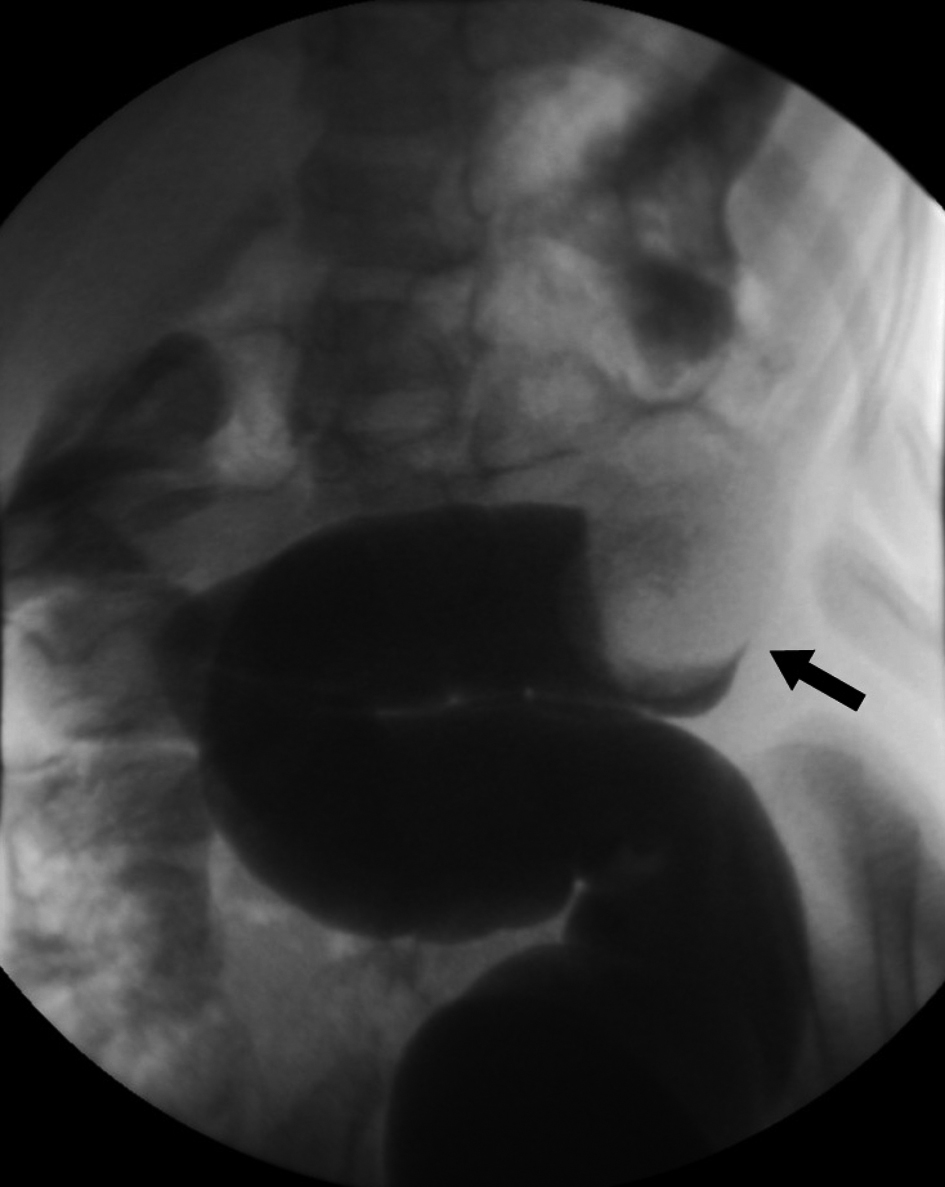
A 4-year-old male was brought to the clinic by his parents with worsening vomiting and diarrhea for three days. His parents have observed him curling up and arching his back intermittently and recently had one episode of bloody stools. His past medical history was unremarkable with the exception of uncomplicated surgical excision of penile skin bridges at two years of age. The patient was referred to our institution for an abdominal ultrasound to evaluate for intussusception. The ultrasound showed a 7.3 × 2.7 ×3.7 cm mass in the left lower quadrant with a target-like appearance consistent with intussusception (Fig. 1). The diagnosis was confirmed with air enema and the intussusception was successfully reduced (Fig. 2). The patient was admitted for observation and discharged the following morning in good condition. Five days later, the patient’s parents found him curled up and brought him back to the hospital. The patient was admitted and ultrasound was performed which again demonstrated an abdominal mass with a target sign. The intussusception was successfully reduced with air contrast enema (Fig. 3) and exploratory laparoscopy was performed to search for a meckel’s diverticulum or mass lesion. At surgery, there was no evidence of meckel’s diverticulum or other lead point at the serosal surface of the small bowel or colon. The patient was discharged in good condition. Before his followup appointment, he had three more days of abdominal pain and bloody stools. He was admitted with ultrasound and air contrast enema again demonstrating a left lower quadrant intussusception with questionable colonic filling defect. The intussusception was again reduced and the patient was taken to the operating room for open diagnostic laparotomy. A mass was palpated in the transverse colon and segmental colectomy was performed. Two large intraluminal pedunculated polyps (measuring 3.3 × 2.5 × 2.0 cm and 2.2 × 2.0 × 1.0 cm) and one small polyp were identified on the mesenteric side of the bowel (Fig 4). Pathologic examination revealed these to be juvenile polyps without atypia. The patient recovered well from surgery and has had no further episodes of intussusception. Colonoscopy was scheduled to evaluate for other polypoid lesions.
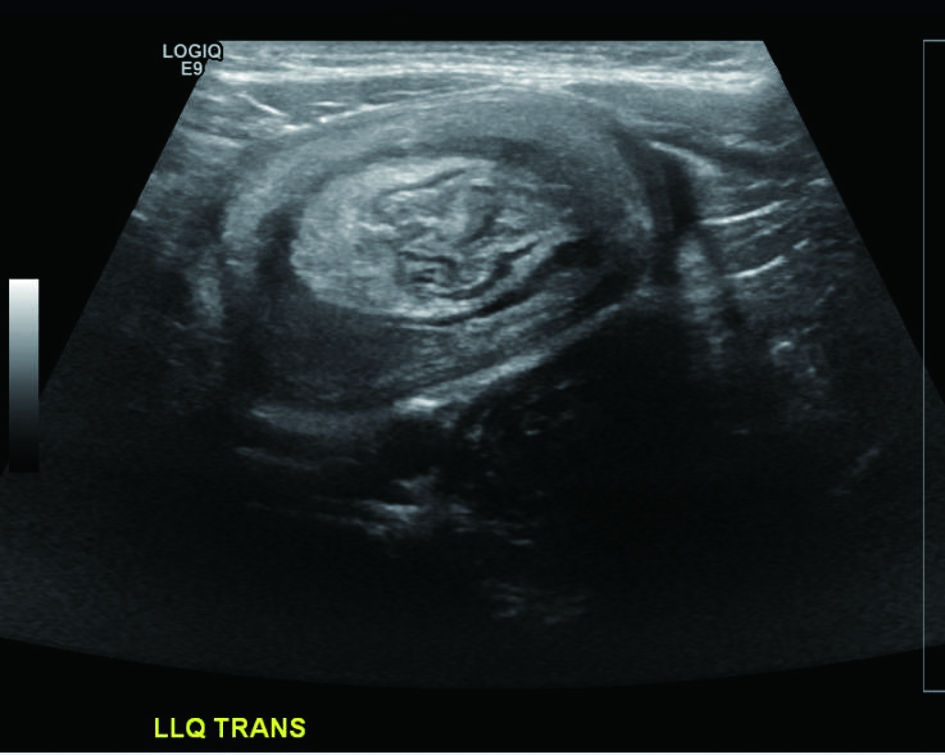 Click for large image | Figure 1. Transverse ultrasound image of the left lower quadrant demonstrates a mass with a “target” sign. |
 Click for large image | Figure 2. Air enema demonstrates a filling defect in the descending colon surrounded by a crescent of air representing the intussusceptum. Real time images demonstrated retrograde movement of the filling defect as the intussusception was reduced. |
 Click for large image | Figure 3. Single contract enema again shows a filling defect in the colon, representing the intussusceptum. |
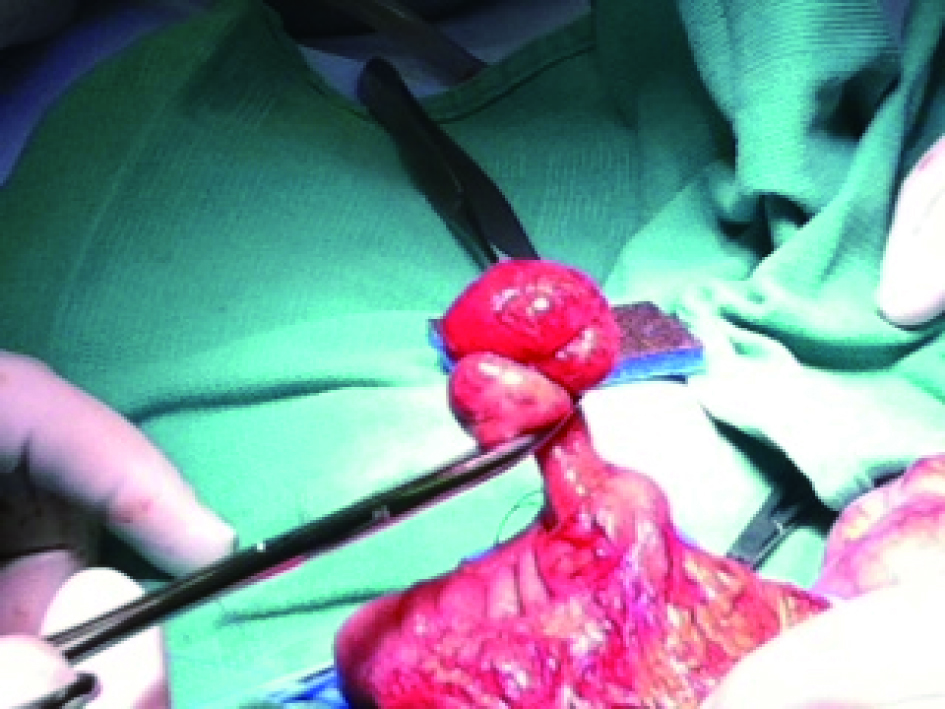 Click for large image | Figure 4. Pedunculated juvenile polyp is isolated from the mesenteric side of the transverse colon mucosa for surgical excision. |
| Discussion | ▴Top |
Intussusception is one of the most common causes of acute abdominal pain in infancy [1-3]. Intussusception results from invagination of a segment of bowel wall that is pulled into its lumen and becomes telescoped into adjacent bowel segment at times far from the starting point (Fig. 5). The condition usually occurs between the age of 6 months and 2 years [1]. The vast majority of intussusceptions in children are ileo-colic, meaning the ileum becomes telescoped into the colon. If correctly diagnosed and treated, the majority of patients have a very good prognosis.
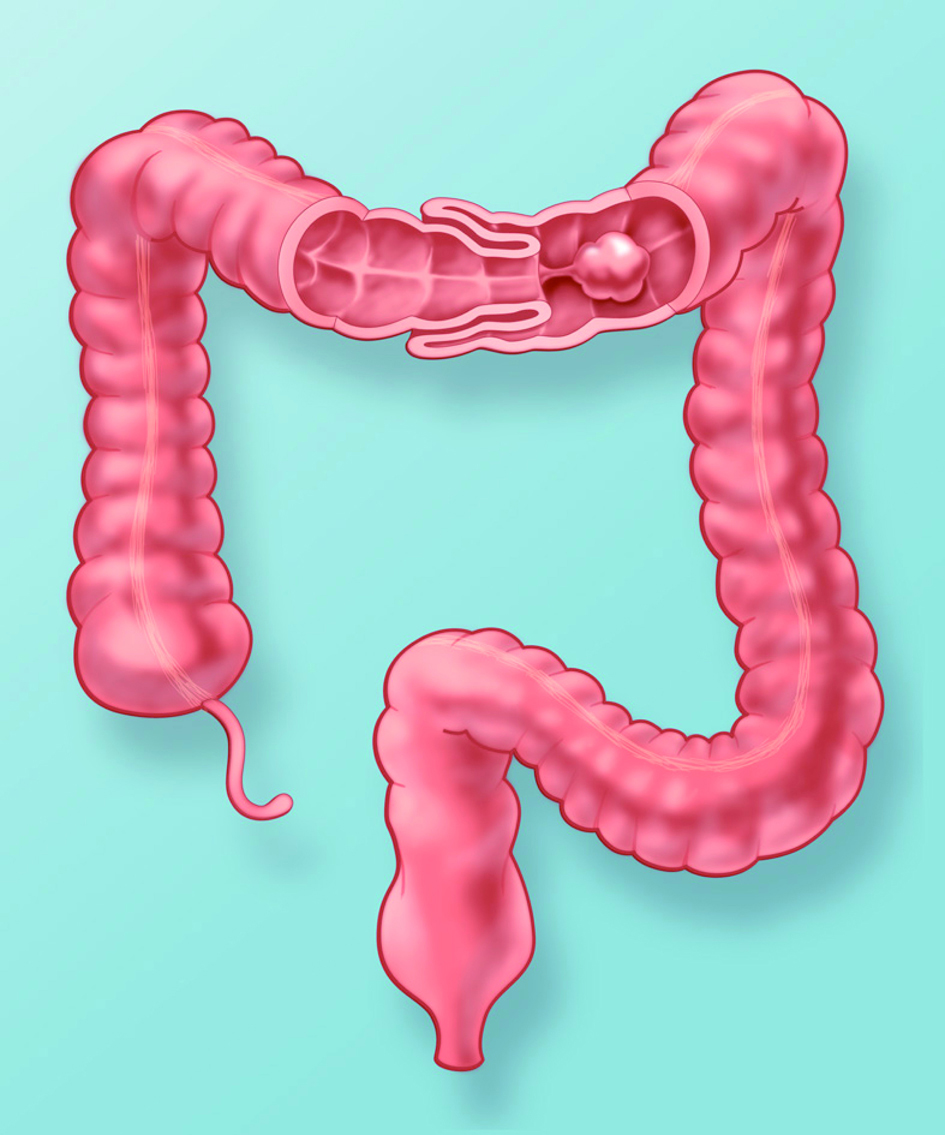 Click for large image | Figure 5. Artist’s rendering of the colon with coronal window through the transverse colon demonstrates intussusception secondary to a pedunculated polyp. Peristalsis pulls the large polyp distally, dragging the attached bowel wall into the intussuscipient. |
The classic clinical triad of acute abdominal pain (colic), currant-jelly stools or hematochezia, and a palpable abdominal mass is present in less than 50% of children with intussusception [4]. The onset of nonspecific abdominal symptoms in which vomiting predominates, the absence of passage of blood via the rectum (usually in cases of less than 48 hours duration), and the inability to obtain a reliable history from these nonverbal children lead to dismissal of the diagnosis of intussusception in almost 50% of cases [5]. In some cases lethargy and convulsions predominate [6].
The majority of pediatric intussusceptions are idiopathic without pathologic lead point [1, 7]. Intussusception lead points such as a Meckel diverticulum, duplication cyst, polyp, or tumor (eg, lymphoma) are uncommon in infants. Intussusception lead points are more common in neonates (< 30 days old), older children (> 5 years old), and cases restricted to the small intestine. Colocolic intussusception in the adults is almost always a complication of pre-existing colonic disease, usually carcinoma or polypoid tumor [8]. Pediatric patients presenting with documented colocolic intussusception should suggest the possibility of a colonic polyp or other mass lesion [9]. RotaShield, the first generation rotavirus vaccine, was shown to cause a transient risk of intussusception and was therefore withdrawn from the market [10]. The possible risk of intussusception in second generation vaccines is under debate.
Studies on the absolute prevalence of intussusception in the United States are not available [11]. Its estimated incidence is approximately 1 case per 2000 live births. In Great Britain, incidence varies from 1.6 - 4 cases per 1000 live births. Overall, the male-to-female ratio is approximately 3:1. With advancing age, gender differences become marked; in patients older than 4 years, the male-to-female ratio is 8:1. The studies of prevalence of the disease refer to ileocecal intussusception, which is the most common type. Colocolic intussusception is very rare in the pediatric population and there are no studies to document the exact prevalence of the disease. A rare occurrence of colocolic intussusception in a neonate with malrotated intestine was reported, that was believed to the first reported case in the neonatal period where the pathogenic lead point was an intestinal lymphangioma [12]. Juvenile colonic polyps have been reported to cause colocolic intussusception [13]. Colocolic intussusception has also been reported without anatomic lead point [9, 14]. In a study performed to compare ileocolic to colocolic intussusception it was found that in the colocolic group, there were fewer shocked and pyrexial patients, and the rate of successful nonoperative reduction was higher [15]. The groups had a similar incidence of surgical intervention. In the ileocolic group, there was a higher mortality rate and more complications, but only the higher resection rate was statistically significant.
Abdominal radiography is the most common initial study used in the workup of adbominal pain and suspected intussusception. Abdominal radiographs have low sensitivity and specificity for the diagnosis of intussusception, although they are useful in demonstrating other causes of abdominal pain and excluding free intraperitoneal air when enema is planned [16]. The addition of decubitus view increases the ability to diagnose or exclude intussusception and free air [17]. However, a quarter of intussusception cases will have a normal abdominal radiograph [18]. The meniscus sign is specific in plain abdominal radiographs for the diagnosis of intussusception. The meniscus sign is formed by the interface of the soft tissue density intussusceptum with air adjacent to its convexity in the intussuscepient. Although this sign is very specific it is not always seen. When the meniscus sign is seen the patient can go directly for fluoroscopic enema either with air or water-soluble contrast for confirmation of the diagnosis and reduction. At times opacity in the right lower quadrant of the abdomen without presence of bowel gas in frontal and left lateral views radiographs increases the suspicion for the diagnosis. In all other cases the abdominal radiograph is nonspecific. If free air is identified on the initial radiograph, the next step is surgical management and enema is contraindicated.
Ultrasonography is a well established imaging modality for the diagnosis of intussusception [19]. Not only is ultrasound sensitive and specific in the diagnosis of intussusception, it also does not expose the patient to ionizing radiation. Pathologic lead points can also be identified [20]. Sonographically a bull’s eye or target-like lesion on transverse views is the most frequently described appearances of intussusception (Fig. 6). This appearance is formed by a loop of bowel (intissusceptum) within another loop of bowel (intussuscepient). The target sign is also seen on radiographs when the involved bowel is viewed en face [21]. On ultrasound, the wall of the intussusceptum and the intussuscpient has the sonographic characteristics of bowl wall with multiple interfaces of mucosal and serosal layers. Echogenic layer surrounds the intussusceptum that corresponds to mesenteric fat. Longitudinal view of the affected bowel segment resembles the appearance of a kidney called pseudo-kidney. Ultrasound has a high sensitivity and specificity for intussusception and has been shown to be a reliable and inexpensive imaging modality in developing countries [22].
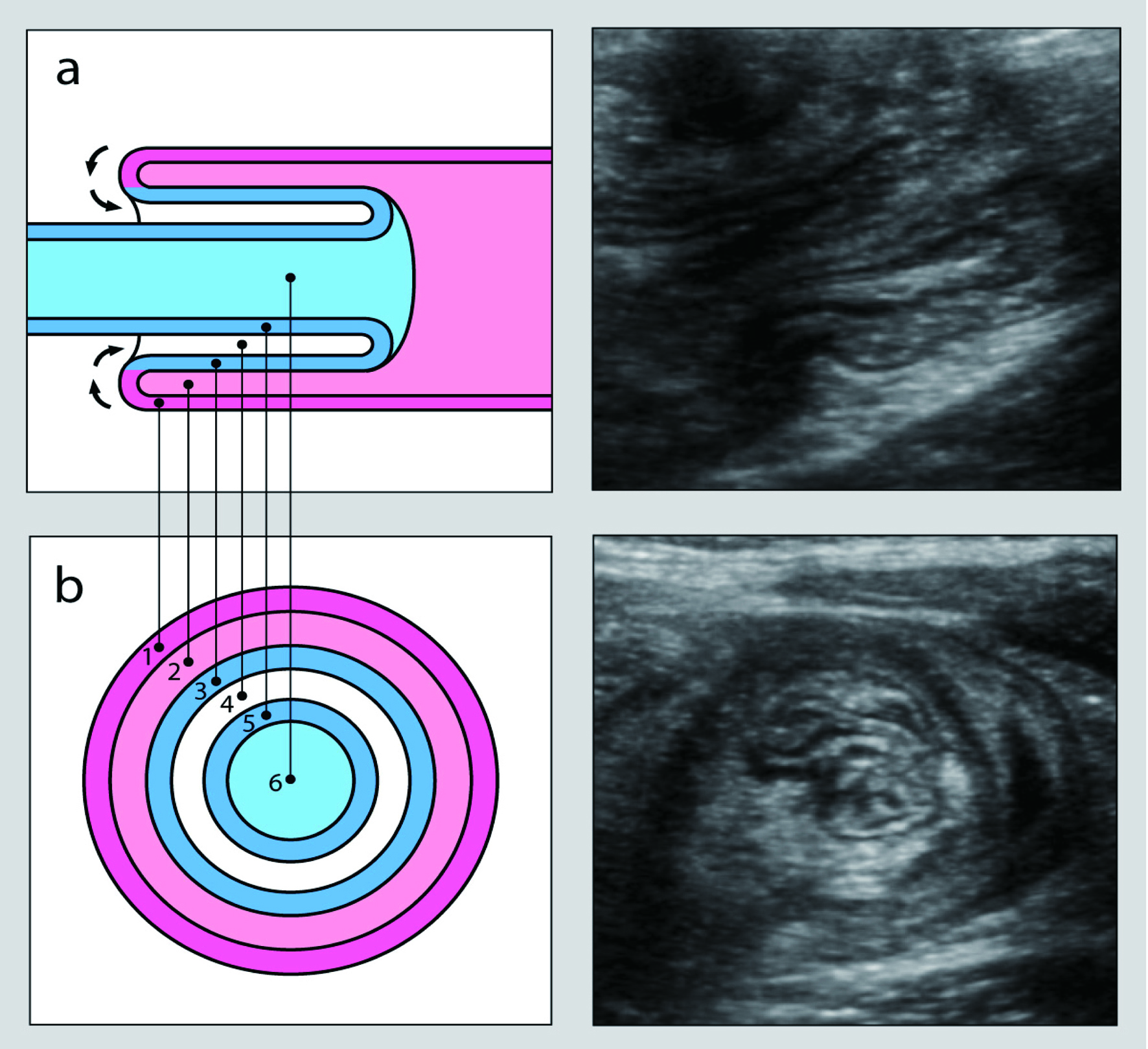 Click for large image | Figure 6. Longitudinal (a) and transverse (b) cross-sectional views of an intussusception. Images on the left graphically represent the intussusception complex while corresponding ultrasound images are depicted on the right. The outer layers represent the intussuscepient while the inner layers represent the intussusceptum. The bowel wall (1) and lumen (2) of the intussuscepient make up the outer rings. The inner rings are comprised of the bowel wall (3 and 5) and lumen (6) of the intussusceptum surrounded by mesenteric fat (4). In vivo, the lumen is collapsed and the echogenic rings on ultrasound represent interfaces between the mucosa, submucosa, muscularis, and serosa. |
The first step in management of intussusception is air or contrast enema guided with either fluoroscopy or ultrasound. Ultrasound guided reduction is typically performed with saline, although air has also been used. The reducibility, recurrence rate, recurrence pattern, and long term outcomes of intussusception has been shown to be similar between air and contrast enemas [23]. There is conflicting evidence regarding the complication rate between air and contrast enemas with the risk of perforation more closely related to the applied pressure and degree of pressure fluctuation [1, 24]. If fluoroscopic contrast enema is performed, water soluble contrast is preferred over barium due to the risk of barium peritonitis [1].
| References | ▴Top |
- del-Pozo G, Albillos JC, Tejedor D, Calero R, Rasero M, de-la-Calle U, Lopez-Pacheco U. Intussusception in children: current concepts in diagnosis and enema reduction. Radiographics. 1999;19(2):299-319.
pubmed - Tseng YC, Lee MS, Chang YJ, Wu HP. Acute abdomen in pediatric patients admitted to the pediatric emergency department. Pediatr Neonatol. 2008;49(4):126-134.
pubmed doi - Carty HM. Paediatric emergencies: non-traumatic abdominal emergencies. Eur Radiol. 2002;12(12):2835-2848.
pubmed - Daneman A, Alton DJ. Intussusception. Issues and controversies related to diagnosis and reduction. Radiol Clin North Am. 1996;34(4):743-756.
pubmed - Beasley SW, Auldist AW, Stokes KB. The diagnostically difficult intussusception: its characteristics and consequences. Pediatr Surg Int 1988; 3:135-138.
- Stringer MD, Pablot SM, Brereton RJ. Paediatric intussusception. Br J Surg. 1992;79(9):867-876.
pubmed doi - Eklof OA, Johanson L, Lohr G. Childhood intussusception: hydrostatic reducibility and incidence of leading points in different age groups. Pediatr Radiol. 1980;10(2):83-86.
pubmed doi - Figiel LS, Figiel SJ. Colocolic Intussusception. Am J Dig Dis. 1963;8:1017-1028.
pubmed - Mahmudloo R, Gheibi S, Vahed SN. Colocolic Intussusception without Lead Point; A Case Report and Literature Review. Iran J Pediatr 2008;18(4)373-376.
- Murphy TV, Gargiullo PM, Massoudi MS, Nelson DB, Jumaan AO, Okoro CA, Zanardi LR, et al. Intussusception among infants given an oral rotavirus vaccine. N Engl J Med. 2001;344(8):564-572.
pubmed doi - Blanco FC, Cuffari C. Intussusception. http://emedicine.medscape.com/article/930708-overview#a0156.
- Al-Jahdali A, Lees GM, Gay DP, Al-Sairafi R. Colocolic intussusception in a preterm infant with intestinal malrotation. J Pediatr Surg. 2009;44(12):e17-18.
pubmed doi - Arthur AL, Garvey R, Vaness DG. Colocolic intussusception in a three-year-old child caused by a colonic polyp. Conn Med. 1990;54(9):492-494.
pubmed - Sanchez S, Javid P, Ricca R, Avansino J. Colocolonic intussusception in a four-yr-old with a heart transplant: A case report and review of the literature. Pediatr Transplant. 2011.
pubmed - Grant HW, Buccimazza I, Hadley GP. A comparison of colo-colic and ileo-colic intussusception. J Pediatr Surg. 1996;31(12):1607-1610.
pubmed doi - Morrison J, Lucas N, Gravel J. The role of abdominal radiography in the diagnosis of intussusception when interpreted by pediatric emergency physicians. J Pediatr. 2009;155(4):556-559.
pubmed doi - Hooker RL, Hernanz-Schulman M, Yu C, Kan JH. Radiographic evaluation of intussusception: utility of left-side-down decubitus view. Radiology. 2008;248(3):987-994.
pubmed doi - Hernandez JA, Swischuk LE, Angel CA. Validity of plain films in intussusception. Emerg Radiol. 2004;10(6):323-326.
pubmed - Bowerman RA, Silver TM, Jaffe MH. Real-time ultrasound diagnosis of intussusception in children. Radiology. 1982;143(2):527-529.
pubmed - Navarro O, Dugougeat F, Kornecki A, Shuckett B, Alton DJ, Daneman A. The impact of imaging in the management of intussusception owing to pathologic lead points in children. A review of 43 cases. Pediatr Radiol. 2000;30(9):594-603.
pubmed doi - Ratcliffe JF, Fong S, Cheong I, O'Connell P. Plain film diagnosis of intussusception: prevalence of the target sign. AJR Am J Roentgenol. 1992;158(3):619-621.
pubmed - Justice FA, de Campo M, Liem NT, Son TN, Ninh TP, Bines JE. Accuracy of ultrasonography for the diagnosis of intussusception in infants in Vietnam. Pediatr Radiol. 2007;37(2):195-199.
pubmed doi - Daneman A, Alton DJ, Lobo E, Gravett J, Kim P, Ein SH. Patterns of recurrence of intussusception in children: a 17-year review. Pediatr Radiol. 1998;28(12):913-919.
pubmed doi - Hadidi AT, El Shal N. Childhood intussusception: a comparative study of nonsurgical management. J Pediatr Surg. 1999;34(2):304-307.
pubmed doi
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


