| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 13, Number 8, August 2022, pages 391-395
Unusual Case of Non-HIV Patient With Multifocal Pyomyositis: Developed on Appropriate Antibiotic Therapy
Elisa Akagia, Ashish Bhargavab, c
aDivision of Infectious Disease, Providence Medford Medical Center, Medford, OR 97504, USA
bDivision of Infectious Disease, Department of Internal Medicine, Ascension St. John Hospital, Detroit, MI 48236, USA
cCorresponding Author: Ashish Bhargava, Division of Infectious Disease, Department of Internal Medicine, Ascension St. John Hospital, Detroit, MI 48236, USA
Manuscript submitted June 8, 2022, accepted July 23, 2022, published online August 19, 2022
Short title: A Case of Multifocal Pyomyositis
doi: https://doi.org/10.14740/jmc3967
| Abstract | ▴Top |
Pyomyositis is a clinical condition classically associated with tropical climates, but there are an increasing number of reports in temperate climates. We present a diabetic patient, who presented with gastrointestinal symptoms and right foot ulcer. He was found to have methicillin-resistant Staphylococcus aureus (MRSA). Initial computed tomography (CT) scan of abdomen and pelvis was negative for any abscesses, but after persistent bacteremia developed pyomyositis being on appropriate antibiotic therapy. This case may make physicians aware that initial negative test results do not always preclude the presence of pyomyositis in the presence of risk factors.
Keywords: Pyomyositis; MRSA pyomyositis; Pyomyositis in diabetes; Multifocal myositis
| Introduction | ▴Top |
Pyomyositis is a rare clinical condition in temperate climates, characterized by primary intramuscular abscess. It was classically described in tropical settings, but it has been increasingly recognized in temperate climates [1]. Staphylococcus aureus is the commonest organism involved [2]. In the early stage of the presentation, the diagnosis can be missed due to unawareness of the condition, and non-specific clinical presentation. In the United States, bacterial pyomyositis is increasingly reported, especially among human immunodeficiency virus (HIV)-infected patients [3, 4]. Usually the presentation described in literature is unifocal in the majority of patients (81%) [4]. We present an unusual case of multifocal pyomyositis in a male with diabetes mellitus, who presented with bacteremia and no evidence of pyomyositis on admission.
| Case Report | ▴Top |
Investigations
A 63-year-old male was admitted to the hospital with complaints of nausea, vomiting, abdominal pain, and diarrhea of 5 days duration. He had multiple comorbidities including previously treated hepatitis C, cirrhosis, hypertension, hyperlipidemia, and diabetes mellitus. Patient’s HIV status was negative. Six months prior to the current admission, he presented with abdominal pain, diarrhea, fever, and a non-healing right foot ulcer. At that time, he underwent esophagogastroduodenoscopy (EGD), and was found to have small epigastric varices. Due to a non-healing ulcer with erythema, edema and pain concerning for infection, a magnetic resonance imaging (MRI) of the foot was done. The imaging study reported cellulitis, myositis, and tenosynovitis. The patient underwent incision and drainage, as well as a first metatarsal head bone biopsy to rule out osteomyelitis. The culture from the incision and drainage grew methicillin-resistant Staphylococcus aureus (MRSA), but bone biopsy remained negative. Given there was still a high suspicion of osteomyelitis, intravenous (IV) vancomycin therapy was started with a plan to complete 6 weeks of therapy. One month prior to the current admission, the patient presented again to an outside hospital with epigastric abdominal pain, vomiting, and diarrhea. Another EGD revealed erosive esophagitis and gastritis. Testing for Clostridioides difficile (C. difficile) was performed and found to be positive. Oral vancomycin was started with a plan to finish 14 days of therapy. Five days prior to the current evaluation, the patient started to experience epigastric pain. Three days prior, coffee-ground emesis was noted, along with episodes of watery diarrhea. Due to progressive worsening of abdominal pain and vomiting, the patient decided to call the ambulance.
Diagnosis
Upon admission, the patient was tachycardic with a heart rate of 133/min, and slightly elevated temperature of 37.6 °C. He was alert and oriented, not in acute distress, with some epigastric tenderness without rebound tenderness. There was right plantar foot ulceration of 4 × 6 cm with small purulent drainage and a tunnelling sinus which did not probe to bone. The workup revealed leukocytosis (white blood cells (WBCs) 22.90 × 103/mm3), mild anemia (hemoglobin (Hb) 12.9 g/dL), hyperglycemia (519 mg/dL), and HbA1c of 12.4%. Creatinine was within normal range (1.39 mg/dL), bicarbonate level decreased (17 mmol/L), aspartate aminotransferase (AST) slightly elevated (62 IU/L), normal alanine aminotransferase (ALT) (44 IU/L), total bilirubin (0.7 mg/dL), and normal lipase (5 IU/L) (Table 1). Computed tomography (CT) scan of the abdomen and pelvis with IV contrast (Fig. 1a) was done as the patient presented with coffee-ground emesis and epigastric pain, but no extravasation of the contrast from the vasculature was seen. There was no intra abdominal collection, or intramuscular fluid collection noted in this study.
 Click to view | Table 1. Clinical Laboratory Results |
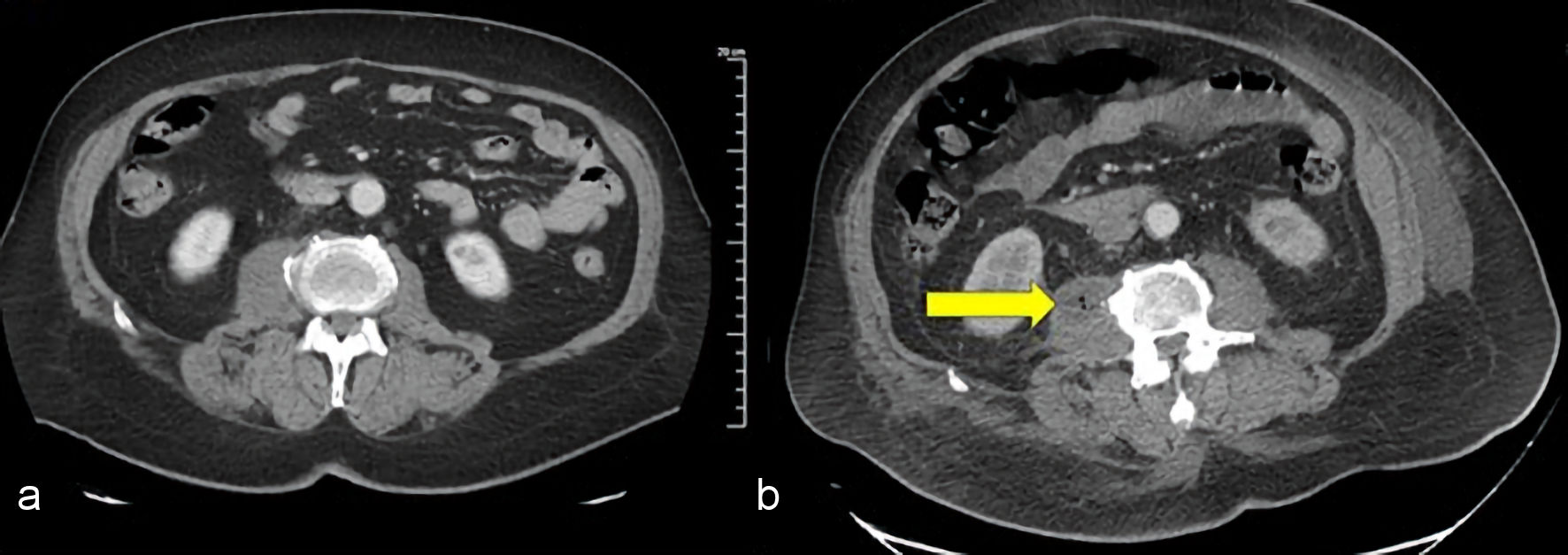 Click for large image | Figure 1. CT scan of the abdomen and pelvis with IV contrast: (a) On admission, no abscess was found; (b) At 10th day of admission, right psoas abscess (arrow) was observed. CT: computed tomography; IV: intravenous. |
Further imaging with MRI of the abdomen and pelvis were not done as the abdominal CT scan did not reveal any abscess or muscle involvement. Given leukocytosis and tachycardia with recurrence of diarrhea and purulence from the right foot, infectious disease was consulted for further evaluation and treatment. Upon evaluation by the infectious disease on the next day of admission, the vomiting and diarrhea was already subsiding. Attention was directed to the right foot, and infectious disease recommended treatment with IV vancomycin (target trough levels: 15 - 20 mcg/L) and to consult podiatry. Podiatry drained the abscess from the right foot, and the fluid sample was sent for aerobic and anaerobic cultures. Two sets of blood cultures were also collected before the start of antibiotic therapy. On the next day, both sets of blood cultures turned positive for MRSA, and sensitivity showed minimal inhibitory concentration (MIC) of 1.5 mg/mL for vancomycin. Transthoracic echocardiogram was done to rule out endocarditis in a setting of high-grade bacteremia, followed by transesophageal echocardiogram for persistence of bacteremia, with both studies negative for vegetation. The patient continued to receive vancomycin with trough levels within the therapeutic range, but the blood cultures were persistently positive. Persistent bacteremia led to the second CT scan of chest, abdomen and pelvis searching for occult source of infection. It was done on the 10th day of admission. This time, there were foci of air and abscesses on two different sites. The first was left pectoralis major muscle (Fig. 2), and the second, a big right psoas abscess measuring 8 × 3 × 2.4 cm (Fig. 1b).
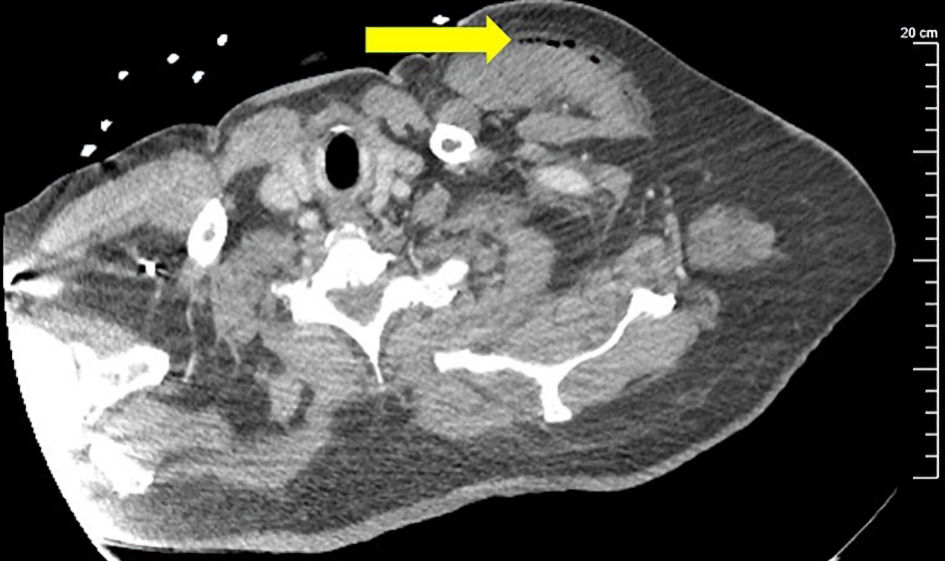 Click for large image | Figure 2. CT scan of chest with IV contrast revealed the abscess on the left pectoral major muscle (arrow). CT: computed tomography; IV: intravenous. |
The focus for pectoralis muscle was small and it was not considered a target for the drainage. The right psoas abscess on the other hand was aspirated under CT guidance and 20 mL of purulent fluid mixed with blood was removed, and a drain was left in place. After drainage of the abscess, one more set of blood cultures turned positive, but two subsequent blood cultures on different days remained negative. Around the same time the second CT scan was performed, the patient complained about worsening of chronic back pain without other new neurological findings on physical exam. MRI of cervical, thoracic, and lumbar spine with contrast was performed to rule out paraspinal processes. Bone marrow of the L1 and L2 vertebral bodies showed enhancement, concerning for osteomyelitis without any abscess or phlegmon (Fig. 3).
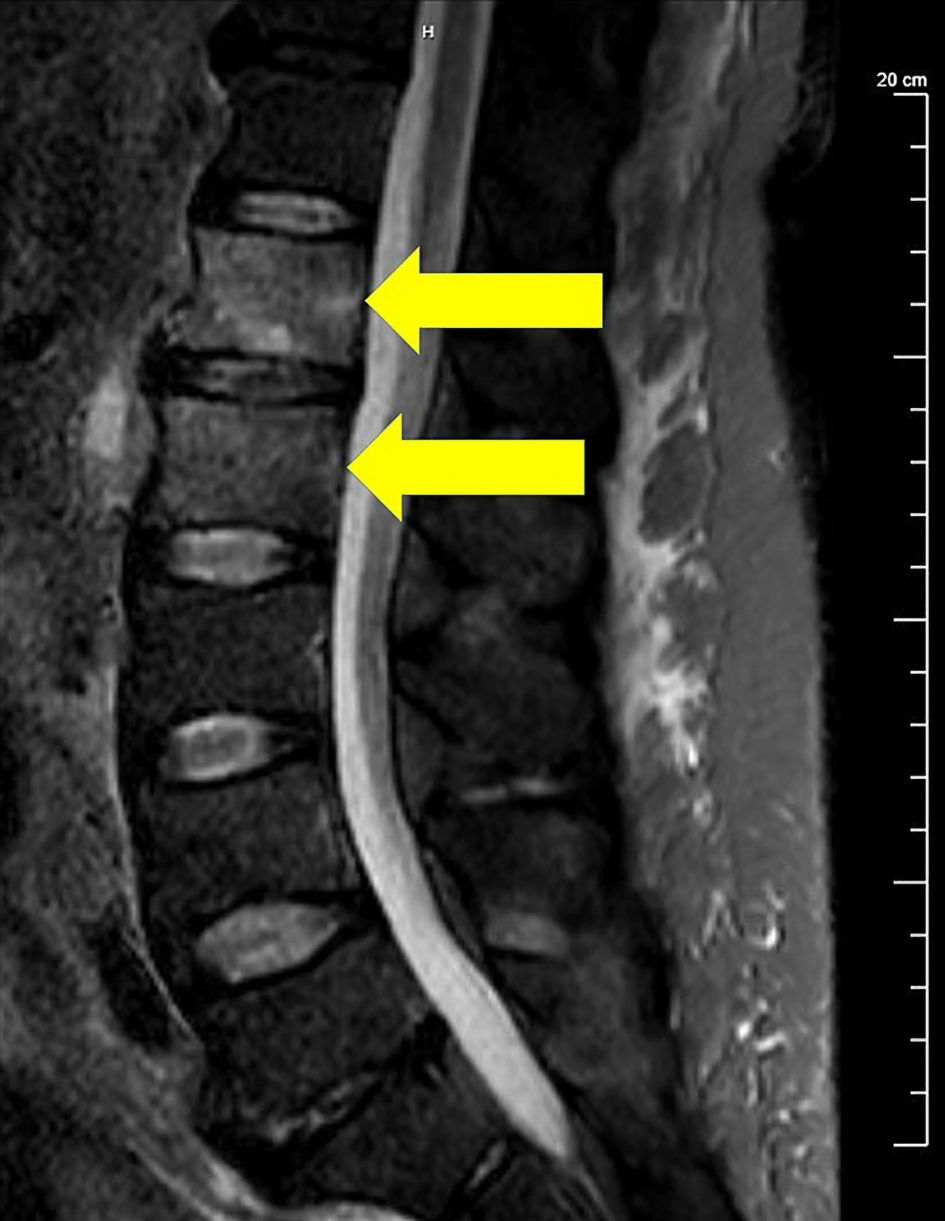 Click for large image | Figure 3. T2-weighted fat suppression image of lumbar spine MRI showed marrow edema involving L1 and L2 vertebral bodies suggesting osteomyelitis (arrows). Clinically, there were no signs of cord compression. MRI: magnetic resonance imaging. |
Treatment
Neurosurgery was consulted, but no further surgical treatment was required. On day 23 of admission, serum creatinine increased to 5.23 from normal baseline creatinine level. The antibiotic was switched from vancomycin to daptomycin (10 mg/kg/day) with a plan to complete at least 6 weeks of therapy from the time of negative blood culture. The patient was advised at the time of hospital discharge to follow up at the infectious disease clinic.
Follow-up and outcomes
The patient was lost to follow up, but no further hospitalizations were recorded in our medical records.
| Discussion | ▴Top |
Pyomyositis is a common disease in tropical countries through several continents, including Asia, Africa, Oceania, and part of the American Caribbean Islands [1]. It accounts for up to 4% of hospitalizations in a country with a high prevalence such as Uganda [5]. Other commonly used names for this condition are tropical pyomyositis and myositis tropicans, due to the geographical distribution in warmer climates. The incidence is increasing in temperate climates as in the United States, especially among immunocompromised patients. In a study which included over 100 million discharges in the United States between 2002 and 2014 [4], a little more than 13,000 cases of pyomyositis were reported. The rate of discharges with diagnosis of pyomyositis has been increasing over the years, from 0.0054% in 2002 to 0.0209% in 2014. Odds ratio of each risk factor was calculated in this study. The age-adjusted odds ratios of patients with HIV were 4.89 being the highest, followed by hematologic malignancy (2.42), and type 1, type 2 diabetes mellitus (2.37 and 2.04 respectively). Other conditions listed as risk factors were organ transplant, malnutrition, chronic kidney disease, and rheumatoid arthritis. Though the pathophysiology is not fully explained, there are case reports of cirrhosis and even hepatitis C, both of which impair the immunity, associated with pyomyositis [6-9]. Interestingly, obesity also demonstrated to increase the risk, with morbid obesity being higher risk (1.47) than obesity (1.34). The most frequently recovered organism is Staphylococcus aureus, which can have variable rates according to geographical regions. In a recent study from the United States, the frequency reported for methicillin-sensitive Staphylococcus aureus (MSSA) was 46%, and for MRSA was 20% [2, 3]. Affected areas are typically unifocal, but in fewer cases can be multifocal, as in our case. In a report comparing North America and Nigeria, multiple muscles were affected in 12% in North America, compared with 43% in Nigeria [2].
The pathogenesis of pyomyositis is not well understood. It is theorized that for immunocompetent patients, the initiating event may be a transient bacteremia and seeding [3], especially in traumatized muscles, as there is a report that 20-50% of cases have a history of muscle injury prior to the infectious process [1]. Recently, a very interesting association was found between the Panton-Valentine Leukocidin (PVL) and pyomyositis. Although there are several cytotoxins produced by Staphylococcus aureus, the isolates with PVL were strongly associated with pyomyositis (OR > 55) [8, 9]. There are muscle groups which are more commonly involved, such as gluteus, quadriceps, iliopsoas, gastrocnemius, pectoralis major, serratus anterior, biceps, abdominal and spinal muscles [1]. The process can go from invasive to suppurative stages to stages of complications [2]. Locally, severe edema can compress adjoining structures and cause compartment syndrome, or when becomes more severe, produce septicemia and seeding of other non-muscular structures.
Treatment should be aggressive with a combination of surgical debridement or image guided drainage, accompanied by an IV anti-staphylococcal antibiotic as initial treatment [3]. Our patient received vancomycin initially for treatment of MRSA but developed acute kidney injury and required switching of the treatment to daptomycin. A recently published retrospective study included cases of pyomyositis treated with daptomycin [10]. The overall success rate was 84%, but the breakdown of outcomes according to each antimicrobial therapy was not reported. A case of pyomyositis reported successful treatment with daptomycin [11], but as in our case, the initial treatment was vancomycin and it was switched to daptomycin for suspected drug fever. Also, the gram stain of the sample from the surgical site was positive for gram positive cocci, but the culture did not have any growth, and the nasal screen for MRSA was negative.
In our case, the patient had a prolonged period of bacteremia and developed pyomyositis despite initial appropriate therapy. The patient had several conditions known to impact the immune system negatively, including diabetes mellitus, cirrhosis, and hepatitis C [6, 7, 9]. Both cirrhosis and hepatitis C affect the innate and adaptive immune response [12, 13]. Hyperglycemia in diabetes mellitus is believed to cause dysfunction of the immune response, failing to control the infection. We theorized that our patient was not able to control the initial bacteremia due to hyperglycemia, even with appropriate antibiotic therapy, which led to the formation of abscesses. This case may make physicians aware that an initial negative imaging study does not preclude the presence of pyomyositis, especially if the suspicion is high, and the patient has risk factors.
Learning points
Cases of pyomyositis are increasingly reported in temperate climates. Diagnosis can be challenging. Staphylococcus aureus is the commonest cause. In patients with risk factors for developing the infection, along with continuous high suspicion, may require clinicians to reconsider the diagnosis even after initial negative workup. Treatment should be aggressive, with medical and surgical management removing the foci of infection. Educating the patient about the importance of being compliant with the medication and glycemic control, is probably an important measure for a successful therapy.
Acknowledgments
None to declare.
Financial Disclosure
There was no funding involved.
Conflict of Interest
There is no conflict of interest.
Informed Consent
Informed consent was obtained by the patient.
Author Contributions
EA contributed to the design of the work, the acquisition, interpretation, and initial drafts. AB contributed to designing and revising the manuscript critically for important intellectual content. Both authors gave final approval of the submitted version.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Chauhan S, Jain S, Varma S, Chauhan SS. Tropical pyomyositis (myositis tropicans): current perspective. Postgrad Med J. 2004;80(943):267-270.
doi pubmed - Christin L, Sarosi GA. Pyomyositis in North America: case reports and review. Clin Infect Dis. 1992;15(4):668-677.
doi pubmed - Crum NF. Bacterial pyomyositis in the United States. Am J Med. 2004;117(6):420-428.
doi pubmed - Maravelas R, Melgar TA, Vos D, Lima N, Sadarangani S. Pyomyositis in the United States 2002-2014. J Infect. 2020;80(5):497-503.
doi pubmed - Horn CV, Master S. Pyomyositis tropicans in Uganda. East Afr Med J. 1968;45(7):463-471.
- Polizelli DV, Geraldino GC, Narvaes E, Funes E, de Toledo RA, Menin Rde C. Pyomyositis associated with diabetes mellitus and liver cirrhosis. Rev Bras Reumatol. 2010;50(4):472-477.
doi pubmed - Revuelto-Artigas T, Cabrerizo-Garcia JL, Domene-Moros R, Sanjoaquin-Conde I. [Cellulitis, pyomyositis, and sternoclavicular arthritis due to Streptococcus agalactiae in a patient with liver cirrhosis]. Gastroenterol Hepatol. 2011;34(1):53-54.
doi pubmed - Shittu A, Deinhardt-Emmer S, Vas Nunes J, Niemann S, Grobusch MP, Schaumburg F. Tropical pyomyositis: an update. Trop Med Int Health. 2020;25(6):660-665.
doi pubmed - Radcliffe C, Gisriel S, Niu YS, Peaper D, Delgado S, Grant M. Pyomyositis and infectious myositis: a comprehensive, single-center retrospective study. Open Forum Infect Dis. 2021;8(4):ofab098.
doi pubmed - Tan EM, Marcelin JR, Sohail R, Ramar K. Necrotising pyomyositis complicating intramuscular antipsychotic administration. BMJ Case Rep. 2015;2015:bcr2015210017.
doi pubmed - Berbudi A, Rahmadika N, Tjahjadi AI, Ruslami R. Type 2 diabetes and its impact on the immune system. Curr Diabetes Rev. 2020;16(5):442-449.
doi pubmed - Noor MT, Manoria P. Immune dysfunction in cirrhosis. J Clin Transl Hepatol. 2017;5(1):50-58.
doi pubmed - Urbanowicz A, Zagozdzon R, Ciszek M. Modulation of the immune system in chronic hepatitis C and during antiviral interferon-free therapy. Arch Immunol Ther Exp (Warsz). 2019;67(2):79-88.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


