| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 12, Number 9, September 2021, pages 347-350
Unique Communication: A Case Report of Acquired Esophageal Pulmonary Fistula
Ruhma Alia, d, Aditya Patela, d, Muhammad Hussaina, Theodore DaCostab, Yatinder Bainsb, Richard Millerc
aDepartment of Internal Medicine, Saint Michael’s Medical Center, Newark, NJ, USA
bDepartment of Gastroenterology, Saint Michael’s Medical Center, Newark, NJ, USA
cDepartment of Pulmonology, Saint Michael’s Medical Center, Newark, NJ, USA
dCorresponding Author: Ruhma Ali and Aditya Patel, Department of Internal Medicine, Saint Michael’s Medical Center, Newark, NJ 07102, USAand
Manuscript submitted July 11, 2021, accepted July 24, 2021, published online August 25, 2021
Short title: A Case of Acquired Esophageal Pulmonary Fistula
doi: https://doi.org/10.14740/jmc3746
| Abstract | ▴Top |
Esophageal respiratory fistula represents a connection between esophagus and the respiratory system. Esophageal tracheal and esophageal bronchial fistulas are common whereas esophageal pulmonary fistula is rarely seen. We report a case of esophageal pulmonary fistula in a middle aged African American male with a history of bronchoesophageal fistula who presented with pneumonia. The diagnosis was confirmed with fluoroscopy esophagram. Management with endoscopic stent placement was planned however the patient refused treatment. A diagnosis of esophageal pulmonary fistula should be kept in mind for patients with pulmonary symptoms and dysphagia. Early diagnosis and treatment are required to prevent complications and improve quality of life in these patients.
Keywords: Esophageal pulmonary fistula; Esophageal stent; Fluoroscopy esophagram; Antral gastrectomy
| Introduction | ▴Top |
Esophageal respiratory fistulas are abnormal communications between the esophagus and the respiratory system. Most common esophageal respiratory fistulas are esophageal tracheal (52-57%) and esophageal bronchial (37-40%), whereas esophageal pulmonary fistula consists of 3-11% of the cases [1]. Emergent therapeutic intervention is required since this uncommon pathology can lead to increase in morbidity and mortality because of nutritional debilitation, poor functional status and respiratory complications. Implantation of endoscopic stents is the preferred treatment of choice to improve the quality of life in these patients. We present a rare case of esophageal pulmonary fistula in a patient with a history of bronchoesophageal fistula treated with esophageal stent placement.
| Case Report | ▴Top |
Investigations
A 53-year-old homeless male with a history of smoking, alcoholism, substance abuse, gastroesophageal reflux disease (GERD), perforated peptic ulcer status post antrectomy with type II Billroth reconstruction (in 1997), pseudodiverticulum of the distal one-third of esophagus, bronchoesophageal fistula and human immunodeficiency virus (HIV) presented to the emergency department with dyspnea and productive cough for the past 2 weeks. The cough is productive of yellowish, non-bloody sputum that has worsened progressively. He reported dysphagia to liquids and unintentional weight loss without any appetite loss. He is unable to quantify the amount or duration of weight loss. He was recently hospitalized for empyema and was discharged on unknown antibiotics. He was incarcerated 6 months ago and states that he had a negative tuberculosis test recently. Review of medical records from other hospitals revealed that he was admitted for pneumonia 3 years ago and workup demonstrated bronchoesophageal fistula followed by stent (fully covered self-expandable metallic stent, 20 mm × 8 cm) placement endoscopically with removal after 2 months to reassess fistula. Computed tomography (CT) scan of chest after a few months showed resolution of fistula. On this admission, the patient was febrile, tachycardic, saturating 93% on room air. On physical examination, the patient appeared disheveled and malnourished. Decreased air entry was noted on the right side with crackles throughout the right lung. The rest of the physical examination was non-contributory.
Diagnosis
The white blood cells were elevated to 20.3 × 103/µL (reference value: 4.4 - 11 × 103/µL) with absolute neutrophils count of 18.2 × 103/µL (reference value: 1.7 - 7 × 103/µL) on admission. Chest X-ray was significant for right lower lobe opacification. CT chest without contrast showed debris filling the middle and lower esophagus, right pleural effusion with multiple areas of gas without direct evidence of esophageal pleural fistula. On thoracocentesis, the pleural fluid was serous but cloudy. The analysis confirmed exudative pleural fluid as per light’s criteria with lactate dehydrogenase (LDH) 986 U/L (reference value: 122 - 222 U/L), pH 7, WBC 8,375/mm3 with 88% neutrophils. Acid-fast bacilli (AFB) culture and smear were negative. CT chest with contrast showed irregular and debris distended esophagus with locules of air extending from the region of the esophagus into the mediastinum and right lower lung parenchyma. Fluoroscopy esophagram documented that the distal one-third of the esophagus is markedly dilated, irregular and contrast extravasation was seen from the right side of the distal esophagus into the right lower lobe parenchyma compatible with esophageal pulmonary fistula (Fig. 1). Contrast is also seen filling the right lower lobe bronchus which suggests possible reflux from the right lower lung parenchyma (Fig. 2).
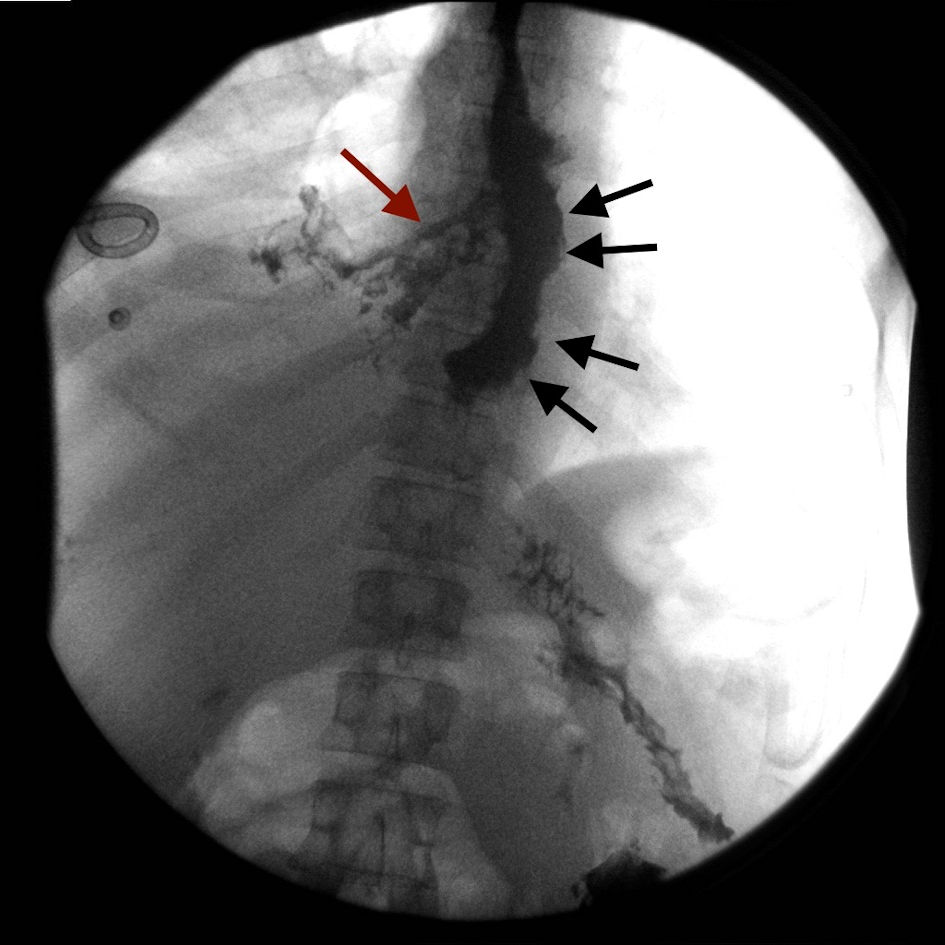 Click for large image | Figure 1. The distal one-third of esophagus is markedly dilated and irregular in contour (black arrows). Contrast is seen extravasating from the right side of the esophagus into the right lower lobe parenchyma consistent with esophageal pulmonary fistula (red arrow). |
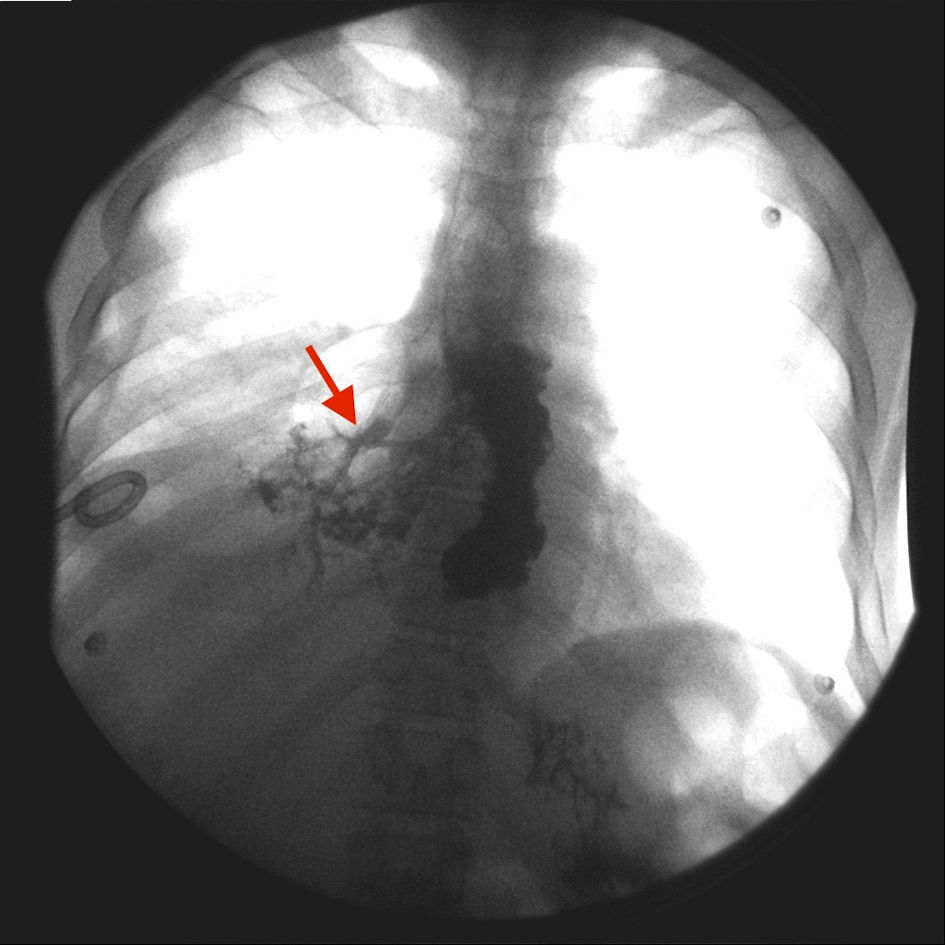 Click for large image | Figure 2. Contrast is seen filling the right lower lobe bronchus, which suggests possible reflux from the right lower lung parenchyma (red arrow). |
Treatment
Gastroenterology, pulmonology, infectious disease and surgery were consulted for the management of the patient. An esophageal stent placement was planned but was declined by the patient who then left against medical advice.
Follow-up and outcomes
The patient was informed to follow-up in gastroenterology clinic for further management. The patient was found to be admitted to another hospital for similar complaints, while trying to reach him for the follow-up appointment.
| Discussion | ▴Top |
Esophageal respiratory fistula can be congenital or acquired. Congenital fistulas arise from esophageal abnormalities in the fourth week of embryonic development and account for 0.04% of all live births. Congenital fistulas are usually associated with esophageal atresia at birth [2]. Acquired esophageal respiratory fistula can be due to malignant and non-malignant etiologies. The most common malignancies are esophageal and lung cancers. The pathophysiology behind malignancies causing esophageal respiratory fistula includes direct invasion of the tumor or as a side effect of the treatment modalities specifically radiotherapy. The use of antiangiogenic drugs such as bevacizumab has also been reported to cause esophageal respiratory fistula [2]. Non-malignant etiologies include postoperative, radiation induced, intubation associated, related to granulomatous disease including tuberculosis and histoplasmosis, history of tracheal and esophageal stents, blunt trauma, pseudodiverticulum of the esophagus, Crohn’s disease or foreign body ingestion [3, 4]. A review of Lenz et al [5] from 2001 to 2012 revealed five of the 58 patients with benign esophageal respiratory fistula to be from radiation, three from esophageal diverticula, one each related to caustic ingestion, broncholithiasis, tracheal stenosis and Actinomyces. In our case, etiologies of bronchoesophageal fistula and then esophageal pulmonary fistula were believed to be multifactorial, which includes esophagitis due to history of chronic GERD, history of antral gastrectomy, history of stent placement for a bronchoesophageal fistula and pseudodiverticulum of distal one-third of the esophagus. Nonetheless, nutritional insufficiency, history of alcoholism and smoking, lost to follow-up could also have played a significant role.
Most patients with aerodigestive fistula present with symptoms of intractable cough, dysphagia, weight loss, recurrent pneumonia or other respiratory complications [6]. The patients may give a history of primary disease causing esophageal pulmonary fistula including chest trauma, cachexia, intubation or recent travel. These patients will have a low functional status due to chronic inflammation and malnutrition. Our patient presented with complaints of recurrent episodes of pneumonia and empyema untreated with antibiotics due to lack of source control. Radiological imaging including CT scan and contrast-enhanced esophagography can be used to diagnose and localize the fistula [7]. Gastrografin is not recommended if the index of suspicion is high for esophageal respiratory fistula since it is hypertonic and can cause pulmonary edema, pneumonia, or death. Therefore, barium is preferred over Gastrografin and aspiration of small amounts of barium seems to have little clinical relevance. Bronchoscopy and esophageal endoscopy also play a role in diagnosis and treatment plan [2]. In this case a CT scan with and without contrast was done due to the suspicion of fistula and the diagnosis was confirmed with fluoroscopy esophagram, which showed that the esophageal fistula communicated directly with the right lower lobe parenchyma. If left untreated the quality of life is severely affected and most people die of respiratory complications and poor nutritional status. The goals of treatment for successful fistula management are treatment of pulmonary sepsis, prevention of complications like aspiration pneumonia [2] and to improve the nutritional status and performance score. Treatment modalities include endoscopic stenting and/or surgical repair and pulmonary support rehabilitation. Non-surgical management is associated with a mortality rate of 100% whereas mortality rate becomes 50% with surgical approach [8]. Operative closure can be considered for larger fistulas and better prognosis [5]. Direct closure of the fistula, surgical resection and esophageal bypass can be employed as surgical options. An esophageal stent can be placed for treatment and symptomatic relief as was planned in our patient. The purpose of the stent is to create a seal between the lumen of the esophagus and the airway to prevent bronchial contamination. A covered self-expanding metallic stent is typically preferred over plastic prosthesis to seal the fistula since the plastic prosthesis is associated with complications such as perforation, hemorrhage, tube migration, tube dislodgement and tube necrosis. Close surveillance is required to monitor the clinical condition after stent placement to prevent complications. After stent placement, an esophagram should be obtained to confirm the sealing of the fistula to prevent further aspiration pneumonia. In case of persistent leakage from incomplete expansion of the stent, repeat esophagogram should be obtained 2 - 3 days after stent placement to confirm stent expansion before suggesting safe oral intake. Procedural complications include tracheal compression in 7-10% of the patients and respiratory failure in 6% of the patients.
A close follow-up of patients with esophageal respiratory fistula is recommended since non-sealing of a fistula after stent placement, reopening of a fistula after initial sealing and/or development of a new fistula might cause aspiration pneumonia which would result in respiratory failure and death. The protocol of a repeat esophagogram at 1 week and then every 1 -2 months after the procedure is suggested to evaluate fistula closure and stent patency or migration. This would also provide early detection of fistula reopening as well as long-term outcomes.
Learning points
This case provides an excellent example of an uncommon pathology presenting with non-specific symptoms. A high index of suspicion should be held in patients with dysphagia symptoms, weight loss and pulmonary complications. A holistic approach with the involvement of pulmonologist, gastroenterologist and thoracic surgeon is essential to improve patient care. Given the significant morbidity and mortality associated with a missed diagnosis, early detection and prompt treatment with an endoscopically placed covered stent and close follow-up are crucial. Further prospective studies are required to establish official guidelines for the management of esophageal respiratory fistulas since only a few retrospective studies exist so far that highlight the outcome and treatment options for this devastating disease.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Not applicable.
Author Contributions
Ruhma Ali MD, Aditya Patel MD, and Muhammad Hussain MD: diagnosis and management of the patient, discussion, writing and drafting of the case, final approval of the case report. Theodore DaCosta MD, Yatinder Bains MD, and Richard Miller MD: management of the patient, revision and final approval of the case report.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Elsayed AAA, Mohamed EEH, Ahmed ARH. Case report: acquired esophageal-pulmonary fistula. Esophagus. 2016;13:93-96.
doi - Bixby BA, Maddock SD, Reddy CB, Iravani A, Ansari SA. Acquired esophago-respiratory fistulae in adults. Shanghai Chest. 2019;4:4.
- Mangi AA, Gaissert HA, Wright CD, Allan JS, Wain JC, Grillo HC, Mathisen DJ. Benign broncho-esophageal fistula in the adult. Ann Thorac Surg. 2002;73(3):911-915.
doi - Balazs A, Kupcsulik PK, Galambos Z. Esophagorespiratory fistulas of tumorous origin. Non-operative management of 264 cases in a 20-year period. Eur J Cardiothorac Surg. 2008;34(5):1103-1107.
doi pubmed - Lenz CJ, Bick BL, Katzka D, Nichols FC, Depew ZS, Wong Kee Song LM, Baron TH, et al. Esophagorespiratory fistulas: survival and outcomes of treatment. J Clin Gastroenterol. 2018;52(2):131-136.
doi pubmed - Reed MF, Mathisen DJ. Tracheoesophageal fistula. Chest Surg Clin N Am. 2003;13(2):271-289.
doi - Youness HA, Harris K, Awab A, Keddissi JI. Bronchoscopic advances in the management of aerodigestive fistulas. J Thorac Dis. 2018;10(9):5636-5647.
doi pubmed - Liu PS, Levine MS, Torigian DA. Esophagopleural fistula secondary to esophageal wall ballooning and thinning after pneumonectomy: findings on chest CT and esophagography. AJR Am J Roentgenol. 2006;186(6):1627-1629.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


