| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 10, Number 4, April 2019, pages 106-109
A Challenging Case of Granulomatous Mycosis Fungoides Mimicking Cutaneous Sarcoidosis
Krishna Mohan Baradhia, d, Ramya Pakalab, Supriya Koyac
aDivision of Nephrology, University of Oklahoma, 4502 E 41st, OU-Tulsa Schusterman Center, Tulsa, OK 74135, USA
bChalmeda Anand Rao Institute of Medical Sciences, Telangana, India
cHematology-Oncology, Hillcrest Medical Center, 1245 S Utica Ave Ste 240, Tulsa, OK 74104, USA
dCorresponding Author: Krishna Mohan Baradhi, Division of Nephrology, University of Oklahoma, 4502 E 41st, OU-Tulsa Schusterman Center, Tulsa, OK 74135, USA
Manuscript submitted March 4, 2019, accepted March 18, 2019
Short title: Granulomatous Mycosis Fungoides
doi: https://doi.org/10.14740/jmc3276
| Abstract | ▴Top |
Granulomatous mycosis fungoides was first described by Ackerman and Flaxman in 1970 and is characterized histologically by diffuse invasion of dermis by giant cell lymphocytes. Granulomatous mycosis fungoides is a subtype of cutaneous T-cell lymphoma which is a variant of non-Hodgkin’s lymphoma. It usually affects middle-aged adults, presenting as progressive skin lesions. Initial diagnosis can be extremely challenging as it mimics various dermatopathies both clinically and histologically. Despite advances in diagnostic techniques, diagnosis is often delayed, as granulomatous mycosis fungoides is a great imitator. We describe a unique case of a 51-year-old female presenting with cutaneous granulomatous infiltration, which was initially diagnosed as sarcoid granulomatous dermatitis; and after 6 years of evolution, was eventually determined to be granulomatous mycosis fungoides. We discuss the rare presentation of granulomatous mycosis fungoides misdiagnosed as sarcoid granulomatous dermatitis and the challenges encountered in confirming the lymphoma diagnosis. Clinicians and pathologists should consider this entity in differential diagnosis, when encountered with persistent granulomatous skin lesions, as extensive granulomatous lesions tend to obscure the underlying lymphoma. Immunophenotyping and molecular gene rearrangement studies can improve diagnostic accuracy.
Keywords: Granulomatous mycosis fungoides; Sarcoidosis; Non-Hodgkin’s lymphoma; Granuloma; Plaques; T-cells
| Introduction | ▴Top |
Though mycosis fungoides is the most common form of cutaneous lymphoma, granulomatous mycosis fungoides (GrMF) remains a rare subtype of cutaneous lymphoma. GrMF is caused by unusual expression of cluster of differentiation (CD)4 T lymphocytes, a part of immune system. GrMF has an incidence of 1 in 100,000 - 350,000. Most cases are in people 40 - 55 years of age. It is twice more common in males than in females. The granulomatous component may be intense and obscures the lymphomatous component in some patients [1]. We present a 51-year-old female with significant plaque measuring about 10 cm in the L3 - L5 lumbar area and a similar plaque in the region of right ankle which was initially diagnosed as sarcoid granulomatous dermatitis on immunohistopathology. It was later diagnosed as GrMF on repeat biopsies of the plaques. GrMF simulating sarcoidosis has rarely been reported in literature.
| Case Report | ▴Top |
A 51-year-old Caucasian woman with diabetes, hyperlipidemia and chronic pain initially presented to the clinic after she noticed a patch associated with pruritus on her right ankle, below medial malleolus. A similar lesion was found on her back in L3 - L5 dermatomal region (Fig. 1). Further history and exam were largely unremarkable. Skin biopsy with immunohistopathology of the two regions showed areas of epithelioid histiocytes with multinucleated giant cells mixed with a significant lymphocyte component. Computed tomography (CT) scan of the chest and abdomen showed no adenopathy. The granulomatous reaction was initially diagnosed as sarcoidosis, and was started on corticosteroids. Unfortunately, there was no improvement in the lesions.
 Click for large image | Figure 1. Erythematous violaceous plaque over back in the lumbar area. |
Subsequently few years later, two other biopsies of the hyperpigmented and erythematous plaques were performed. Immunohistochemical staining of the specimen composed of T-helper cell subtypes CD2+, CD3+, CD5+ with partial loss of CD7. Numerous T-suppressor/CD8+ subsets was seen with none expressing B-cell markers. There was prominent positivity of numerous histiocytes with CD4. A few rare cells stained CD30+. Loss of one or more of the pan T-cell markers, mostly CD5/CD7 is common in mycosis fungoides. Twenty percent of early mycosis fungoides show CD8+ (Figs. 2, 3). Molecular studies with T-cell receptor gene rearrangement showed evidence of T-cell clonality, favoring diagnosis of GrMF.
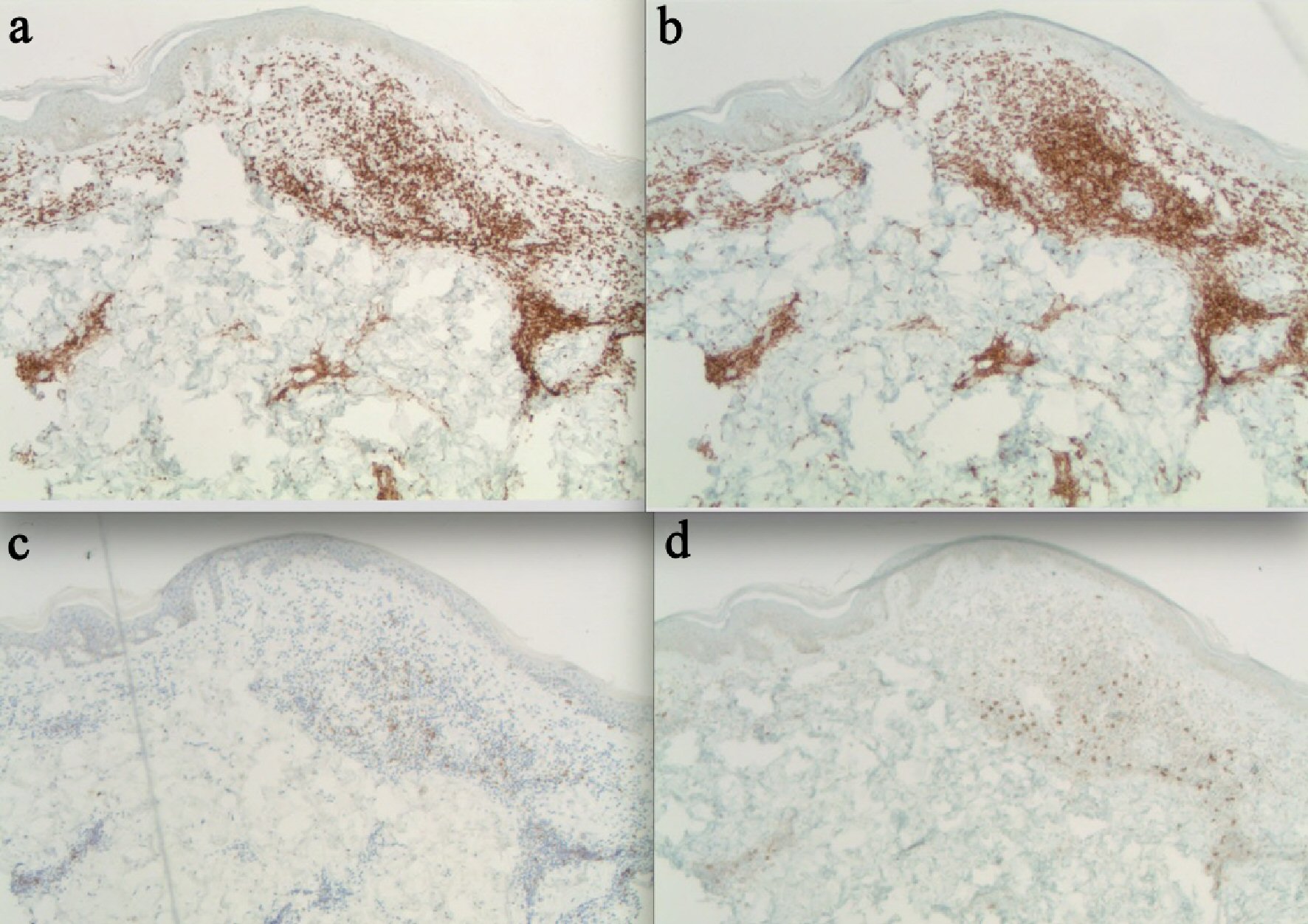 Click for large image | Figure 2. Skin biopsy. (a) CD3 stain. Skin biopsy of the lumbar area depicting CD3+ scattered T-cell lymphocytes. (b) CD4 stain. Striking feature of dermal invasion by strongly positive CD4+ lymphocytes. (c) CD7 stain. Infiltration by strongly positive CD7+ lymphocytes. (d) CD8 stain. Positive for scattered CD8+ lymphocytes. |
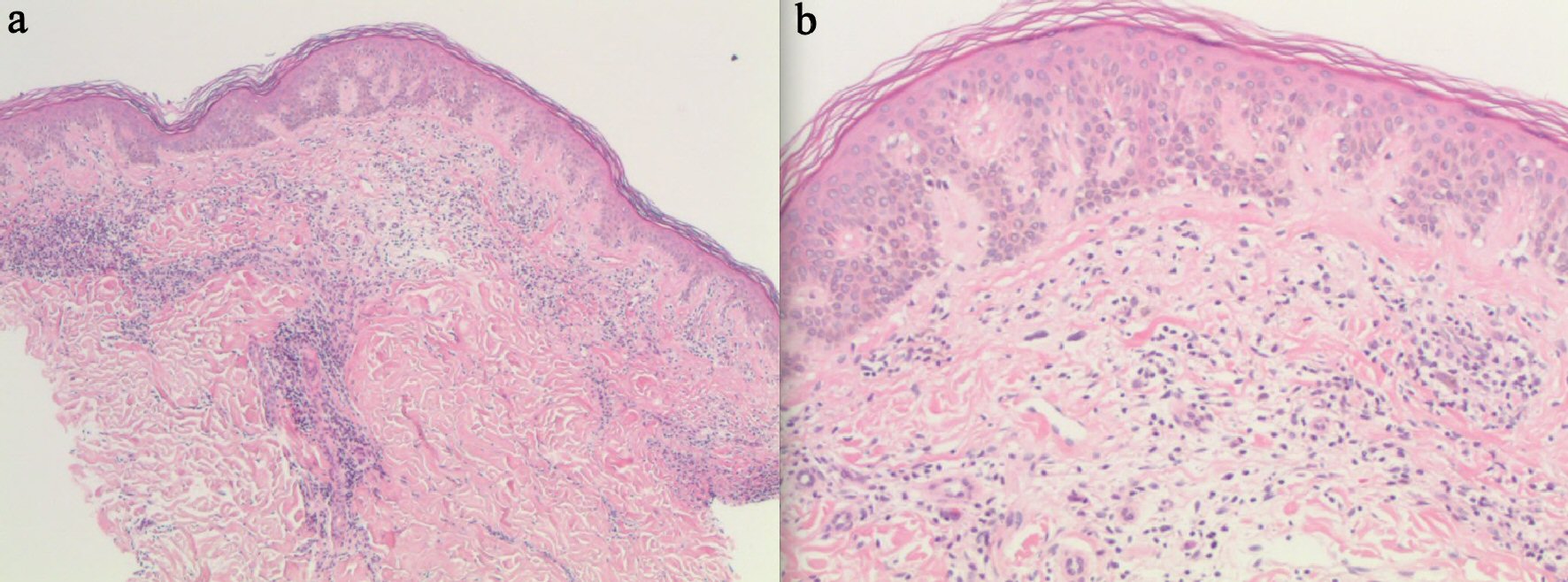 Click for large image | Figure 3. Skin biopsy. (a) H&E stain of skin and subcutaneous tissue infiltration with lymphocytes and granuloma formation. (b) H&E stain. Dermal invasion by pleomorphic atypical lymphocytes. |
Bone marrow biopsy was unrevealing, dismissing the possibility of systemic involvement. TNM classification was T1 N0 M0 (stage Ib). Patient skin lesions were refractory to ultraviolet B (UVB) therapy. Hence, immunotherapy with brentuximab was initiated. Patient initially responded to this treatment with mild improvement of the plaques. However, she later developed significant numbness and tingling of the toes as an adverse effect of brentuximab, leading to its discontinuation. The biopsy at this stage stained positive for CD30. Finally, radiation therapy was started, following which the lesion showed marked improvement in its appearance (Fig. 4).
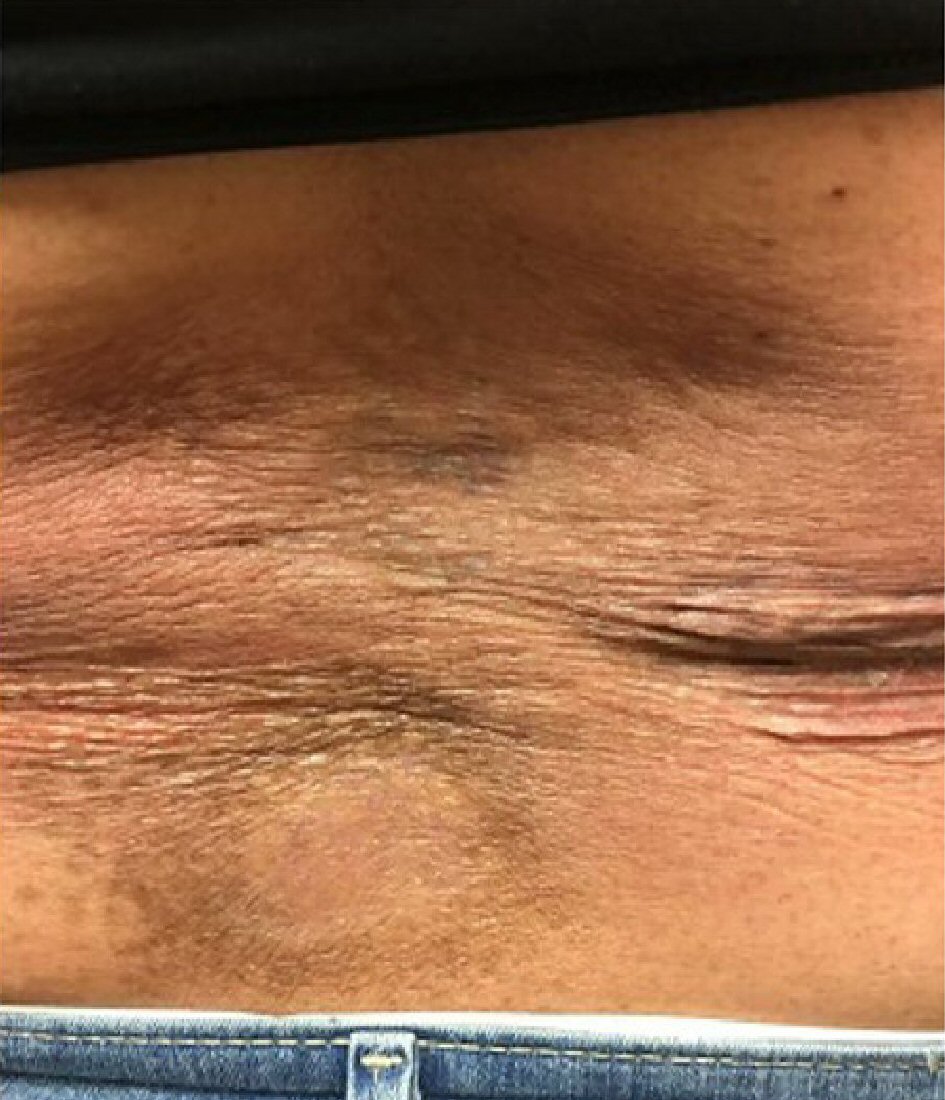 Click for large image | Figure 4. Improvement of plaque over back. |
| Discussion | ▴Top |
Mycosis fungoides is the most commonly described primary cutaneous T-cell lymphoma. GrMF is a rare subtype of cutaneous T-cell lymphoma first described by Ackerman and Flaxman in 1970. GrMF is characterized by dermal invasion of T cells with associated epithelioid and giant cells. It typically affects middle-aged adults and may present initially as a patch and then progresses to plaque and eventually evolve into a tumor in some individuals. In different studies, it is also found that there is a slightly increased incidence of lympho-proliferative disease, occurring after chronic sarcoidosis, probably as a consequence of immunologic abnormalities observed in lymphoproliferative disease [2].
A strong granulomatous component can sometimes obscure the underlying cutaneous lymphoma, which is mistaken for cutaneous sarcoidosis [3]. Only few cases have been reported in literature about GrMF being mistaken for sarcoidosis as depicted in our case [3-5]. In most cases, cutaneous granulomatous lesions follow the course of underlying lymphoproliferative disease and are considered as a possible malignant lymphoma [3].
Diagnosis can be challenging due to heterogeneous clinical and histopathological features. No particular diagnostic clinical criteria are available for diagnosis of GrMF, because of its variable presentations and hence the detection of GrMF is primarily considered histopathology diagnosis [6].
Histologically, GrMF shows dermal T-cell intrusion with epithelioid and giant cell granulomas without necrosis mimicking other granulomatous disease like sarcoidosis. Variants may be misleading simulating other inflammatory dermopathies when the epithelioid and giant cell feature dominates [7]. Distinct clinical characteristics are not present. Apart from granulomatous formation, no other noticeable features are evident. The same features were seen in our patient, which misdirected the diagnosis as sarcoidosis. The International Society of Cutaneous Lymphoma consensus algorithm advocates immunophenotyping and molecular gene rearrangement studies to aid clinic-pathological diagnosis of GrMF [6].
Patients with stage 4 disease, advanced age, blacks have worse prognosis, while a survival rate of stage 1 disease is more than 20 years. The clinical significance of granulomas in prognostication of mycosis fungoides is uncertain as both indolent and aggressive cases have been described.
Conclusions
GrMF is a diagnostic challenge, in the light of perplexing histopathological variants. Our case adds to growing number of GrMF cases misdiagnosed as sarcoidosis highlighting the plight of diagnostic obstacles. When the patient’s clinical course does not support the diagnosis of sarcoidosis, the coexistence of granulomas and typical histologic features of mycosis fungoides should indicate GrMF. Clinical dissection of atypical clinic-pathological variants coupled with immunophenotyping and molecular genetics, is crucial for early diagnosis and accurate treatment.
Acknowledgments
None to declare.
Financial Disclosure
No funding.
Conflict of Interest
No conflict of interest to disclose.
Informed Consent
Patient consent was taken.
Author Contributions
All authors equally contributed to this manuscript.
| References | ▴Top |
- Gallardo F, Garcia-Muret MP, Servitje O, Estrach T, Bielsa I, Salar A, Abella E, et al. Cutaneous lymphomas showing prominent granulomatous component: clinicopathological features in a series of 16 cases. J Eur Acad Dermatol Venereol. 2009;23(6):639-647.
doi pubmed - Brincker H. The sarcoidosis-lymphoma syndrome. Br J Cancer. 1986;54(3):467-473.
doi pubmed - Bessis D, Sotto A, Farcet JP, Barneon G, Guilhou JJ. Granulomatous mycosis fungoides presenting as sarcoidosis. Dermatology. 1996;193(4):330-332.
doi pubmed - Mainguene C, Picard O, Audouin J, Le Tourneau A, Jagueux M, Diebold J. An unusual case of mycosis fungoides presenting as sarcoidosis or granulomatous mycosis fungoides. Am J Clin Pathol. 1993;99(1):82-86.
doi pubmed - Maillard H, Croue A, Francois S, Verret JL. [Granulomatous mycosis fungoides histologically simulating cutaneous sarcoidosis]. Ann Dermatol Venereol. 1998;125(12):912-915.
pubmed - Ferrara G, Di Blasi A, Zalaudek I, Argenziano G, Cerroni L. Regarding the algorithm for the diagnosis of early mycosis fungoides proposed by the International Society for Cutaneous Lymphomas: suggestions from routine histopathology practice. J Cutan Pathol. 2008;35(6):549-553.
doi pubmed - Byragani D, Baradhi K, Schendrick I, Koya S. Langerhan cell histiocytosis: a rare disorder with a rare presentation. World J Oncol. 2015;6(2):335-337.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


