| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 2, Number 5, October 2011, pages 210-215
Anterior Tibial Cortex Stress Fracture in a High Demand Professional Soccer Player
Ioannis Gigisa, b, Ioannis Rallisa, Panagiotis Gigisa, Vasilis Gouliosa
aOrthopaedic Department, Interbalkan Medical Center, Aristotle University of Thessaloniki, Thessaloniki, Greece
bCorresponding author: Ioannis Gigis, Assisstant Professor of Orthopaedics, Profiti Ilia 13, Pylea, 55535, Thessaloniki, Greece
Manuscript accepted for publication June 8, 2011
Short title: Anterior Tibial Cortex Stress Fracture
doi: https://doi.org/10.4021/jmc249e
| Abstract | ▴Top |
Anterior tibia cortex consists a less common location stress fractures. Treatment and return-to-play decision making can have the greatest impact on an athlete’s career. We report a case of a 33 years old high demand professional soccer player who suffered an anterior tibia cortex stress fracture. After a short period of conservative treatment we proceeded in an intramedullary nailing, drilling on the fracture site and insertion of autologous growth factors were performed in order to assisst the healing process. He returned to full activities (every day training and official games) 9 weeks after the operation. The last radiograph 6 months post operatively showed healing of the fracture. We believe that intramedullary fixation of anterior cortex tibial stress fractures when combined with drilling and the use of growth factors helps return sooner than expected to full pre-injury levels of performance.
Keywords: Anterior tibia stress fracture; Intramedullary nailing; Autologous growth factors; Soccer player
| Introduction | ▴Top |
Stress fractures in professional soccer players have become a very common entity worldwide. Although stress fractures of the tibia are the most frequent, anterior tibia cortex consists a less common location for this type of fractures. They were first described in 1956 by Burrows [1], who reported on five ballet dancers who had such lesion. Constant tension from posterior muscle forces and hypovascularity of the anterior aspect of the tibia predispose this site to nonunion or delayed union. Treatment and return-to-play decision making can have the greatest impact on an athlete’s career.
We describe a case of a high demand professional soccer player who suffered this particular form of tibial stress fracture that involved the anterior cortical aspect of the midsaft, the treatment that followed and lead to return to full activity much sooner than expected.
| Case Report | ▴Top |
We present a case of a 33-year-old professional high demand soccer player with an anterior tibia cortex stress fracture.
Three months prior the end of the season, the athlete complained for pain at the anterior aspect of his left tibia but the radiographs that followed didn’t reveal anything important. After some rest the athlete continued his activities without further problems until the end of the season. He departed for vacations to his home country and only after a week he reported serious pain, tenderness and swelling within a localized area in the anterior left tibia. The local doctor made all the necessary radiographs along with a CT and MRI and the diagnosis was a stress fracture on the anterior cortex of the left tibia. Conservative treatment was then decided and the athlete took a 2 months rest before he returned to his basis. He then took full responsibility and decided to participate in all activities of the club since he had no pain and although the radiographs showed no healing. No more than 2 months later he complained again for pain at the same area and the radiograph revealed fracture of the ipsilateral fibula (Fig. 1). Apart from pain, swelling, local tenderness and a palpable callus were added in the clinical examination. Pain was present not only during exercise but in rest also. Bone scan (Fig. 2) and CT (Fig. 3) verified the diagnosis as well as the absence of any healing process and the decision for operating treatment was made.
 Click for large image | Figure 1. Anteroposterial and lateral radiographs showing cortical hypertrophy (black arrow) and a ‘black line’ (white arrow) defect on the anterior cortex of the middle third of the left tibia as well as periosteal thickening and lucent line of the fracture (black thick arrow) at the same height of the fibula. |
 Click for large image | Figure 2. Bone scan demonstrating a discrete area of moderately increased uptake of technetium on the anterior border of the middle third of the left tibia. |
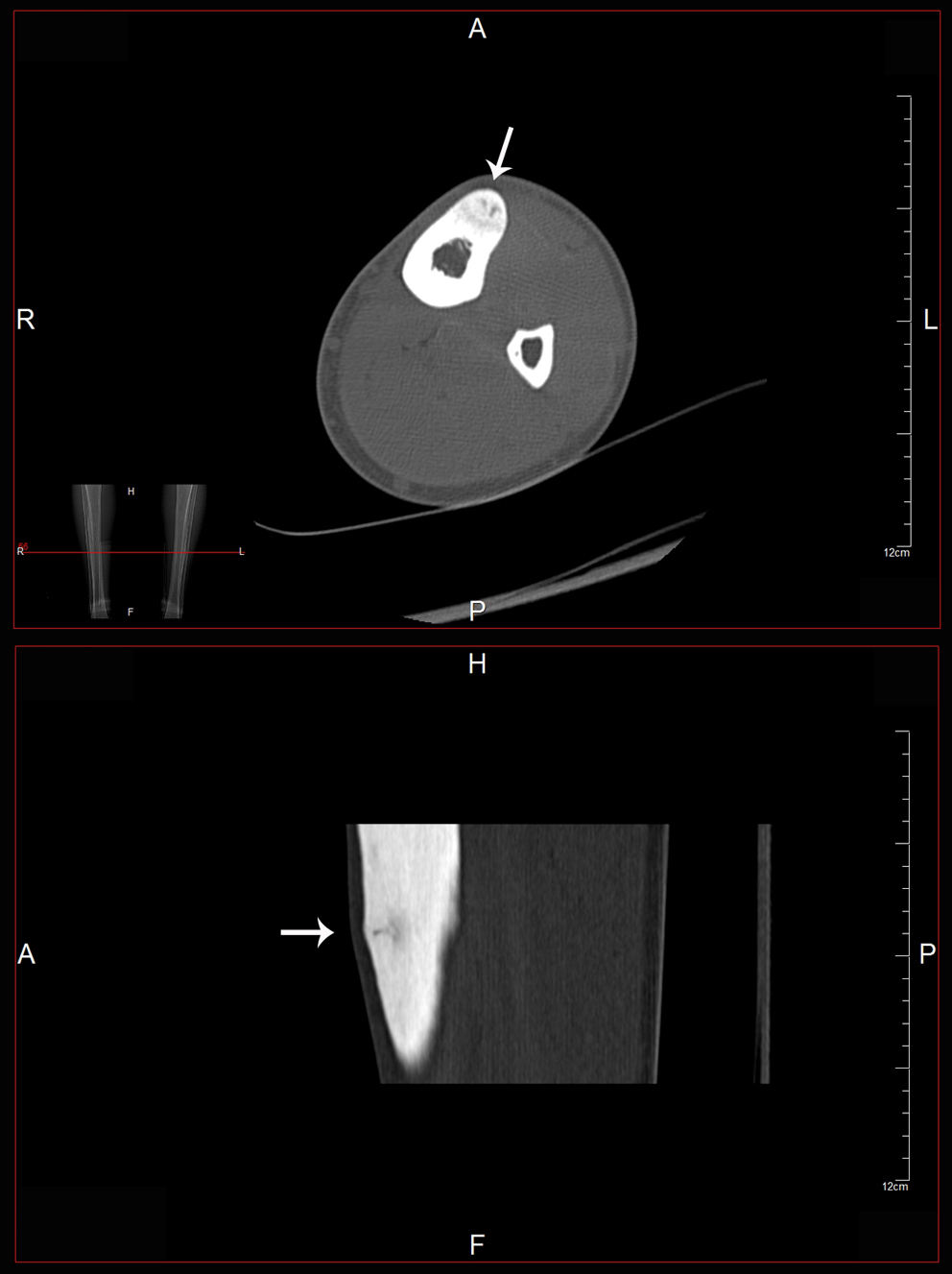 Click for large image | Figure 3. CT axial and coronal images showing an abnormal area (arrows) on the anterior part of the middle third of the tibia. |
We performed an intramedullary nailing of the left tibia along with some drilling at the fracture area. Additionally we inserted autuogous growth factors through the drilling holes in order to assist the healing process (Fig. 4).
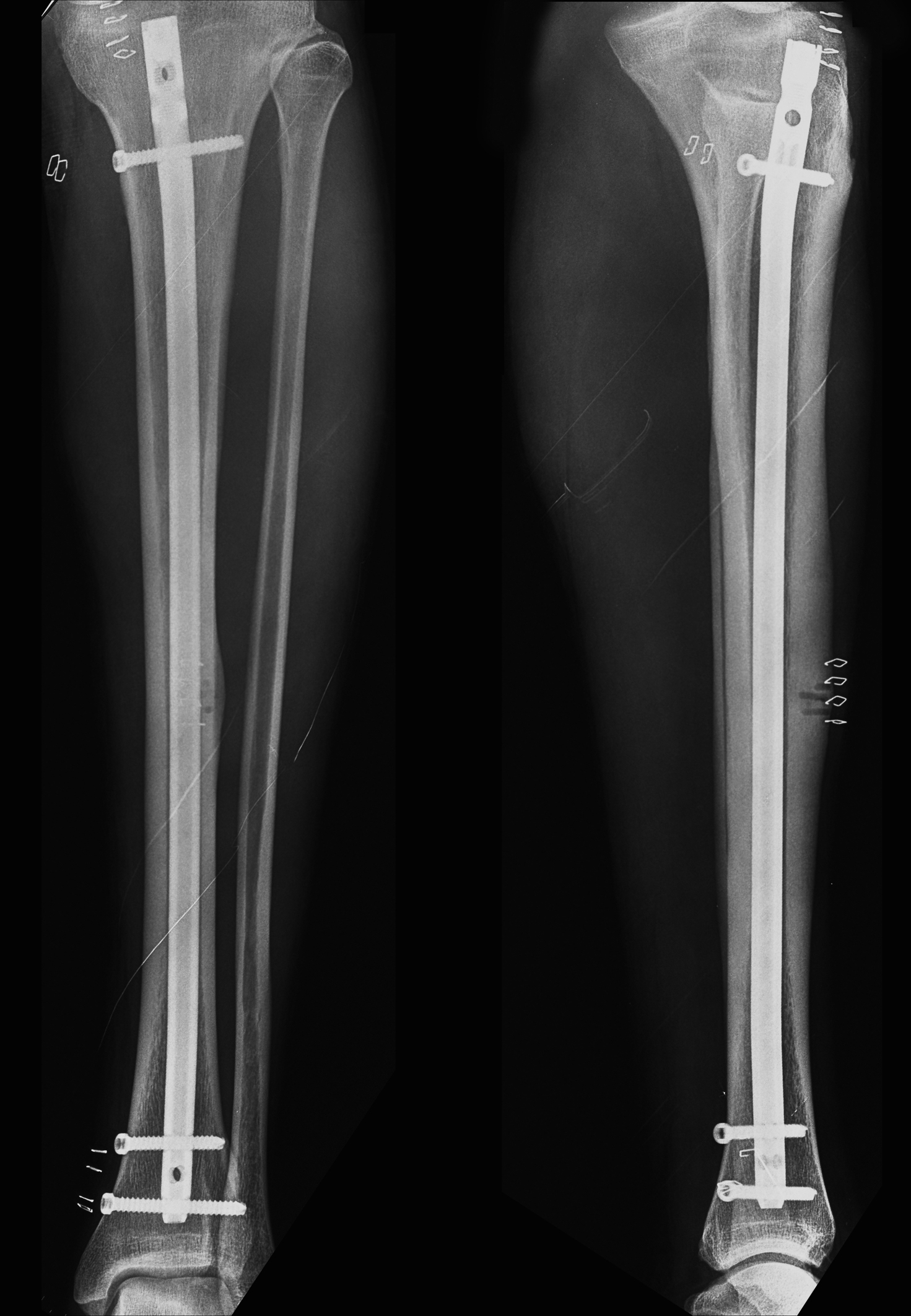 Click for large image | Figure 4. Post-operative radiographs showing intramedullary nailing of the tibia as well as drilling that was performed on the site of the fracture |
He was allowed partially weight bearing along with the use of crutches for two weeks while full range mobilization of the knee and ankle and strengthening of the quadricheps were performed immediately after the operation. Physiotherapy continued until the sixth week postoperatively and then he was allowed to start jogging and running. Two months post operatively the radiograph showed some healing (Fig. 5) and he was allowed to perform excersises with the ball. As soon as he reached the ninth week he returned to full activity with the rest of the team with participation in every day training and official games. During this period and up to six months post operatively he has no pain or any other symptom from the left tibia or any other limitation. The final radiograph shows advanced healing of the fracture (Fig. 6).
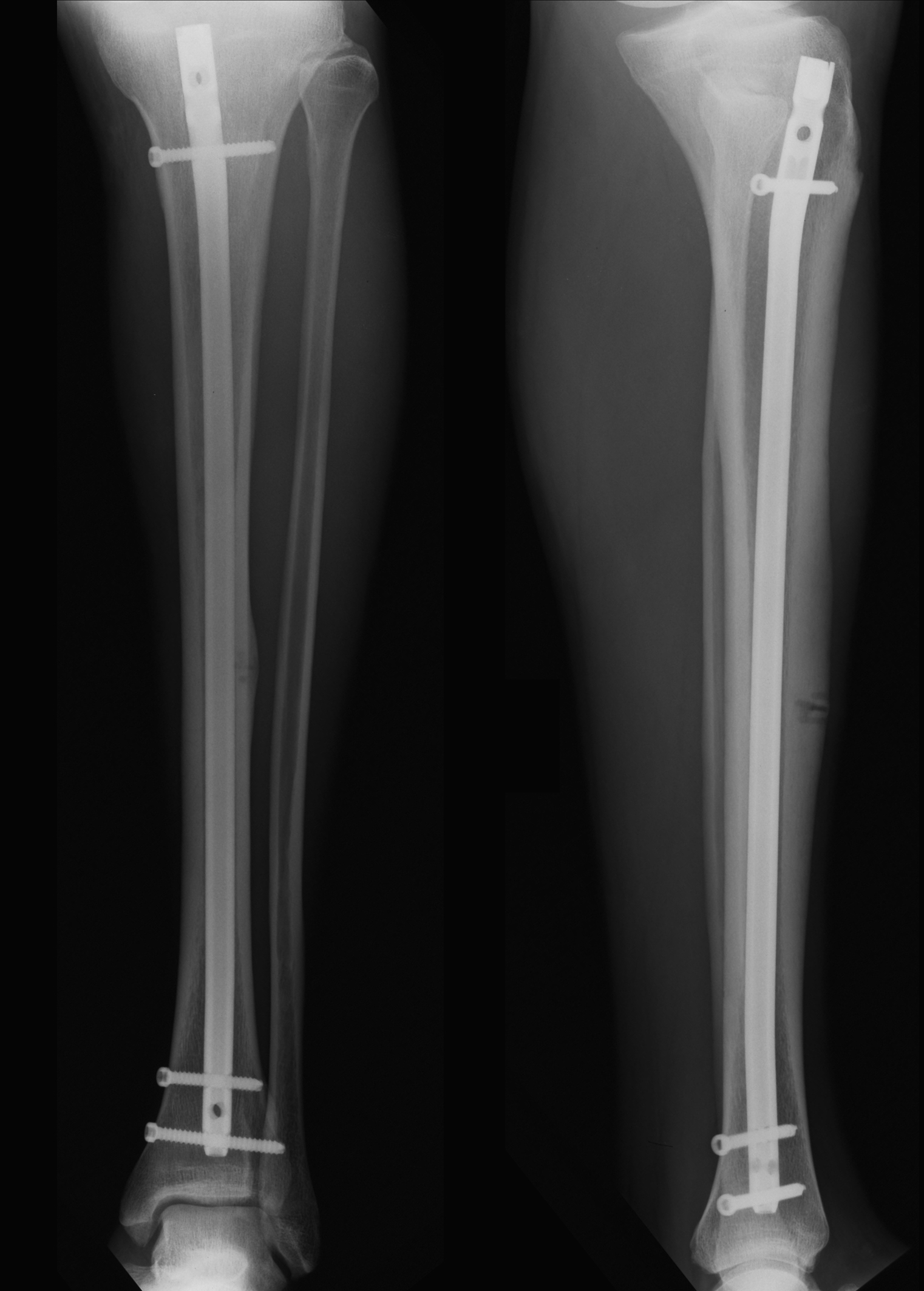 Click for large image | Figure 5. Two months post-operatively and the healing process seems to have commenced. |
 Click for large image | Figure 6. Six months post-operatively showing advanced healing of the stress fracture. |
| Discussion | ▴Top |
As athletes continue to be more competitive in their desire to be the best, they will train exceptionally hard, sometimes to the point of injury. Stress fractures are commonly diagnosed in competitive athletes [2]. They were first reported in 1855 by Briethaupt in Prussian soldiers. This kind of fractures can occur when the stresses on the bone are greater than the capacity of the bone to withstand and heal from the stresses. Injuries like these are most common in the lower extremities of repetetive-motion athletes especially in professional soccer players [3]. Theories that try to justify this include the field being too hard; possible dysfunctional shoe design; training progressions or duration, intensity and frequency may be too intense; fitness levels; or abnormalities in nutrition and endocrine variables [4]. Although stress fractures of the tibia are the most frequent, anterior tibia cortex consists a less common location for this type of fractures. They were first described in 1956 by Burrows [1]. It is relatively rare form of stress fracture, making up 2.7% [5] to 4.6% [6] of all cases.
Repeated compression loading is the pathophysiological mechanism involved according to Mabit et al [7]. In contrary Wagner et al [8] showed that the anterior aspect of the midshaft of the tibia is an area under tension than compression. Stanitsky et al [9] believes that concentrated muscle forces acting across a specific bone enhance the loading which occurs simply from direct weightbearing thus anterior cortex fractures of the tibia may be due to additional forces from the posterior muscle group causing increased anterior tension stress. As a consequence these lesions appear to be prone to delayed union or non union. Histopathologic examination of chronic anterior cortex tibial stress fractures has revealed fibrotic infiltrations, local osteonecrosis and limited or no bone remodeling activity, consistent with pseudarthrosis. Rolf and colleagues [10] reported no evidence of bone remodeling, absence of inflamatory cells, extensive fibrotic infiltration and local avascular bone necrosis in two patients with anterior tibia cortex stress fractures. The relative hypovascularity of the anterior cortex, which is subcutaneous, may be a factor promoting this complication. Another possible complication is the development of an acute fracture [11]. Brahms et al [12] reported such a case of a professional football player who played three and a half seasons before sustaining an acute tibial fracture through the site of the stress fracture. Our case was a high demand professional soccer player. He had to train hard every day and sometimes twice a day and play a game once or twice a week for 90 minutes most of the times in two competitive championships local and european.
Symptoms vary and may be vague in nature. Initially pain is present only with activity and may be associated with localised tenderness. As the stress fracture progresses, pain begins to affect performance and with continued training pain persists into daily living activities [13]. Physical examination usually reveals tenderness within a localized area. Also several authors have frequently observed swelling or a palpable callus [5, 14, 15]. Our athlete’s first symptom was pain and swelling appeared only 10 weeks after the initial pain. When pain persisted into daily activities, swelling and tenderness were found and a palpable callus was obvious. Compartments should be palpated as well as a thorough neurovascular examination. Differential diagnosis includes muscle strain, medial tibia stress syndrome, stress reaction, periostitis, infection, bursitis, neoplasm, compartment symdrome and nerve entrapment.
Plain radiographs are usually normal within the first few weeks but may be useful when positive. Subsequently they develop a characteristic V-shaped defect in the anterior cortex but callus formation is generally absent[15]. Once the cortex becomes hypertrophied and the fissure widens, the healing capacity is limited . If a stress fracture is suspected based on history and physical examination and repeat radiographs remain negative although the athlete continuous to have symptoms then advanced imaging is required. According to Young et al [13] bone scans are considered the standard for diagnosing stress fractures but it is not a useful tool to monitor healing progress. In our case the V-shaped defect in the anterior cortex can be clearly seen in the pre-operation radiograph. The bone scan was also very characteristic.
CT is less expensive and offers adequate bony detail including location, orientation and extent as well as signs of healing. The CT that we performed in our athlete in accordance with the clinical history and examination, the x-ray and the bone scan set the diagnosis so definitely that there was no need to proceed with an MRI.
Magnetic resonance imaging is of course a valuable tool in identifying stress fractures. According to Diehl et al[3] MRI has become the method of choice because of its availability, speed and the amount of information that is provided. MRI shows more precise the location and the extent of fracture. Specificity and positive predictive values may approach 100%. Young and McAllister [13] point that it is more useful in grading lesions and therefore guiding treatment options. Arendt and colleague [16] proposed a grading system (Normal or Grade 0 to Grade 4) based on radiographs, bone scans, MR image and suggested treatment but was used for other bones whereas the one used by Fredericson et al [17] was developed using data for the tibia alone. According to this grading system normal or grade 0 has normal radiographs, a normal bone scan and a normal MR appearance on all sequences. Grade 4 though, represents true stress fractures and can be clearly seen radiographically as well as on all MR sequences. The scintigraphic appearance shows a more intense focal cortical uptake typical of a Grade 4 injury. By grading stress fractures, the approximate time to healing can be predicted.
Classification of stress fractures into high risk or low risk has been suggested by various authors [18, 11]. High-risk stress fracture locations include among others, the anterior tibia cortex. Delay in diagnosis or with less aggressive treatment, these fractures tend to progress to nonunion or complete fracture, require operative management or recur in the same location. Our patient suffered a high-risk stress fracture and probably the initial less aggressive conservative treatment led to the fracture of the ipsilateral fibula but in comparison with reported similar cases, the 4 months period from the initial symptom to the operation cannot be considered a big delay.
The management of bony stress injuries should be based on the location and grade of the injury. These details give the amount of microdamage that has accumulated and wether it is a high-risk or low-risk injury.
Treatment decisions should be made only after careful consideration of the individual athlete, based on the type and duration of symptoms, fracture pattern and level of competition. Return-to-play decisions for athletes who have high-risk stress fractures are more difficult than for low-risk fractures. Highly competitive athletes who place a greater amount of stress at these high-risk locations are at increased risk for fracture progression and reinjury and according to Diehl and colleagues [3] should be managed aggressively. This kind of teatment may prevent the athlete from having a repeat injury in a subsequent season. Diehl and colleagues [3] believe that athletes with anterior cortex stress fractures of the tibia may return to activity faster with surgical management compared with conservative treatment. Surgery may speed healing of the fracture, allow earlier return to play, prevent refracture and a catastrophic fracture progression. Young and McAllister [13] support that anterior tibial stress fractures benefit from intramedullary nailing. Plasschaert et al [19] had to use intramedullary nailing for such a fracture in a professional ballet dancer after an unsuccessful year of concervative treatment and later tibial drilling. Barrick and Jackson [20] proposed a successful prophylactic intramedullary nailing in a professional football player. Brukner and colleagues [21] reported a case of a bilateral anterior tibial cortex stress fracture in a football player treted with intramedullary nailing that led to satisfactory clinical and radiographic healing of the fracture of the right tibia. They operated after a five year unsuccessful conservative treatment which included periods of rest, training modifications, physical therapy modalities, strengthening exercises for the muscles of the leg and foot orthoses. Rolf and colleagues [10] reported that drilling and bone grafting had not been successful although theoritically they would increase the vascularization and enhance bone remodelling. Drilling, though, combined with rest up to six months, as reported by Orava et al [22], was successful. Rolf and colleagues concluded that their cases demonstrate that athletes with high functional demands who suffer from such fractures must be treated with a stabilizing surgery. Rettig et al [15], in a series in which a regimen of rest and external electrical stimulation was evaluated, seven of eight patients showed complete healing after an average of 8.7 months of treatment. Batt and coworkers [23] reported successful healing in all three patients in a mean of 8 months with the use of a pneumatic leg brace. On the other hand Chang and Harris [24] reported good to excellent results in five patients that were treated with reamed unlocked tibial nails. Blank [5], in a study of five patients reported that none of the fractures healed despite immobilization in a cast for three to five months. Similar results were reported by Green et al [25]. These reports suggest that although surgical intervention may become necessary, conservative measures may still be successful and should be considered but not in high demand professional athletes.
In the case we present we deal with a 33 years old high demand professional soccer player. It is apparent that his soccer future due to his age is limited and thus does not have the luxury to wait for a long period of conservative treatment. The decision to proceed with the operation was taken after a thorough discussion with the player and his club. We proceeded with what we believe is the suggested method of operative treatment in such cases. We added the drilling and the insertion of autologous growth factors in order to further assist the healing process.
In conlusion, intramedullary fixation when combined with drilling and the use of growth factors helps the athlete return sooner than expected to full pre-injury levels of performance. It is apparent that the use of growth factors in such cases must be further studied in future papers.
Conflict of Interest
None.
| References | ▴Top |
- Burrows HJ. Fatigue infraction of the middle of the tibia in ballet dancers. J Bone Joint Surg Br. 1956;38-B(1):83-94.
pubmed - Pepper M, Akuthota V, McCarty EC. The pathophysiology of stress fractures. Clin Sports Med. 2006;25(1):1-16, vii.
pubmed - Diehl JJ, Best TM, Kaeding CC. Classification and return-to-play considerations for stress fractures. Clin Sports Med. 2006;25(1):17-28, vii.
pubmed - Knapp TP, Mandelbaum BR, Garrett Jr WE (1998). Why are stress injuries so common in the soccer player? Clin Sports Med 17 (4): 835-853.
- Blank S. Transverse tibial stress fractures. A special problem. Am J Sports Med. 1987;15(6):597-602.
pubmed doi - Orava S, Hulkko A. Delayed unions and nonunions of stress fractures in athletes. Am J Sports Med. 1988;16(4):378-382.
pubmed doi - Mabit C, Pecout C. Non-union of a midshaft anterior tibial stress fracture: a frequent complication. Knee Surg Sports Traumatol Arthrosc. 1994;2(1):60-61.
pubmed - Wagner J, Bourgois R, Hermanne A. Mechanical behavior of the tibio-fibular aspects of genu varum and valgum. Acta Orthop Belg. 1982;48(1):57-92.
pubmed - Stanitski CL, McMaster JH, Scranton PE. On the nature of stress fractures. Am J Sports Med. 1978;6(6):391-396.
pubmed doi - Rolf C, Ekenman I, Tornqvist H, Gad A. The anterior stress fracture of the tibia: an atrophic pseudoarthosis? Scand J Med Sci Sports. 1997;7(4):249-252.
pubmed doi - Brukner P, Bradshaw C, Bennell K. Managing common stress fractures: let risk level guide treatment. Phys Sportsmed. 1998;26(8):39-47.
pubmed doi - Brahms MA, Fumich RM, Ippolito VD. Atypical stress fracture of the tibia in a professional athlete. Am J Sports Med. 1980;8(2):131-132.
pubmed doi - Young AJ, McAllister DR. Evaluation and treatment of tibial stress fractures. Clin Sports Med. 2006;25(1):117-128, x.
pubmed - Orava S, Hulkko A. Stress fracture of the mid-tibial shaft. Acta Orthop Scand. 1984;55(1):35-37.
pubmed doi - Rettig AC, Shelbourne KD, McCarroll JR, Bisesi M, Watts J. The natural history and treatment of delayed union stress fractures of the anterior cortex of the tibia. Am J Sports Med. 1988;16(3):250-255.
pubmed doi - Arendt EA, Griffiths HJ. The use of MR imaging in the assessment and clinical management of stress reactions of bone in high-performance athletes. Clin Sports Med. 1997;16(2):291-306.
pubmed doi - Fredericson M, Bergman AG, Hoffman KL, Dillingham MS. Tibial stress reaction in runners. Correlation of clinical symptoms and scintigraphy with a new magnetic resonance imaging grading system. Am J Sports Med. 1995;23(4):472-481.
pubmed doi - Boden BP, Osbahr DC. High-risk stress fractures: evaluation and treatment. J Am Acad Orthop Surg. 2000;8(6):344-353.
pubmed - Plasschaert VF, Johansson CG, Micheli LJ. Anterior tibial stress fracture treated with intramedullary nailing: a case report. Clin J Sport Med. 1995;5(1):58-61; discussion 61-52.
pubmed - Barrick EF, Jackson CB. Prophylactic intramedullary fixation of the tibia for stress fracture in a professional athlete. J Orthop Trauma. 1992;6(2):241-244.
pubmed doi - Brukner P, Fanton G, Bergman AG, Beaulieu C, Matheson GO. Bilateral stress fractures of the anterior part of the tibial cortex. A case report. J Bone Joint Surg Am. 2000;82(2):213-218.
pubmed - Orava S, Karpakka J, Hulkko A, Vaananen K, Takala T, Kallinen M, Alen M. Diagnosis and treatment of stress fractures located at the mid-tibial shaft in athletes. Int J Sports Med. 1991;12(4):419-422.
pubmed doi - Batt ME, Kemp S, Kerslake R. Delayed union stress fractures of the anterior tibia: conservative management. Br J Sports Med. 2001;35(1):74-77.
pubmed doi - Chang PS, Harris RM. Intramedullary nailing for chronic tibial stress fractures. A review of five cases. Am J Sports Med. 1996;24(5):688-692.
pubmed doi - Green NE, Rogers RA, Lipscomb AB. Nonunions of stress fractures of the tibia. Am J Sports Med. 1985;13(3):171-176.
pubmed doi
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


