| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 2, Number 5, October 2011, pages 194-196
Successful Endoscopic Management of Gastrojejunal Anastomotic Leak Following Open Roux-en-Y Gastric Bypass
Andrey Vizhula, Daniel W. Bircha, Shahzeer Karmalia, b
aCentre for the Advancement of Minimally Invasive Surgery, Division of General Surgery, University of Alberta, Edmonton, Alberta, Canada
bCorrespondence author: Department of Surgery, Division of General Surgery, University of Alberta, 405 CSC, 10240 Kingsway Avenue, Edmonton, AB T5H 3V9 Canada
Manuscript accepted for publication July 7, 2011
Short title: Endoscopic Management of Gastrojejunal Anastomotic Leak
doi: https://doi.org/10.4021/jmc252w
| Abstract | ▴Top |
Gastrojejunal anastomotic leak following Roux-en-Y gastric bypass (RYGB) for morbid obesity can lead to devastating and life-threatening intraabdominal sepsis. Typical management includes external drainage of the intraperitoneal collection with a risk of long lasting and difficult to manage gastrocutaneous fistula. The situation is additionally aggravated by the nature of a severely obese patient with multiple comorbidities and a modified gastrointestinal anatomy. In the reported case, the gastrojejunal leak after an open RYGB was successfully managed by a combined laparoscopic and gastroscopic intervention with a nasogastric drainage of intraabdominal collection. The quick recovery of the patient was based on the minimally invasive nature of the procedure and early aggressive enteral feeding via gastric remnant. Intraoperative gastroscopy allowed confirmation of the absence of free intraperitonel leakage and guided nasogastric drainage of the abscess. This report confirms the feasibility of a laparoscopic revision after open RYGB for a contained gastrojejunal insufficiency when it is combined with on-table gastroscopy.
Keywords: Bariatric surgery; Endoscopy; Leak; Anastamosis
| Introduction | ▴Top |
Gastrojejunal anastomotic leakage is recognized as one of the most common intraabdominal disruptions of gastrointestinal continuity following Roux-en-Y gastric bypass (RYGB) for morbid obesity. Although infrequent, it carries a high morbidity rate if not recognized and treated promptly.
| Case Report | ▴Top |
A 36-year old female with a body mass index of 53 kg/m2 and a medical history of type 2 diabetes, hypertension, asthma, urinary incontinence, depression and smoking underwent an elective open retrocolic, retrogastric RYGB with a hand sewn gastrojejunal anastomosis and a Stamm gastrostomy of the gastric remnant in November 2009. Upper gastrointestinal radiological study with water-soluble contrast on postoperative day 4 showed normal gastrojejunal transit and no anastomotic leak. The early postoperative period was uncomplicated; the patient was discharged home with bariatric liquid diet on day 7 after the procedure.
On postoperative day 14, the patient developed abdominal pain radiating into the right and left shoulder, diaphoresis, tachycardia (heart rate 102 beats per minute, blood pressure 134/70 mmHg). Her white blood cell count was 16.0 х 109/L. Computed tomography (CT) of abdomen demonstrated a large rim-enhancing multiloculated air and fluid collection near the gastrojejunal anastomosis and a small amount of free intraabdominal fluid (Fig. 1). Fluoroscopic study of the esophagus and stomach with gastrografin (Bracco Diagnostics, Princeton, NJ) demonstrated a large extraluminal contrast collection close to the gastrojejunal anastomosis with abscess formation (Fig. 2). An urgent diagnostic laparoscopy with on-table flexible gastroscopy was performed. No free purulent secretion was found in the abdominal cavity; only a small amount of serous fluid was aspirated. The abscess cavity was not entered. Flexible gastroscopy identified a large blow out of the gastrojejunal anastomosis and an abscess cavity behind it. Gastroscopic air insufflation and methylene blue injection into the gastric pouch and the adjacent abscess cavity did not demonstrate any bubbling or blue dye leak into the abdominal cavity. The leakage thus was found to be contained. A nasogastric tube was placed into the abscess cavity with the flexible gastroscope. The abdominal cavity was drained with a Jackson-Pratt drain placed into the left subdiaphragmatic space. The gastrostomy tube, placed in the original procedure and still remaining in a good position, was connected to a straight drain.
 Click for large image | Figure 1. Computed tomography of abdomen at admission, demonstrating a large rim-enhancing multiloculated air and fluid collection (white arrows) near the gastrojejunal anastomosis (black arrow). |
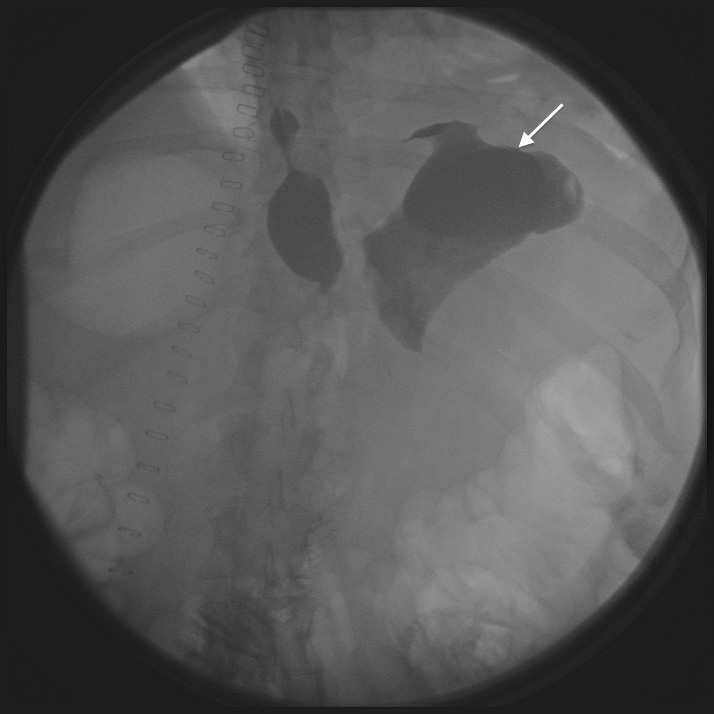 Click for large image | Figure 2. Fluoroscopic study of the esophagus and stomach with gastrografin before diagnostic laparoscopy. White arrow indicates the abscess cavity of the gastrojejunal anastomotic leak. |
Postoperatively, the patient was stable, slowly improving. Enteral feeding through the gastrostomy into the gastric remnant was continued during all the time of hospital admission and after the discharge home on postoperative day 25. No oral intake was allowed. Subsequent flexible gastroscopy and serial radiological studies with oral water-soluble contrast two and three weeks later demonstrated decrease in the size of the abscess and no intraabdominal leak of contrast (Fig. 3, 4). No gastrointestinal content or purulent material was detected coming from the Jackson-Pratt abdominal drain. After her hospital discharge, patient continued recovering with enteral feeding via gastrostomy; her nasogastric tube was removed and the gastrostomy tube was discontinued later, after subsequent follow up controls confirmed her favorable evolution.
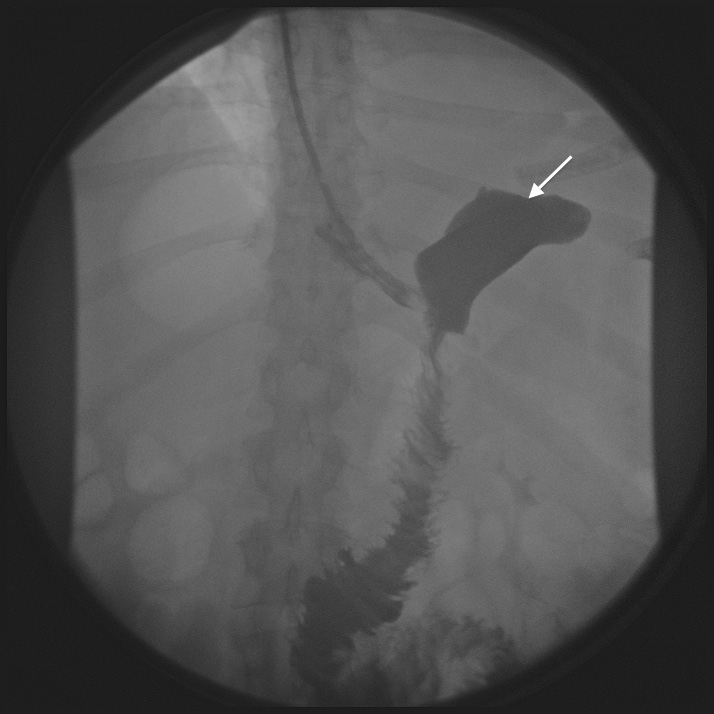 Click for large image | Figure 3. Fluoroscopic study of the esophagus and stomach with gastrografin on day 7 after laparoscopy and drainage. White arrow indicates decreasing size of an extraluminal abdominal collection. |
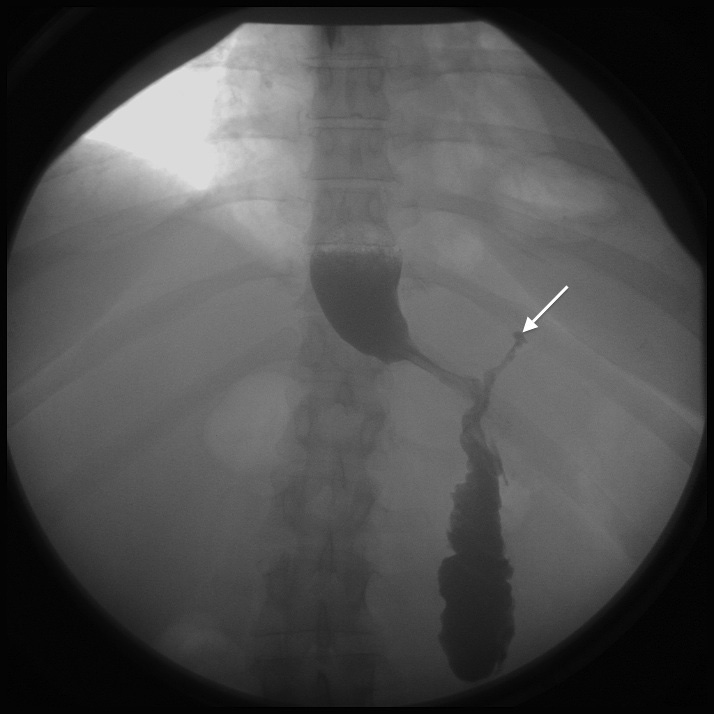 Click for large image | Figure 4. Fluoroscopic study of the esophagus and stomach with gastrografin on day 24 after laparoscopy and drainage. White arrows indicates small extraluminal residual cavity. |
| Discussion | ▴Top |
The leakage from the gastrojejunal anastomosis after RYGB is one of the most serious complications in bariatric surgery. It was reported to occur in 1.4% of RYGB patients [1]. The leaks are recognized as risk factors related to postoperative mortality [2, 3]. mmediate recognition of a leak is crucial to prevent severe surgical sepsis and death. The diagnosis of the anastomotic leak includes clinical signs (tachycardia, fever, pain radiating to shoulders, hypoxia, hemodynamic instability), urgent radiological investigations, such as CT of abdomen and upper gastrointestinal series with water-soluble contrast, or direct visualization of the leaking site on urgent laparoscopy or laparotomy in unstable patient. Urgent surgical exploration has an advantage of a possible mechanical closure of the defect or exact placement of drains in the desirable position. These leaks can generate an important amount of effluent and the correct drain position is paramount. Intraoperative flexible gastroscopy is imperative, as it allows to assess the location and extension of the defect, and to insufflate air or methylene blue into the stomach, permitting thus to identify any luminal connection with the abdominal cavity. Stable patients can be managed non-operatively, provided that an adequate drainage of the extraluminal collection is achieved. Typically, such extraluminal collections are drained externally under radiological guidance, CT or ultrasound, if no surgical drain is in place from the original procedure [3]. External drainage of an upper gastrointestinal leak can lead to formation of a chronic fistula, which can persist for a long time. Open RYGB represents a specific challenge in case of postoperative complication as created postoperative adhesions may preclude urgent laparoscopic exploration. Laparoscopic approach is preferred due to its lower morbidity. In the reported case, the performance of the exploration by less traumatic laparoscopic approach permitted to mobilize a morbidly obese patient and restart enteral feeding sooner, contributing in this way to a faster recovery. External drainage of the intraabdominal abscess was achieved by flexible gastroscopy, avoiding the risk of formation of external fistula. Other crucial components of management of gastrojejunal leak include parenteral or enteral nutrition via gastric remnant or jejunostomy and antibiotics.
Conclusion
Gastrojejunal anastomotic leakage following RYGB can be life threatening and difficult to manage. The present report describes a successful completely endoscopic management of a contained leak with a placement of nasogastric draining tube and enteral feeding via gastric remnant.
| References | ▴Top |
- Thodiyil PA, Yenumula P, Rogula T, Gorecki P, Fahoum B, Gourash W, Ramanathan R, et al. Selective nonoperative management of leaks after gastric bypass: lessons learned from 2675 consecutive patients.Ann Surg. 2008;248(5):782-792.
pubmed - Fernandez AZ, Jr., Demaria EJ, Tichansky DS, Kellum JM, Wolfe LG, Meador J, Sugerman HJ. Multivariate analysis of risk factors for death following gastric bypass for treatment of morbid obesity. Ann Surg. 2004;239(5):698-702; discussion 702-693.
pubmed - Csendes A, Burdiles P, Burgos AM, Maluenda F, Diaz JC. Conservative management of anastomotic leaks after 557 open gastric bypasses. Obes Surg. 2005;15(9):1252-1256.
pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


