| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 5, Number 2, February 2014, pages 58-61
Recurrent Rhinosporidiosis
Josue Cherya, b, Christopher Bacskaia, Ernesto Mendozaa
aDepartment of Surgery, New York Methodist Hospital, Brooklyn, New York, USA
bCorresponding author: Josue Chery, Department of Surgery, New York Methodist Hospital, 506 Sixth Street, Brooklyn, NY 11215, USA
Manuscript accepted for publication December 18, 2013
Short title: Recurrent Rhinosporidiosis
doi: https://doi.org/10.14740/jmc1637w
| Abstract | ▴Top |
Rhinosporidiosis is a rare, chronic granulomatous disease, caused by the parasite Rhinosporidium seeberi. While rare in the United Sates, the disease is prevalent in the Indian subcontinent; as such, increasing immigration from that region will change the prevalence of R. seeberi in the United States. We report a case of recurrent rhinosporidiosis in a Bangladeshian male affecting the nasopharynx. The patient is a 41-year-old male from Bangladesh, with a 20 pack year smoking history, who first presented to our office, 4 years ago, complaining of hoarseness and a “feeling of a lump” in his throat. His symptoms were progressive. He underwent surgical resection using combination of scapel and electrocautery. Pathology was consistent with rhinosporidiosis. He now presents, 4 years later, with similar complaints and a physical examination demonstrating a recurrent, flesh-like lesion. This time however, surgical excision was performed using the Harmonic™ scapel. Follow-up endoscopic evaluation 6 months after surgery showed no signs of a recurrent lesion. The mode of treatment for rhinosporidosis has widely been anecdotal without much literature. Wide local surgical electrocauterization is the treatment of choice with postoperative systematic dapsone that may be prescribed for up to 1 year. However, local recurrence remains a problem, likely secondary to auto-innoculation during the surgical trauma. Although rare in the United States, immigration from areas of the world where it exists increases the likelihood that the practicing head and neck specialist may encounter such disease entity in their practice. Familiarity with surgical and medical therapy will afford a more systematic approach for treating patients.
Keywords: Rhinosporidiosis; Recurrent; Surgical technique; Dapsone
| Introduction | ▴Top |
Rhinosporidiosis is a rare chronic granulomatous disease, caused by the parasite Rhinosporidium seeberi [1, 2]. It typically manifests as vascular polyps that arise from the upper respiratory tract. The disease is commonly found in the anterior nares, the inferior turbinates, septum and floor of the nasal cavity; however, it can also affect extranasal sites including the oral cavity, trachea and uvula [1, 3-9]. Rhinosporidiosis is usually a result of direct traumatic inoculation with the organism. Trauma from surgery has also been cited as potential mode of transmission [1, 5, 7, 8]. The disease progresses with local replication of R. seeberi and results in hyperplastic growth of host tissue and associated local immune response [1, 2].
The disease is prevalent mainly in Indian subcontinent [1, 8], and remains quite rare in the United States [2, 3, 5, 6, 9]. As such definitive guidelines regarding surgical and medical treatment are poorly covered in the literature. Although rare in the United States, immigration from areas of the world where it exists increases the likelihood that the practicing head and neck specialist may encounter such disease entity in their practice. Familiarity with surgical and medical therapy will afford a more systematic approach for treating patients. We report a case of recurrent rhinosporidiosis in a Bangladeshian male affecting the nasopharynx, who presented with globus pharyngeus and dysphonia and underwent surgical resection with the use of the Harmonic™ scapel. We report our clinical outcome.
| Case Report | ▴Top |
A 41-year-old male from Bangladesh, with a 20 pack year smoking history, first presented to our office, 4 years ago, complaining of hoarseness and a “feeling of a lump” in his throat that was progressive. At the time a nasopharyngeal lesion was identified and biopsied with a pathology consistent with rhinosporidosis. The nasopharyngeal lesion was then surgically removed, using a combination of #15 blade scapel and electrocautery, uneventfully. The patient presented a week later for his first postoperative follow-up, and his symptoms had much improved. We planned to have him followed up with our infectious disease collegues for further postoperative treatment; however, he was lost to follow up; until recently he presented to our office with similar complaints as he did 4 years earlier.
On examination, a flesh-like, reddish, exophytic and lobular mass was seen to occupy most of the oropharynx. The mass had a pedicle that stemmed from the nasopharynx, which suggested it to be its origin. The rest of his oral cavity was unremarkable. His trachea was midline, thyroid gland was normal and there were no cervical lymphadenopathy noted on palpation. Fiberoptic laryngoscopy was performed which confirmed the origin of the lesion to be arising from the posterior wall of the upper nasopharynx. The pedicle was roughly 3 cm in width. Further evaluation with a CT scan demonstrated a midline mass that appeared to be lobulated in the nasopharynx (Fig. 1). Given his symptoms and the size of the lesion, a decision was made to proceed with surgical resection.
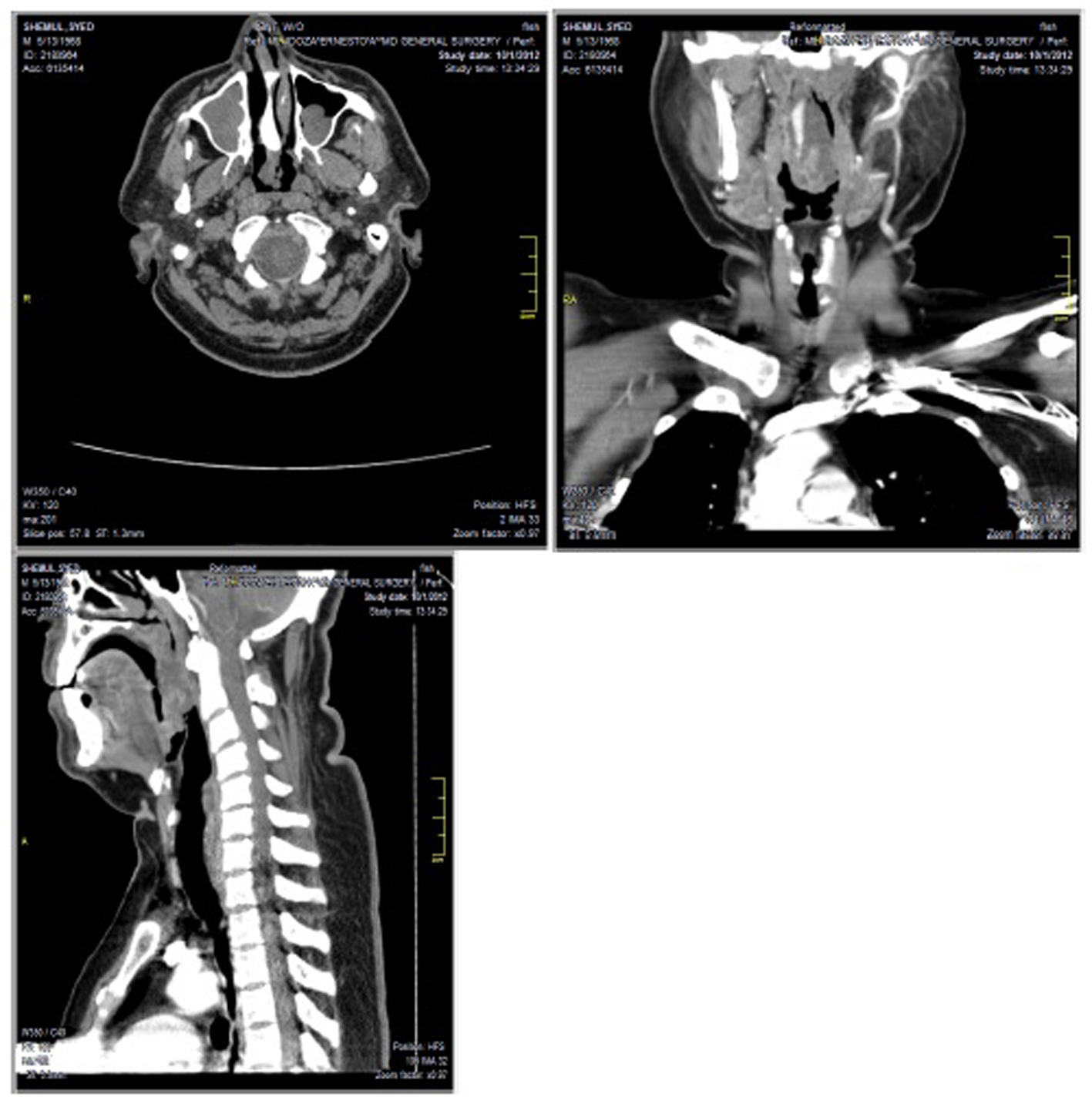 Click for large image | Figure 1. CT scan of transverse, coronal and saggital views demonstrating mass in nasopharynx. |
In the operating room, general anesthesia was induced after endotrachael intubation via fiber optic. Excision of the nasopharyngeal mass was performed transorally. With the patient in the supine position, self spreader was placed to open the mouth. Two #14 rubber catheters were placed through both nostrils in order to retract the soft palate. This maneuver exposed the root of the tumor in the nasopharynx. The Harmonic™ scapel was used to transect the lesion at the base of the pedicle, in its entirety. Surrounding tissues were noted to be intact without evidence of local trauma. Furthermore, inspection through the nose disclosed no evidence of nasal component.
On gross pathology, a moderalely firm, flesh-like mass was excised (Fig. 2). Microscopic evaluation identified sporangia and endopores (Fig. 3) demonstrating a granulomatous reaction with eosinophilia (Fig. 4). Final pathology is consistent with rhinosporidiosis with chronic inflammation and giant cell reaction. His postoperative course was unremarkable. Follow-up evaluation 6 months later with fiber optic laryngoscopy demonstrated no local recurrence, despite not using postoperative dapsone.
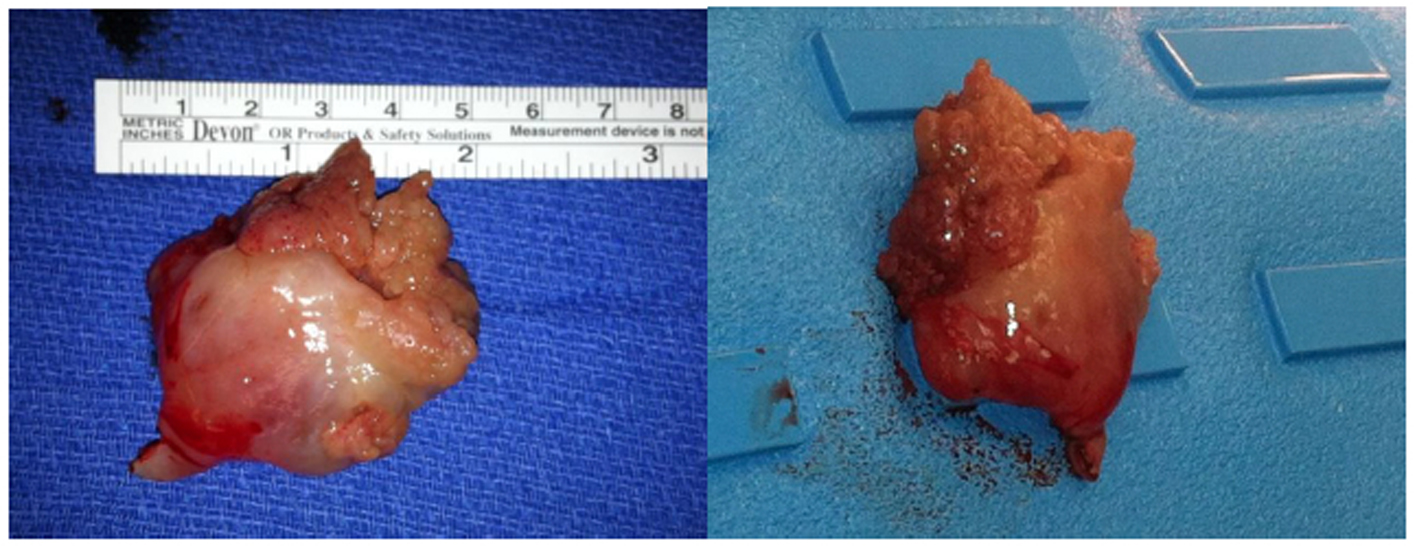 Click for large image | Figure 2. Pale-tan-like mass with focal papillary areas measuring 3.9 × 3.8 × 3.2 cm. |
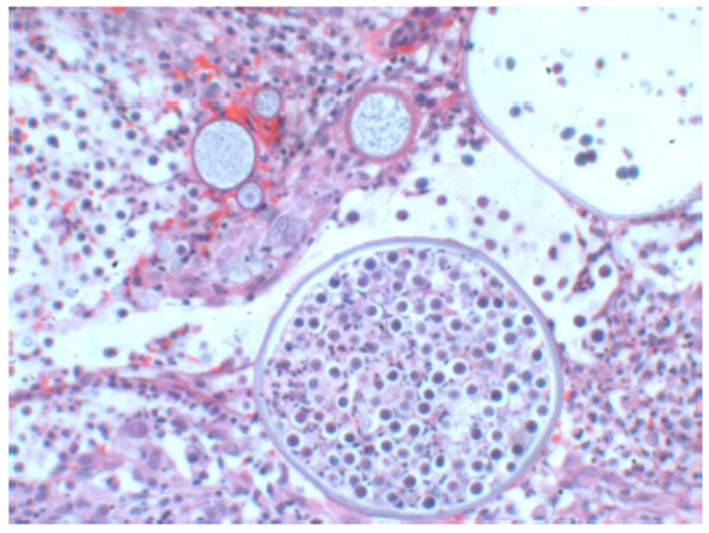 Click for large image | Figure 3. H&E sporigia and endospores (× 10). |
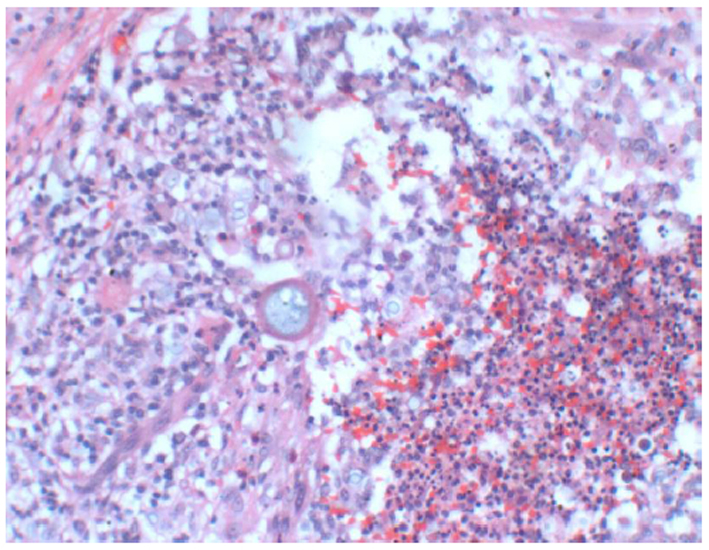 Click for large image | Figure 4. H&E granulomatous reaction and eosinophil (× 4). |
| Discussion | ▴Top |
We present a rare disease entity that the practicing head and neck surgeon may encounter, in light of immigration to the United States from the Indian subcontinent. The mode of treatment for rhinosporidosis has widely been anecdotal with little literature to support it. Wide local surgical electrocauterization of the base of the lesion is the treatment of choice [1-6, 8, 9]. Additionally, systematic dapsone may be prescribed for 1 year to prevent recurrence, as its mechanisnm has shown to arrest the maturation of sporangia and promote fibrosis in stroma [1-6, 8]. There is a greater paucity of literature for the treatment of recurrent disease.
Surgery is effective at removing the lesion; however, resection with electrocautery can potentially cause localized tissue trauma that potentiates the possibility for innoculation [1, 4, 7]. This may potentially explain the recurrence in our patient, as his initial surgical resection was with the use of electrocautery. It is unlikely that he had de novo innoculation of new spores, as the patient had not traveled outside of the country during that time frame and the parasite is not known to be spread between humans through casual contact [1]. While he presented to our office after 4 years, the mass had been growing for couple of years prior. However, his symptoms had been manageable, hence his reluctance to seek medical help.
The patient had an uneventful surgical resection with the use of the Harmonic™ scapel. The Harmonic™ scapel has been described in the literature to have superior hemostasis while preserving the integrity of local tissue [10]. We believe that it played a key role in the lack of recurrence despite the patient’s non-adherence to postoperative dapsone treatment.
Conclusion
With increased immigration from regions where rhinosporidiosis is endemic, knowledge of the disease and treatment is paramount. In this case report, in an immigrant from Bangladesh, the identificaiton of recurrent rhinosporidiosis re-emphasized the importance of combined surgical and medical treatment to decrease local recurrence. However, pathogen as well as pathophysiology of this disease entity needs to be further elucidated in order to provide more effective and directed therapy.
Grant Support
No grants were used for this case report.
Conflict of Interest
The authors claim no conflict of interest.
| References | ▴Top |
- seculeratne SN. Recent advances in rhinosporidiosis and Rhinosporidium seeberi. Indian J Med Microbiol. 2002;20(3):119-131.
pubmed - Ayub-ur-Rehman, Muhammad MN, Moallam FA. Rhinosporidiosis. J Coll Physicians Surg Pak. 2012;22(10):671-672.
pubmed - Sonkhya N, Singhal P, Mishra P. Naso-oropharyngeal rhinosporidiosis: endoscopic removal. Indian J Otolaryngol Head Neck Surg. 2005;57(4):354-356.
pubmed - Uledi S, Fauzia A. Human nasal rhinosporidiosis: a case report from Malawi. Pan Afr Med J. 2011;9:27.
pubmed - Rajeshwari A, Gangadhaia S, Deviprasad S, Manohar S. Rhinosporisiosis - a report of two cases. Indian J Otolaryngol Head Neck Surg. 2010;62(3):322-325.
doi pubmed - Puri R, Berry S, Mandal AK, Berry N. Isolated trachael rhinosporidiosis - a case report. Indian J Otolaryngol Head Neck Surg. 2000;52(4):380-381.
pubmed - Mathew J, Padhy S, Lata S, Balchander H, Gopalakrishnan S. Telelaryngoscopy-guided flexible fiberoptic intubation for laryngeal rhinosporidiosis. Int Anesthesia Res Soc. 2010;110(4):1066-1068.
- Das S, Kashyap B, Barua M, Gupta N, Saha R, Vaid L, Banka A. Nasal rhinosporidiosis in humans: new interpretations and a review of the literature of this enigmatic disease. Med Mycol. 2011;49(3):311-315.
doi pubmed - Ali A, Flieder D, Guiter G, Hoda SA. Rhinosporidiosis: an unusual affliction. Arch Pathol Lab Med. 2001;125(10):1392-1393.
pubmed - Collison PJ, Weiner R. Harmonic scalpel versus conventional tonsillectomy: a double-blind clinical trial. Ear Nose Throat J. 2004;83(10):707-710.
pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


