| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 2, Number 2, April 2011, pages 48-50
A Case of Squamous Cell Carcinoma Developed in Chronic Tuberculous Empyema Following Therapeutic Extrapleural Pneumothorax
Hiroyuki Kamiya
Division of Respiratory Medicine, Japanese Red Cross Medical Center, 4-1-22, Hiroo Shibuya-ku, Tokyo 150-8935, Japan
Manuscript accepted for publication January 13, 2011
Short title: Carcinoma in Chronic Tuberculous Empyema
doi: https://doi.org/10.4021/jmc125w
| Abstract | ▴Top |
A 72-year-old woman was admitted to our hospital for persistent right-sided chest pain for 6 months and osteolytic changes in some ribs on chest x-rays. The patient had a past history of pulmonary tuberculosis at 19 years of age and underwent treatment for right-sided therapeutic extrapulmonary pneumothorax. A computed tomography (CT) scan of her chest demonstrated a ring-enhanced tumor adjacent to the chronic empyema, which invaded the thoracic wall and eroded some ribs. A poorly differentiated squamous cell carcinoma (SCC) was pathologically diagnosed by percutaneous CT-guided biopsy. Radiation therapy with a total dose of 74.4 Gy was performed instead of surgical resection considering poor pulmonary function. The efficacy of the treatment was confirmed by positron emission tomography (PET) scanning with 18-fluorodeoxyglucose (18FDG), which demonstrated a reduction both in the size and the standardized uptake value (SUV) at the hot spot at the invasive site of the tumor to the thoracic wall. This case was recognized as SCC developed in chronic tuberculous empyema since the tumor had only contacted with the empyema and the lung parenchyma surrounding the empyema was intact.
Keywords: Chronic tuberculous empyema; Extrapleural pneumothorax; Squamous cell carcinoma
| Introduction | ▴Top |
It is widely believed that chronic tuberculous empyema possibly undergoes some complications years later, such as recurrence of tuberculosis, secondary infection and some malignant tumors. The case presented here is of the tumor complicated in chronic tuberculous empyema following therapeutic extrapleural pneumothorax.
| Case Report | ▴Top |
A 72-year-old woman was referred to our hospital and admitted to evaluate her persistent right-sided chest pain. She first visited her physician for her symptom 6 months before, and had been closely followed up although no abnormalities were detected excluding a right-sided calcified chronic empyema.
The patient had a past history of right-sided therapeutic extrapulmonary pneumothorax for pulmonary tuberculosis at 19 years of age.
On admission, she was afebrile and physical examination showed no particular abnormalities although her laboratory data showed both C-reactive protein (CRP) and the erythrocyte sedimentation rate (ESR) were slightly elevated, 1.21 mg/dL and 19 mm/h, respectively. Carcinoembryonic antigen (CEA) was also slightly elevated (7.4 ng/ml), but no other abnormal laboratory findings were detected. Her chest x-ray on admission demonstrated a right-sided pleural thickening with calcification and osteolytic changes in both the 5th and 6th ribs (Fig. 1). A CT scan of her chest demonstrated a right-sided calcified empyema and a ring-enhanced tumor adjacent to it, which had invaded the thoracic wall and eroded some ribs (Fig. 2). Positron emission tomography (PET) scanning with 18-fluorodeoxyglucose (18FDG) demonstrated a crescent-like hot spot at the invasive site of the tumor to the thoracic wall, which was suggestive of a viable lesion of the tumor and it retained continuity from the empyema (Fig. 3).
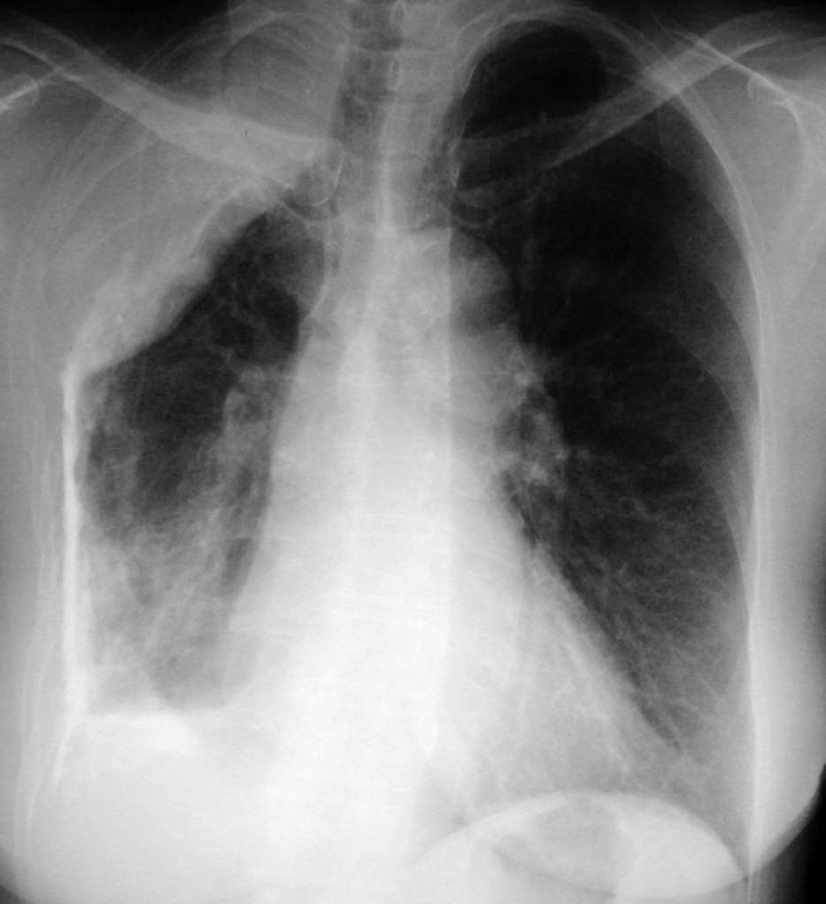 Click for large image | Figure 1. Chest x-ray film on admission shows right-sided pleural calcification and osteolytic changes in the 5th and 6th ribs. |
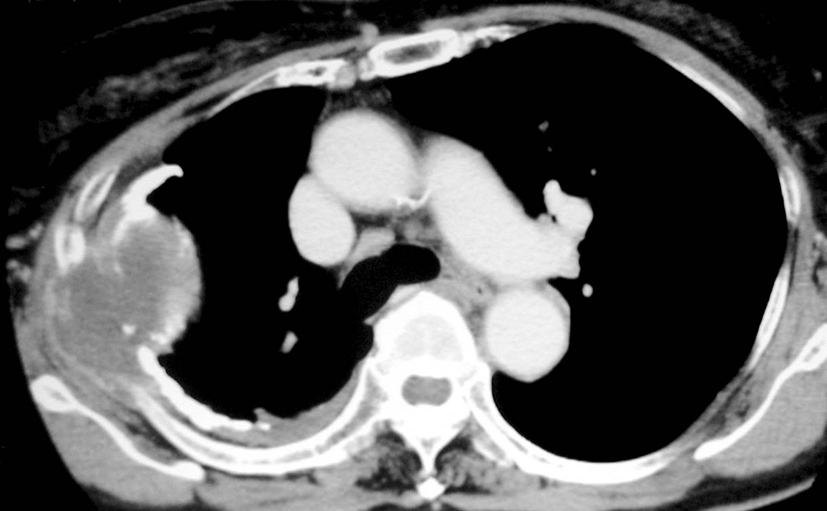 Click for large image | Figure 2. Chest CT scan on admission shows right-sided pleural empyema with calcification and a ring-enhanced tumor adjacent to it, which invades the thoracic wall and erodes some ribs. |
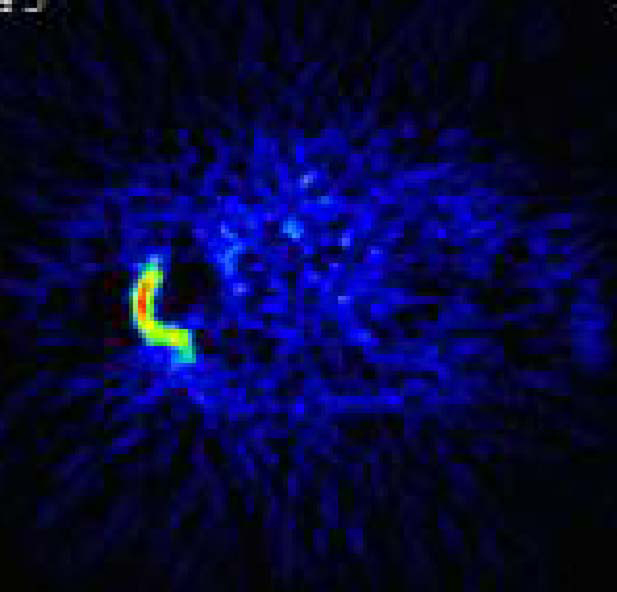 Click for large image | Figure 3. PET with 18FDG scan before treatment shows a crescent-like hot spot at the invasive site of the tumor to the thoracic wall. |
Percutaneous CT-guided biopsy was performed on the tumor and histological examination of the specimen disclosed that atypical cells with enlarged nuclei and abundant cytoplasm formed a sheet-like solid nest with no apparent keratinization (Fig. 4). Immunohistological staining confirmed the diagnosis as poorly differentiated squamous cell carcinoma, which was supposed to have originated in the chronic tuberculous empyema since the tumor had only contacted with the empyema and the lung parenchyma surrounding the empyema was intact.
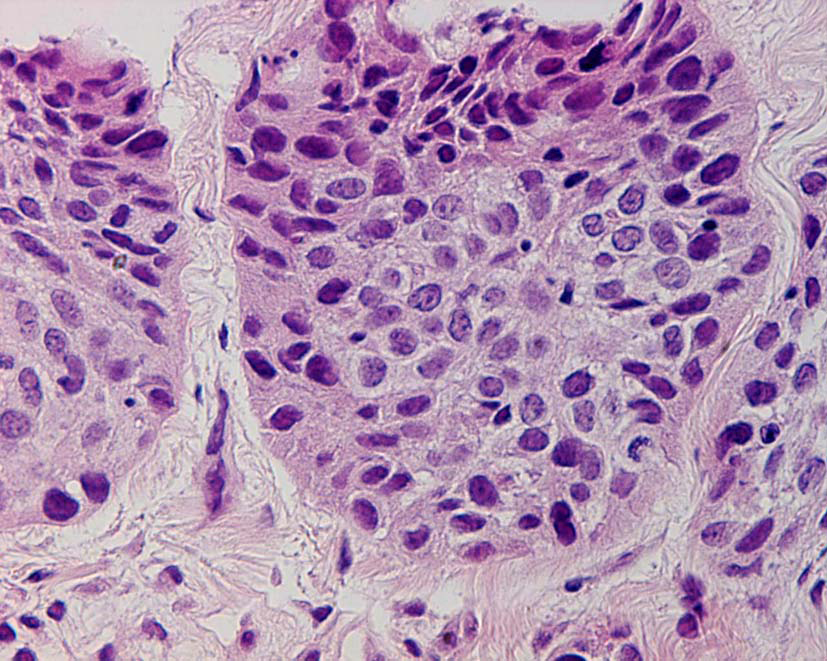 Click for large image | Figure 4. Histological examination of the tumor revealed that atypical cells with enlarged nuclei and abundant cytoplasm formed a sheet-like solid nest with no apparent keratinization. |
Given that the tumor was localized and pulmonary function was poorly damaged, radiation therapy was performed using an accelerated hyperfractionated method. A PET scan with 18FDG three months after the total dose of 74.4 Gy of radiation was administered demonstrated a reduction in the size of the hot spot and the standardized uptake value (SUV) of the spot was decreased from 6.1 g/mL to 2.8 g/mL, which was supposed to indicate some beneficial effect of the treatment. However, the tumor began to recur a few months later and the patient was expired in about one year.
| Discussion | ▴Top |
It is widely recognized that nonepithelial tumors can be complicated with chronic empyema [1], while only a few dozen cases of epithelial tumors associated with it have been reported so far [2-11], and most of those tumors are squamous cell carcinomas.
Most cases in those tumors usually have a long history of empyema lasting about a few decades and the patient in this case also had a long history, about 50 years, of tuberculous empyema. Cattaneo et al [12] described the importance of long-standing chronic inflammation inside the empyema to cause the development of a malignancy in the empyema cavity.
Deaton et al [13] described the origin of the squamous cell in pleural cavity. If there is a cutaneous or bronchial fistula with pleural cavity, it is possible that epithelium of the skin develops through a pleurocutaneous fistula or that bronchial epithelial metaplasia into squamous cell develops through a bronchopleural fistula. However, in cases without any those fistulas, squamous cell carcinoma might arise from the skin fragments that could enter the pleural space at repeated air refills during therapeutic extrapulmonary pneumothorax [3, 5, 6] or mesothelial metaplasia into squamous cell [13]. Squamous cell carcinoma in this case is supposed to have originated from mesothelial metaplasia because no fistula was detected and highly differentiated changes like keratinization should have been presented if it arises from the skin fragments.
Osteolytic changes on chest x-rays led us to the diagnosis in this case, but a chest CT scan will be usually required to evaluate small changes in the thoracic cavity. An enhanced mass adjacent to empyema or nodular pleural thickening on a chest CT scan is suggestive of malignancy complicated with chronic empyema [14]. Watanabe et al reported two types of tumor findings in the literature [7], mass formation type and scattered foci type, and radiological findings in this case were compatible with the former.
Although the localized tumor should be preferentially treated surgically, most tumors complicated with chronic tuberculous empyema will be inoperable because of poor pulmonary function. However, radiation therapy should be a therapeutic candidate, especially when the tumor is squamous cell carcinoma, which is often sensitive to the treatment and this assumption was partly proved by the beneficial results obtained in this case.
In summary, we suggest that we should remember the development of squamous cell carcinoma in the differential diagnosis of the tumor associated with chronic tuberculous empyema following therapeutic extrapleural pneumothorax although it may be a rare case.
| References | ▴Top |
- Tamura A, Hebisawa A, Sagara Y, Suzuki J, Masuda K, Baba M, Nagai H, et al. [Thoracic malignancies in patients with chronic tuberculous empyema]. Kekkaku 2004;79(4):301-307.
pubmed - McAnally AA, Dockerty MB. Carcinoma developing in chronic draining cutaneous sinuses and fistulas. Surg Gynecol Obstet 1949;88(1):87-96.
pubmed - Bruce T, Dahlstrom G, Uggla LG. Squamous epithelial cancer of the pleura following extrapleural pneumothorax for pulmonary tuberculosis. Acta Tuberc Scand 1960;38:261-266.
pubmed - Willen R, Bruce T, Dahlstrom G, Dubiel WT. Squamous epithelial cancer in metaplastic pleura following extrapleural pneumothorax for pulmonary tuberculosis. Virchows Arch A Pathol Anat Histol 1976;370(3):225-231.
pubmed doi - Ruttner JR, Heinzl S. Squamous-cell carcinoma of the pleura. Thorax 1977;32(4):497-500.
pubmed doi - Rena O, Casadio C, Maggi G. Primitive squamous-cell carcinoma after extrapleural pneumothorax for active tuberculosis. Eur J Cardiothorac Surg 2001;19(1):92-95.
pubmed doi - Watanabe S, Yamaoka A, Sakasegawa K, Saigenji H, Shimokawa S, Taira A. Squamous cell carcinoma arising in chronic empyema cavity. Case report with review of the literature. Jpn J Chest Surg 1999;13(1):42-47.
- Dharkar DD, Leininger BJ, Kraft JR. Primary squamous cell carcinoma of pleura. IMJ Ill Med J 1986;170(1):27-29.
pubmed - Prabhakar G, Mitchell IM, Guha T, Norton R. Squamous cell carcinoma of the pleura following bronchopleural fistula. Thorax 1989;44(12):1053-1054.
pubmed doi - Aisaka H, Hirasawa M, Sakon O, Otsuka M, Ouchi H, Kurokawa K, Sugaya F, et al. A case of squamous cell carcinoma of the chest wall in a patient with chronic empyema. J Jpn Soc Bronchosc 2001;23(1):64-68.
- Caviria JZ, Franco CEG, Hiscock LJ, Pascual RP, Calvo LF, Trueba IM, Viguera JL. Carcinoma arising in the pleural cavity following pneumonectomy for hydatid disease. Respiration 2004;71(3):285-288.
pubmed doi - Cattaneo SM, Klassen KP. Letter: Carcinoma of the chest wall complicating chronically draining empyema. Chest 1973;64(5):673-674.
pubmed doi - Deaton WR, Jr. Carcinoma arising in chronic empyema cavity. Case report with review of the literature. Dis Chest 1962;42:563-566.
pubmed - Minami M, Kawauchi N, Yoshikawa K, Itai Y, Kokubo T, Iguchi M, Masuyama S, et al. Malignancy associated with chronic empyema: radiologic assessment. Radiology 1991;178(2):417-423.
pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


