| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 3, Number 3, June 2012, pages 164-166
Unilateral Diaphragm Paralysis Following Vaccination
George S. Habib
Department of Medicine, Carmel Medical Center, Haifa 34362, Israel
Manuscript accepted for publication January 13, 2012
Short title: Diaphragm Paralysis and Vaccination
doi: https://doi.org/10.4021/jmc516w
| Abstract | ▴Top |
Unilateral diaphragm paralysis (UDP) is relatively a rare entity. Currently, phrenic nerve injury following cardiac surgery is probably the most common cause. Here we report a case of symptomatic UDP that developed 5 days following vaccination against polio, Diphtheria (both subcutaneously), hepatitis A and abdominal typhus (intramuscularly). He had no fever or other neurological symptoms or signs. There is only one case report in the literature of UDP following immunization or vaccination with oral polio and triple DTP in a 6 month-old female. In contrast to our patient, here there was evidence of active polio disease with isolation of polio strains from her stool.
Keywords: Diaphragmatic paralysis; Unilateral; Vaccination
| Introduction | ▴Top |
Unilateral diaphragm paralysis (UDP) is relatively a rare entity. Currently, phrenic nerve injury following cardiac surgery is probably the most common cause [1]. Other causes include cervical spondylosis [2], compressive tumors [3], trauma [4], herpes zoster [5], poliomyelitis [6], pneumonia and others. However many cases of UDP remain idiopathic [4].
Patients with UDP but without underlying lung disease are usually asymptomatic at rest, however may have dyspnea on effort or while in supine position. An elevated hemi-diaphragm on chest x-ray is suggestive of the diagnosis that can be confirmed with fluoroscopic sniff test with paradoxical movement of the paralyzed hemi-diaphragm with inspiration. Pulmonary function test usually shows reduced vital capacity of 70-80% of predicted normal values. The prognosis of UDP in idiopathic cases is usually fair. Most cases generally lead a normal life and some cases may recover spontaneously.
Here we report a case of UDP following vaccination against polio, Diphtheria, hepatitis A virus and typhus prior to a planned trip to India in a 62-year-old male physician.
| Case Report | ▴Top |
Sixty-two year old man, who works as a physician and has controlled diabetes (HgA1C < 6.6), hypertension and gout, received vaccination against polio (IPV- immovax, Aventis, France) given subcutaneously, Diphtheria (dT-immovax, Aventis, France) given intramuscularly and against hepatitis A virus and abdominal typhus (Hepatyrix, GSK, Belgium) given intramuscularly before a planned visit to India, 5 days following the vaccination, patient started to complain of orthopnea and shortness of breath on effort without cough, fever or chest pain. Eventually, the patient traveled to India for one week and came back with the same complains without progression, 3 weeks after the start of symptoms patient was referred to the hospital and admitted for evaluation. His medications included aturvastatin, metformin, doxazocin, allopurinol, amlodipine, vitamin E, and candisartan. On physical examination, while in sitting position, patient was without stress or cyanosis and had breath count of 12 per minute. Jugular venous pressure was normal. Heart sounds normal. Decreased breath sounds at the right lung base and dullness on percussion. The rest of the physical examination was negative. Routine complete blood count and chemistry were normal. Blood gases showed arterial oxygen saturation of 95% in room air, arterial PCO2 of 41 mmHg. Electrocardiogram and echocardiogram were normal.
Chest x-ray showed elevated right diaphragm with evidence of no movement on fluoroscopy (Fig. 1). Computerized tomography of the neck and chest showed no evidence of tumor but right diaphragm paralysis. Electromyogram (EMG) of the upper extremities was negative for neuropathy or myopathy.
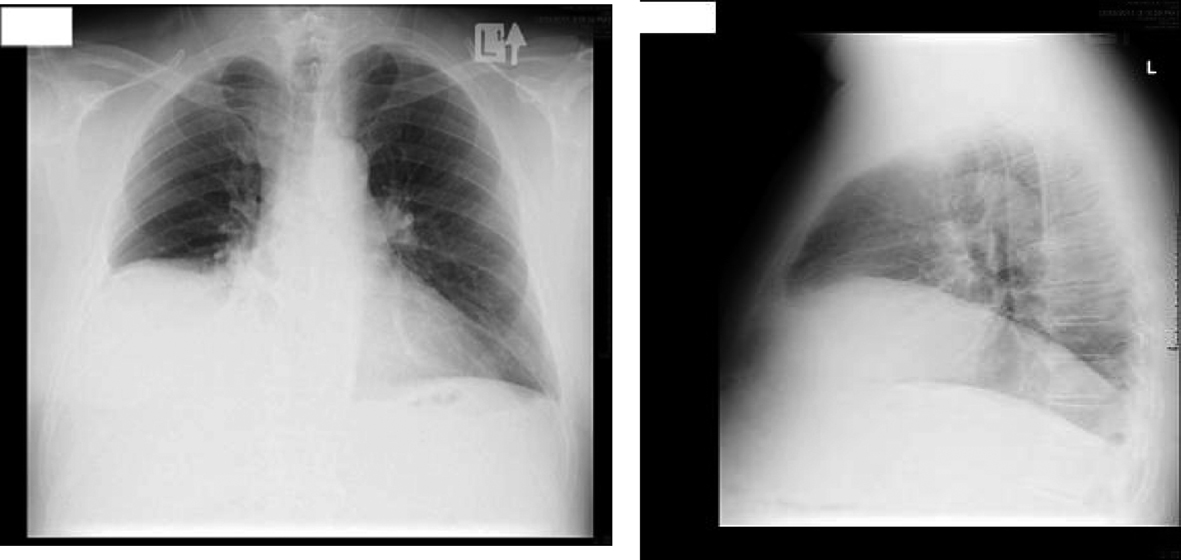 Click for large image | Figure 1. Antero-posterior and lateral views of chest x-ray of the patient. |
Pulmonary function test showed an abnormal restrictive pattern with FEV1 of 1.52 liters (43% of predicted value), and FVC 2.12 liters (46.7% of predicted value). FEV1: FVC ratio of 71.82%, total lung capacity of 4.42 liters (59.2% of predictive value), and residual volume of 2.07 liters (82.3% of predictive value).
Patient was evaluated by neurologist who found no evidence neuropathy or myopathy of any source.
Follow-up after 3 months without subjective or chest x-ray changes and repeated pulmonary function tests showed no change in volume or flow parameters.
| Discussion | ▴Top |
The cause of the UDP in this patient is not clear. The temporal relationship with the vaccination makes the association very suspicious.
There is only a single case report of UDP following immunization in the literature [7]. A 6-month-old female who developed fever and flaccid paralysis of all limbs and right diaphragm following immunization with oral polio and triple (DTP) vaccines. Poliovirus types isolated from her stool matched with the vaccine strains. This case illustrates the development of full blown polio. The polio virus immunization in our patient is a dead virus and there was no evidence of the development of acute infection of polio or other infection in our patient.
There are no reports of diaphragmatic paralysis following Typhus or hepatitis A virus infection. There is one report of diaphragmatic paralysis in a 3-week-old infant following acute infection with diphtheria [8].
Our patient had diabetes, a disease that could be complicated with neuropathy or myopathy. However, he had no symptoms, sings or EMG findings suggestive of neuropathy. In the literature, there is one report of reversible unilateral right diaphragmatic hemi-paralysis in a 52-year-old female with diabetic neuropathy [9].
In my opinion, the most likely explanation in our case is a neurological adverse effect affecting the phrenic nerve following vaccination. Neurological adverse effect post vaccination were reported, especially encephalomyelitis following different types of immunization including diphtheria-tetanus-polio and others [10]. A coincidental event cannot be ruled out.
Conflict of Interests
None.
Funding
None.
| References | ▴Top |
- Canbaz S, Turgut N, Halici U, Balci K, Ege T, Duran E. Electrophysiological evaluation of phrenic nerve injury during cardiac surgery—a prospective, controlled, clinical study. BMC Surg. 2004;4:2.
pubmed - Hayashi H, Kihara S, Hoshimaru M, Hashimoto N. Diaphragmatic paralysis caused by cervical spondylosis. Case report. J Neurosurg Spine. 2005;2(5):604-607.
pubmed doi - Kara M, Isik M, Ozcakar L, Erol O, Dogan S, Altundag K, Aksu S. Unilateral diaphragm paralysis possibly due to cervical spine involvement in multiple myeloma. Med Princ Pract. 2006;15(3):242-244.
pubmed doi - Elefteriades J, Singh M, Tang P, Siegel MD, Kenney B, Pandey A, Kopf GS. Unilateral diaphragm paralysis: etiology, impact, and natural history. J Cardiovasc Surg (Torino). 2008;49(2):289-295.
pubmed - Bahadir C, Kalpakcioglu AB, Kurtulus D. Unilateral diaphragmatic paralysis and segmental motor paresis following herpes zoster. Muscle Nerve. 2008;38(2):1070-1073.
pubmed doi - Imai T, Matsumoto H. Insidious phrenic nerve involvement in postpolio syndrome. Intern Med. 2006;45(8):563-564.
pubmed doi - Asindi AA, Bell EJ, Browning MJ, Stephenson JB. Vaccine-induced polioencephalomyelitis in Scotland. Scott Med J. 1988;33(4):306-307.
pubmed - Staudt F, Hess HJ. [Diphtheria in an infant]. Padiatr Padol. 1993;28(2):51-54.
pubmed - Kadosh S, Qupti G, Flatau E. [Unilateral diaphragmatic paralysis in a diabetes patient]. Harefuah. 2005;144(12):834-835, 911.
pubmed - Huynh W, Cordato DJ, Kehdi E, Masters LT, Dedousis C. Post-vaccination encephalomyelitis: literature review and illustrative case. J Clin Neurosci. 2008;15(12):1315-1322.
pubmed doi
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


