| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 15, Number 4-5, May 2024, pages 92-96
Long Segment Colon Degloving From Blunt Abdominal Trauma
Aldin Malkoca, c, Lana Mamounb, Harpreet Gilla, Danielle Cremata, Gbemisola Lawala, William Shermana
aArrowhead Regional Medical Center, Colton, CA 92324, USA
bCalifornia University of Science and Medicine, Colton, CA 92324, USA
cCorresponding Author: Aldin Malkoc, Arrowhead Regional Medical Center, Colton, CA 92324, USA
Manuscript submitted March 25, 2024, accepted April 24, 2024, published online May 2, 2024
Short title: Long Segment Colon Degloving
doi: https://doi.org/10.14740/jmc4205
| Abstract | ▴Top |
It is extremely rare for blunt abdominal trauma to result in serious injuries to hollow organs. Degloving injuries of the colon are one of the rarest injuries following blunt abdominal trauma. Intestinal degloving is often seen following rapid deceleration, changes in velocity, crushes and motor vehicle collisions (MVCs). Victims with intestinal degloving injuries can experience vague symptoms despite the severity of the lesion. We present the case of a 21-year-old male with insulin-dependent type 1 diabetes who was involved in a high-speed MVC. He sustained second- and third-degree burns to the extremities, right carotid artery dissection, and multiple fractures to the mandible, pelvis and forearm. Free fluid was also noted in the pelvis prompting an emergent exploratory laparotomy. In the operating room, he was found to have a cecal serosal injury involving more than 50% of the circumference and a sigmoid and descending colon degloving injury of 50 cm. The injured segments were resected, and primary anastomoses were created. Degloving of the colon is extremely rare and the sigmoid is one of the more frequently documented locations of injury. Our case contributes to the limited literature available pertaining to the treatment of evolution of these severe colon injuries.
Keywords: Colon; Degloving; Abdominal trauma
| Introduction | ▴Top |
Degloving injuries of the colon from blunt abdominal trauma are a rare occurrence and several different mechanisms have been proposed. One thought is that mobile portions of the intestine may tear away from fixed portions of the intestines, resulting in full thickness lacerations and degloving of the bowel and omentum [1]. Lacerations, mesenteric avulsions, and intestinal degloving have also been noted after sudden deceleration events leading to a rise in intra-abdominal pressure, shearing, and compression [1-4]. Often patients present with vague symptoms such as abdominal tenderness, ecchymoses across the anterior abdomen and vital signs are often normal [3]. Thus, early identification of this injury is key for patient survival. This case describes colonic degloving injuries suffered by a young man after a high-speed motor vehicle collision (MVC) that also resulted in multiple associated injuries including a carotid artery dissection, second- and third-degree burns, mandibular fracture, and multiple orthopedic injuries.
| Case Report | ▴Top |
A 21-year-old male with a history of type I diabetes presented to the emergency department after a high-speed single MVC at approximately 80 miles/h into a fixed object. On arrival, he had a Glasgow Coma Scale (GCS) 15 and was complaining of abdominal pain, bilateral hip pain, and facial pain. Physical exam on arrival was significant for mild tenderness to palpation in the bilateral lower quadrants of the abdomen as well as mixed second and third burns of the bilateral thighs and left hand. The patient’s initial vital signs were blood pressure 102/83 mm Hg, pulse rate 102 beats per minute, temperature 97.9 °F, respiratory rate 18 breaths per minute, and oxygen saturation 94% on room air. Laboratory evaluation was significant for leukocytosis of 20.3 × 103/µL (normal 4,300 - 11,000), hyperglycemia of 410 mg/dL (normal: 70 - 100), and hypocalcemia with ionized calcium of 1.00 mmol/L (normal 1.2 - 1.3). Initial arterial blood gas demonstrated metabolic acidosis with pH 7.22 (normal 7.35 - 7.45), bicarbonate of 14.4 mmol/L (normal 22 - 26), base excess of -12.8 mmol/L (normal -2 - 2), and lactate of 4.96 mmol/L (normal 0 - 2). Chest and pelvic X-rays demonstrated no pneumothorax or rib fractures but right acetabulum and ilium fractures with displacement. Computed tomography (CT) scans redemonstrated right ilium fracture with right hip posterior dislocation along with left sacrum fracture, pelvic free fluid with mild bowel edema in the left lower quadrant, right internal carotid artery dissection, and comminuted fracture of the mandible. No concern of degloving injury was suspected at this time based on the CT findings.
He was taken emergently for an exploratory laparotomy given the presence of pelvic free fluid. The patient was found to have a cecal serosal injury involving greater than 50% of the circumference for a length of 8 cm, as well as a descending and sigmoid degloving injury for 50 cm with an associated bucket-handle injury of the mesentery (Fig. 1). The injured portion of the cecum was resected, and a stapled side-to-side functional end-to-end anastomosis was created. The injured left colon was resected and a side-to-side isoperistaltic stapled anastomosis created. The abdomen was closed primarily. Prior to leaving the operating room, third-degree burns were noted to the bilateral thighs as well as the left hand and fingers; the wounds were cleansed and dressed with Polysporin and Xeroform before being wrapped with Kerlix. Orthopedics was consulted intraoperatively for reduction of the right hip. A Steinmann pin was placed in the right leg along with traction and plans for definitive repair.
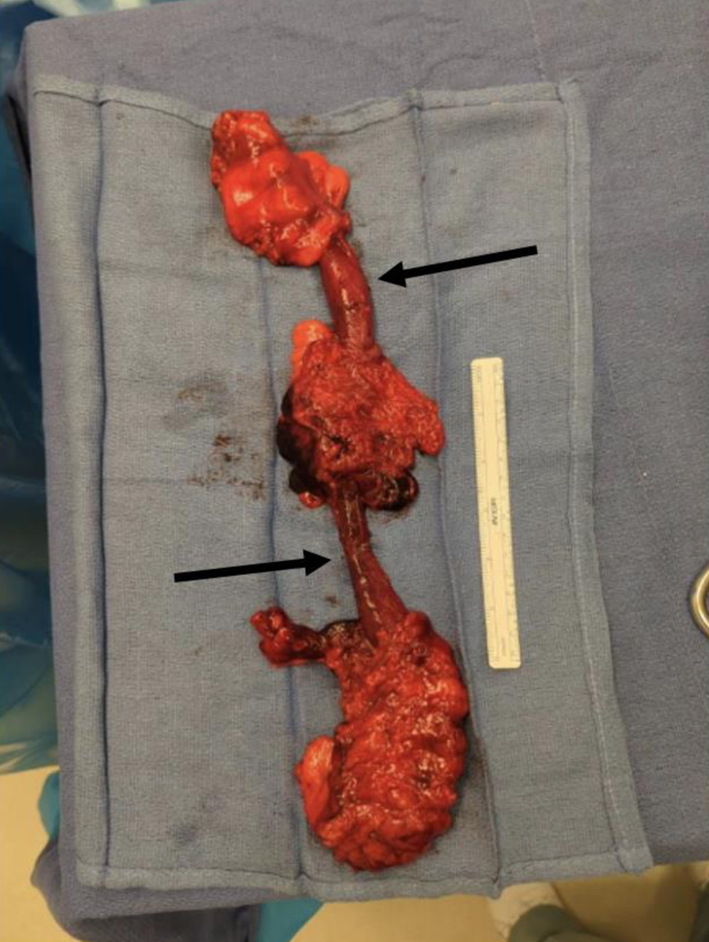 Click for large image | Figure 1. Degloved injury of the colon. The black arrows represent the degloved portion of the colon without any mesentery attached to it. |
Postoperatively, he remained intubated and was admitted to the surgical intensive care unit (SICU). He was placed on a heparin drip due to the right carotid artery dissection and an insulin drip for uncontrolled hyperglycemia. Tube feeds were started at a trickle rate of 20 mL/h. Tertiary exam in the SICU identified a left mid-shaft ulnar fracture and a right occipital condyle fracture. He continued to receive daily wound care for his burn wounds. He returned to the operating room multiple times with orthopedic surgery, burn surgery, and oral-maxillofacial surgery to address his various injuries.
The patient was extubated on hospital day 8 without complication. Tube feeds were started; however, there was difficulty tolerating tube feeds due to the patient’s diabetic gastroparesis. He was eventually advanced to a ground diet on hospital day 21. He remained on the insulin drip intermittently and 5 days before discharge he was placed back on subcutaneous insulin with improved control of his blood sugars. He was discharged to acute rehab per the recommendations of physical and occupational therapy. He is doing well outpatient with regular follow-up in the surgery clinic.
| Discussion | ▴Top |
Blunt abdominal trauma is much more likely to result in solid organ injury rather than small or large intestinal injury. Of reported blunt intestinal injuries, the small intestine accounts for the majority [4, 5]. Degloving injuries occur when the muscle and mesentery of the colon is stripped away, leaving behind only the mucosa. A significant amount of shearing force is required for degloving to occur. The blood supply is lost with the compromise of the mesentery, leading to ischemia and necrosis [3, 4]. Despite its severity, patients often present with vague symptoms such as abdominal tenderness or ecchymoses [3-6]. Ultrasound of the abdomen is associated with human error and it should not be the sole diagnostic method for blunt abdominal trauma and degloving of the colon [2, 4]. Contrast CT scans and laparotomy reveal the true severity of these injuries [2, 4, 5, 7]. Prompt identification of such injuries can result in improved mortality and morbidity [7-9].
In Table 1, we summarize literature on patients with degloving injuries, their demographics, the specific location of injury and their respective managements [3, 4, 6, 9-16]. Reported degloving injuries most often result after MVCs but have been found to occur after falls and crush injuries as well. The most common location for degloving injury is the sigmoid colon followed by the ascending and descending colons (Fig. 2). The most common reported intervention is resection and colostomy (75%) with a handful of cases repaired with primary anastomosis (Table 1). Additionally, the importance of pre-operative antibiotics and early bowel feeding is important as was performed in this patient [17, 18].
 Click to view | Table 1. A Summary of Literature on Reported Cases of Degloving of the Colon and Their Repair Type [3, 4, 6, 9-16] |
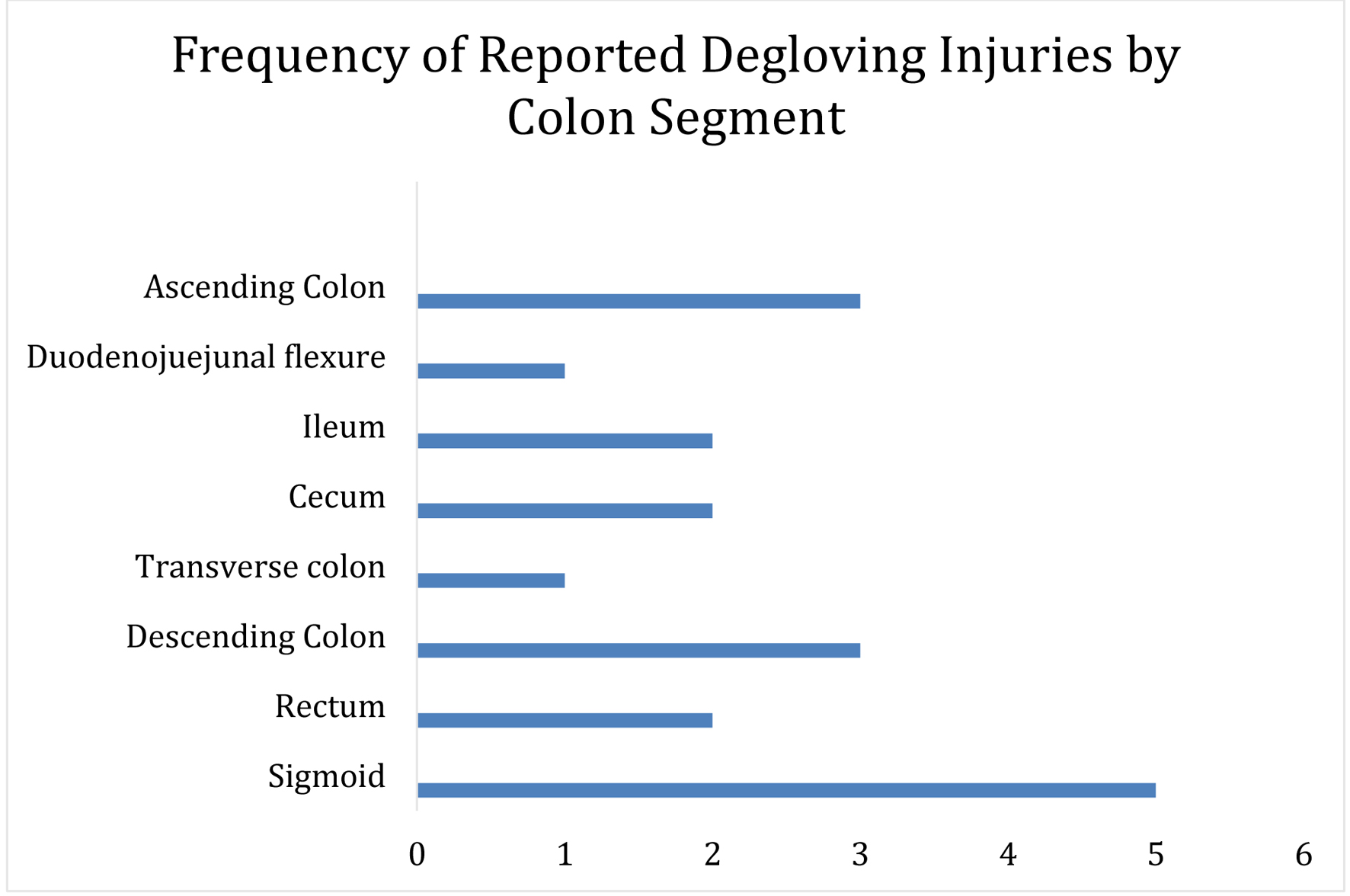 Click for large image | Figure 2. Graphical version of the various segments of colon injury that are reported. |
Management of colon injuries following blunt abdominal trauma varies depending on the severity of the trauma. Kordzadeh et al [2] and Stefanou et al [19] emphasized the importance of immediate intervention in unstable patients with blunt abdominal trauma because of its low risk of infection and reduction of blood loss. Bege et al stated the management of hollow visceral organ injuries begins with determining the patient’s hemodynamic status and confirmation with a CT scan prior to surgical intervention. They also indicated that the lack of abdominal free fluid can warrant nonsurgical methods, with an emphasis on close monitoring of the patient [5]. In the case of our patient, earlier surgical management is the most optimal option as it allows for the most definitive management regarding the patient’s bowel injury.
In the case of our patient, he had a minor seatbelt sign that was noted on his secondary survey. He underwent prompt evaluation and was taken rapidly to the operating room after CT findings of abdominal free fluid and bowel edema. There was no feculent contamination within the abdomen and he was able to undergo primary anastomosis. This patient had a long segment of bowel with degloving injury to the colon that has not been yet reported in the literature. He suffered a multitude of other injuries as well, likely due to the high impact of his MVC. Other surgical services - neurosurgery, orthopedic surgery, burn surgery, and oral maxillofacial surgery - were all involved in a timely manner.
Learning points
Blunt trauma accounts for less than 5% of all intestinal injuries. Degloving of the colon is one of the rarest forms of documented blunt abdominal injury. These patients can experience a range of symptoms, therefore rapid diagnosis and intervention is crucial. This case highlights challenges associated with colonic degloving injuries in combination with multiple associated injuries. We believe our success with this patient was due to prompt evaluation and intervention for his abdominal trauma as well as a multi-disciplinary approach involving consulting services for his burns, fractures, and other injuries.
Acknowledgments
None to declare.
Financial Disclosure
The authors have no financial or funding disclosures.
Conflict of Interest
The authors declare there is no conflict of interest.
Informed Consent
Informed consent was obtained from the patient. The patient was also appropriately de-identified for this manuscript.
Author Contributions
AM performed the initial manuscript write-up, literature review, and editing of the manuscript. LM, HG, and DC assisted with the manuscript write-up, literature review, and editing of the manuscript. GL assisted patient surgery and management of the patient. WS attended on the case and contributed to decision-making, management of the patient, literature review as well as editing of the manuscript.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
Abbreviations
CT: computed tomography; GCS: Glasgow Coma Scale; MVC: motor vehicle collision; SICU: surgical intensive care unit
| References | ▴Top |
- Hughes TM, Elton C. The pathophysiology and management of bowel and mesenteric injuries due to blunt trauma. Injury. 2002;33(4):295-302.
doi pubmed - Kordzadeh A, Melchionda V, Rhodes KM, Fletcher EO, Panayiotopolous YP. Blunt abdominal trauma and mesenteric avulsion: a systematic review. Eur J Trauma Emerg Surg. 2016;42(3):311-315.
doi pubmed - Terazumi K, Yanagawa Y, Takasu A, Sakamoto T. A case of degloving injury of the colon. Am J Emerg Med. 2012;30(1):250.e255-e256.
doi pubmed - Armstrong T, Blaquiere RM, Varshney S, Primrose JN. Traumatic ‘degloving’ of the colon in blunt abdominal injury. Colorectal Dis. 2002;4(2):141-143.
doi pubmed - Bege T, Brunet C, Berdah SV. Hollow viscus injury due to blunt trauma: a review. J Visc Surg. 2016;153(4 Suppl):61-68.
doi pubmed - Panesar D, Waddell O, Herd A. Traumatic ‘degloving’ injury to the ascending colon. ANZ J Surg. 2021;91(9):E627-E628.
doi pubmed - Fakhry SM, Watts DD, Luchette FA, EAST Multi-Institutional Hollow Viscus Injury Research Group. Current diagnostic approaches lack sensitivity in the diagnosis of perforated blunt small bowel injury: analysis from 275,557 trauma admissions from the EAST multi-institutional HVI trial. J Trauma. 2003;54(2):295-306.
doi pubmed - Gunn M, Campbell M, Hoffer EK. Traumatic abdominal aortic injury treated by endovascular stent placement. Emerg Radiol. 2007;13(6):329-331.
doi pubmed - Keller MA, Blewett CJ. Traumatic sigmoid degloving injuries in the pediatric population. Am Surg. 2011;77(4):509-510.
pubmed - Ho YH, Pritchett CJ. Blunt abdominal trauma causing a ‘degloving injury’ to the colon. Injury. 1990;21(2):119-120.
doi pubmed - Sternbergh WC, 3rd, Conners MS, 3rd, Ojeda MA, Money SR. Acute bilateral iliac artery occlusion secondary to blunt trauma: successful endovascular treatment. J Vasc Surg. 2003;38(3):589-592.
doi pubmed - McStay C, Ringwelski A, Levy P, Legome E. Hollow viscus injury. J Emerg Med. 2009;37(3):293-299.
doi pubmed - Ojuka KD, Nangole F, Ngugi M. Management of anterior abdominal wall defect using a pedicled tensor fascia lata flap: a case report. Case Rep Med. 2012;2012:487126.
doi pubmed pmc - Uri IF, Benamore R. Degloving bowel injury following blunt abdominal trauma: a rare CT finding. Emerg Med J. 2012;29(9):719.
doi pubmed - Vailas MG, Moris D, Orfanos S, Vergadis C, Papalampros A. Seatbelt sign in a case of blunt abdominal trauma; what lies beneath it? BMC Surg. 2015;15:121.
doi pubmed pmc - El Kafsi J, Kraus R, Guy R. A report of three cases and review of the literature on rectal disruption following abdominal seatbelt trauma. Ann R Coll Surg Engl. 2016;98(2):86-90.
doi pubmed pmc - Marano L, Carbone L, Poto GE, Calomino N, Neri A, Piagnerelli R, Fontani A, et al. Antimicrobial prophylaxis reduces the rate of surgical site infection in upper gastrointestinal surgery: a systematic review. Antibiotics (Basel). 2022;11(2):230.
doi pubmed pmc - Gustafsson UO, Scott MJ, Hubner M, Nygren J, Demartines N, Francis N, Rockall TA, et al. Guidelines for perioperative care in elective colorectal surgery: Enhanced Recovery After Surgery (ERAS®) Society Recommendations: 2018. World J Surg. 2019;43(3):659-695.
doi pubmed - Stefanou CK, Stefanou SK, Tepelenis K, Flindris S, Tsiantis T, Spyrou S. A big mesenteric rupture after blunt abdominal trauma: a case report and literature review. Int J Surg Case Rep. 2019;61:56-59.
doi pubmed pmc
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


