| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 15, Number 2-3, April 2024, pages 55-59
Lifestyle Interventions in a Patient Identified as Super-Super Obese With a Body Mass Index of 90.5
Ghadeer Al Ghareeba, d , Duoaa Abdoha, Mostafa Kofib, Ayman Afify Konswac
aPreventive Medicine, Lifestyle Medicine Program, Prince Sultan Military Medical City, Riyadh, Saudi Arabia
bPreventive Medicine, FCM Department, Prince Sultan Military Medical City, Riyadh, Saudi Arabia
cFamily Medicine, FCM Department, Prince Sultan Military Medical City, Riyadh, Saudi Arabia
dCorresponding Author: Ghadeer Al Ghareeb, Preventive Medicine, Lifestyle Medicine Program, Prince Sultan Military Medical City, Riyadh, Saudi Arabia
Manuscript submitted February 16, 2024, accepted April 4, 2024, published online April 8, 2024
Short title: Lifestyle Interventions in Super-Super Obese
doi: https://doi.org/10.14740/jmc4194
| Abstract | ▴Top |
Obesity is a growing global health concern. Saudi Arabia is experiencing a higher prevalence of obesity compared to the globe. This case report focuses on a 38-year-old female with a body mass index (BMI) of 90.5 kg/m2, prediabetes, and obstructive sleep apnea who successfully underwent a lifestyle modification process resulting in remarkable weight loss. The patient’s past unsuccessful attempts at weight loss had left her with a reluctance to try again initially. A multidisciplinary team collaborated to develop a management plan starting with an intensive lifestyle intervention. Lifestyle was assessed, then a structured personalized lifestyle intervention based on a plant-based diet and a gradual increase in physical activity was implemented. Over 6 months, the patient succeeded in losing 23 kg, a percent weight loss of 11.9%. An additional 5 kg was lost when liraglutide “Saxenda” was added. This case report represents the effectiveness of intensive lifestyle interventions in patients with super-super obesity for weight loss and long-term health improvement. Additional research is required to determine if the positive outcomes seen in treating a single patient can be applied to a larger population with super-super obesity. This brings up the question of whether pharmacotherapy or surgical interventions should be the primary approaches for addressing these cases, considering that surgical interventions usually involve lifestyle changes. What we already know about such cases: patients with super-super obesity often require interventions such as surgery or medication to aid in weight reduction, as they typically do not respond to lifestyle interventions alone. What this case report adds to existing knowledge: the use of lifestyle interventions proved effective in such cases as super-super obesity and delayed the need for surgical intervention even without weight reduction medications.
Keywords: Obesity; Weight loss; Lifestyle; Primary health care; Body mass index; Liraglutide
| Introduction | ▴Top |
Obesity is an excess body fat associated with health risks [1]. The estimated global prevalence of obesity is increasing among adults reaching up to 18.5% [2]. Saudi Arabia has a high prevalence in which about a quarter of adults are estimated to be obese with a 2.1% annual increase rate [2, 3]. Moreover, a high body mass index (BMI) is the leading risk factor for most disability and deaths combined in Saudi Arabia [4]. Obesity is classified into three classes depending on measured BMI and the excess health risk: class one (BMI: 30 - 34.9 kg/m2), class two (BMI: 35 - 39.9 kg/m2), and class three or morbid obesity (BMI > 40 kg/m2) [5]. Morbid obesity is classified into super obesity as a BMI ≥ 50 kg/m2, and super-super obesity as a BMI ≥ 60 kg/m2 [6].
Obesity is a devastating disease that can affect personal physical, mental, and social health and is associated with poor quality of life [7]. People with obesity may be comorbid with diabetes, hypertension, fatty liver disease, osteoarthritis, obstructive sleep apnea, and or so many types of cancer. They may also have depression, anxiety, binge eating disorders, and experience social stigma [7]. Individual, socioeconomic, cultural, and environmental factors are related to obesity [8]. A healthy lifestyle containing a plant-based diet, physical activity, managing stress, restorative sleep, social connectedness, and avoiding risky substances are modifiable risk factors that may prevent and treat obesity [9]. Treatment of obesity can be augmented with pharmacological or surgical intervention [10].
Because of the scarcity of high-risk patients with super-super obesity particularly those with BMI > 90 kg/m2, the evidence related to best management options is not well-defined. Benefit and harm balance particularly for surgical options was not determined, as many researchers excluded those patients, limiting the generalizability of the results for such patients [11].
This is a report of a super obese patient who underwent a lifestyle modification process for weight loss.
| Case Report | ▴Top |
Investigations
A 38-year-old single female presented to the obesity clinic at primary care for weight management. She was not complaining of any other medical illness other than obesity. The patient’s sister and aunt brought her to the clinic because she was partially willing to lose weight. She had not gone through a structured weight-loss trial previously. She attempted to lose weight through dietary instructions sourced from different social media platforms. However, the outcomes were only modest efficacy and overall dissatisfactory. She had a first-degree family history of obesity, but no one else in her family had super-super obesity. She resides with her aging parents and a housekeeper.
Diagnosis
Her vital signs were as follows: height 146 cm, weight 193 kg, BMI 90.5 kg/m2 with central obesity. Her blood pressure was normal with a regular pulse. Except for a prediabetes level of blood sugar, all of her laboratory results came back normal.
She had an elevated risk of obstructive sleep apnea using the STOP-BANG score.
All six pillars of lifestyle medicine were assessed. She had no physical activity or muscle-strengthening exercise engagement during the week and spent most of her daytime sitting or reclining at home. There was objective evidence of major mobility limitations on a 400-m walk test and climbing one flight of stairs.
In terms of nutrition, the patient’s daily diet consisted mainly of sugary foods and drinks, as well as ultra-processed foods, with very little intake of fruits and vegetables.
Throughout the day, her sleep pattern was frequently interrupted, resulting in only unrefreshed 4 - 5 h of sleep. She did not engage in smoking or substance abuse, and she had limited social connections. Overall, her mental health was generally stable.
Treatment
A multidisciplinary team was formed to discuss the case including a preventive medicine physician, a family medicine physician, a diabetologist, an endocrinologist, a bariatric surgeon, and a health coach. Both preventive and family medicine physicians had lifestyle medicine training along with the health coach. We suggested starting a structured lifestyle intervention for 6 months, then adding weight loss medications “liraglutide” (Saxenda), and then going for surgery. In addition, metformin was prescribed for prediabetes and continuous positive airway pressure (CPAP) for obstructive sleep apnea.
The lifestyle intervention focused on achieving a negative energy balance by implementing a plant-based diet with reduced calorie consumption and gradually increasing physical activity to enhance energy expenditure. The patient adheres to Harvard’s healthy eating plate (Fig. 1), which provides a convenient way to consume energy-poor but nutrient-dense food that helps regulate appetite without the need for calorie counting [12]. This visual guide recommends filling half of the 9-inch plate with non-starchy vegetables and fruits, one-quarter with whole grains, and one-quarter with lean proteins.
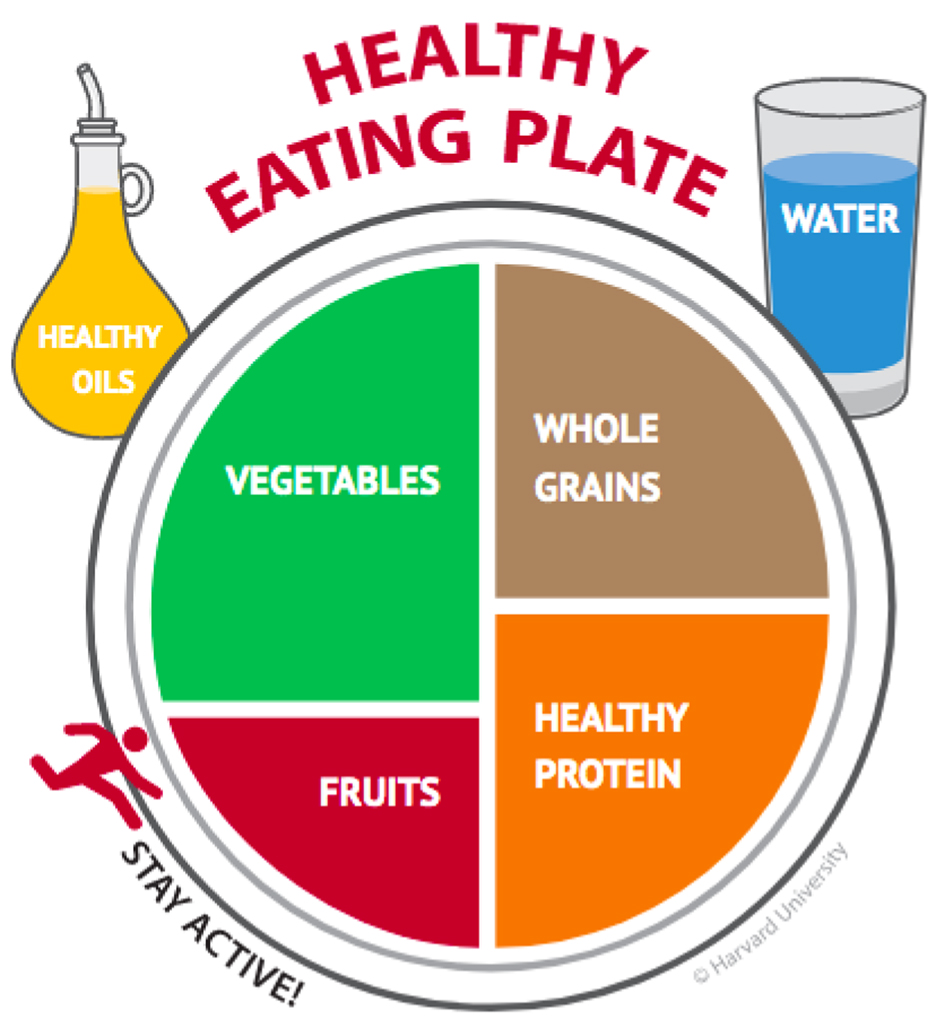 Click for large image | Figure 1. Healthy eating plate. |
The team encouraged and supported her to avoid overeating by consuming three balanced meals daily and stop eating snacks. We also discouraged her from eating sugar-sweetened beverages, high-fat foods, and highly processed foods. In addition, drinking 2 - 3 L of water and herbal teas was emphasized. This approach to eating allows for flexibility in food choices based on the patient’s preferences and availability, and keeps meals enjoyable. At the same time, it promotes the patient’s long-term adaptation to a sustainable and healthy eating style.
Regarding physical activity, we agreed with the patient on an achievable exercise plan based on the patient’s fitness level and preference intended to build a persistent habit. To improve the patient’s cardio-respiratory fitness, walking 2 min three times daily at home was added to her daily schedule. Months later, the patient gradually progressed to daily moderate-intensity walking for a non-continuous 15 min at home but sometimes outdoors. Resistance training for the upper limb using appropriate weightlifting was also added to the patient’s fitness plan with 10 repetitions three times daily. Later, it progressed to include longer sessions, about 5 to 10 min, 2 days per week. Resistance training builds and maintains muscle strength and endurance for the patient and aids both her weight loss and maintenance. Furthermore, the patient was encouraged to interrupt her setting with any physical activity, such as housecleaning, dishwashing, cooking, or simply moving. This is to enjoy social connection with her family, fill time away from eating, and overcome feelings of fatigue.
Despite making efforts to adjust bedtime and wake-up times to improve nighttime rest, the patient found it difficult to extend their sleep duration. To address this issue, the patient implemented an incremental approach by gradually advancing their sleep schedule by 30 min each week. She also intentionally set her wake-up time 30 min earlier. This incremental adjustment, combined with the consistent use of CPAP therapy, allowed the patient to experience uninterrupted sleep and increase her nighttime sleep duration to 6 h.
The patient’s weight loss journey was greatly influenced by the support of her family, particularly her sister. During the first 6 months, the patient spent 5 days a week at her sister’s home, where they both shared the goal of losing excess weight. The supportive environment created by her sister played a significant role in the patient’s success. Her sister actively participated in her care by ensuring that the patient followed the dietary recommendations. They worked together to purchase healthy food options, prepare nutritious meals, and emphasize portion control and a balanced diet. This collaborative approach to meal planning and preparation fostered a sense of shared responsibility and commitment to healthier eating habits. Additionally, the sister actively engaged in exercise practices by walking alongside the patient and participating in resistance training. This collaborative exercise routine not only improved adherence to physical activity regimens but also contributed to the patient’s overall well-being.
Follow-up and outcomes
The patient was committed to attending hybrid follow-up visits every 2 weeks for the first 6 months and then monthly for the next 6 months. We measured her weights in the clinic monthly during the in-person visit. During the course of lifestyle changes of 6 months duration, the patient successfully lost 23 kg, which accounted for a percent weight loss of 11.9%. Subsequently, the patient came unaccompanied to the clinic, willing to continue weight management, and trusted her ability to lose weight. At this point, the medication liraglutide “Saxenda” was introduced, and over the course of 3 months, she lost an additional 5 kg.
Therefore, after 1 year of follow-up, the patient had achieved a total weight loss of 28 kg, which represented a percent weight loss of 14%. Her BMI had decreased to 77.4 kg/m2. As a result, she regained her ability to perform daily activities and took care of herself and others.
Figure 2 shows a graphical representation of the patient’s weight loss progress throughout the year of follow-up.
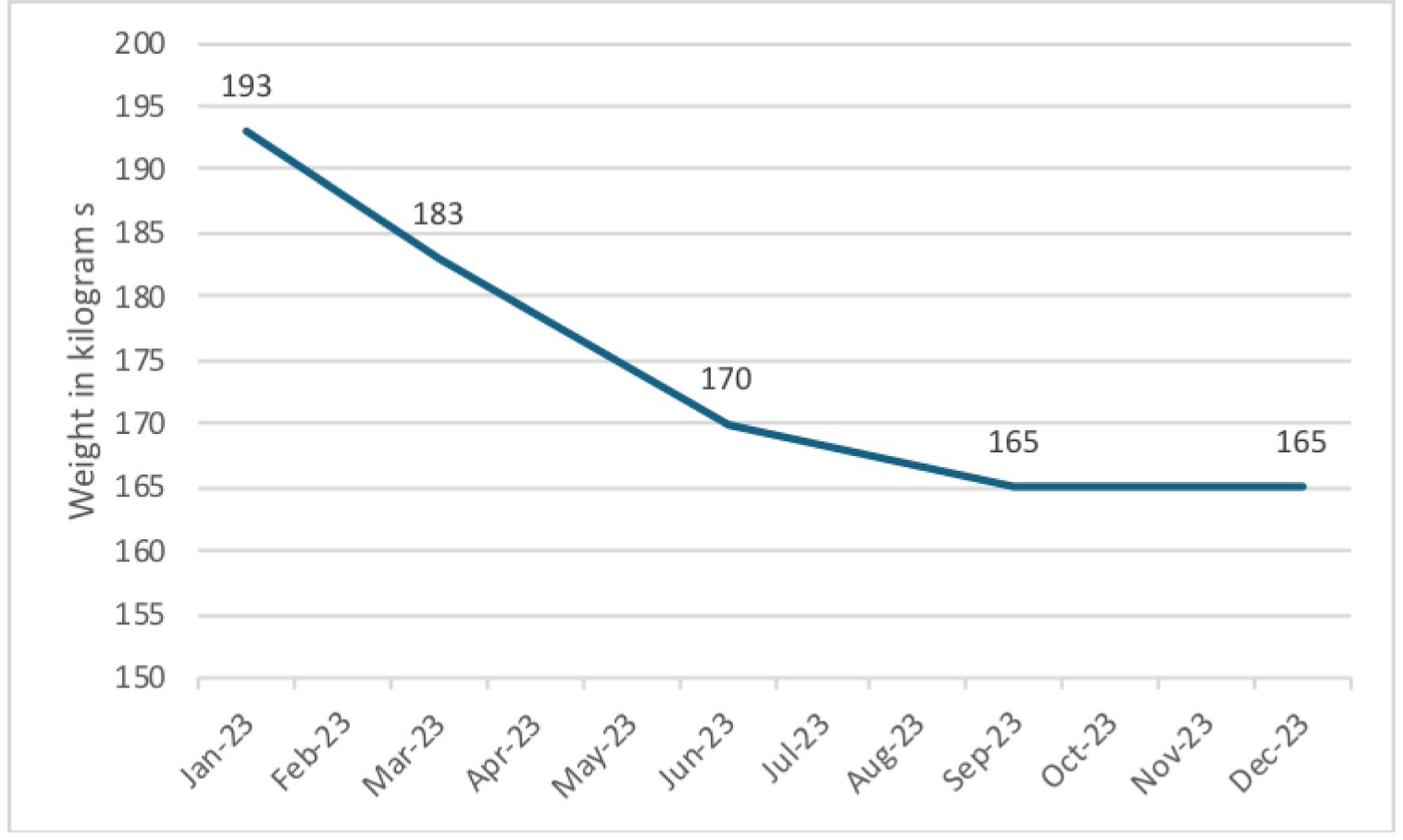 Click for large image | Figure 2. Patient’s weight loss throughout the follow-up year, 2023. |
| Discussion | ▴Top |
Obesity, particularly at its extreme levels such as morbid, super, and super-super obesity, presents significant challenges in management and treatment. Current literature predominantly emphasizes pharmacological and surgical interventions as the principal modalities for weight loss in these severe cases [13]. Surgical treatments like laparoscopic sleeve gastrectomy (LSG) are proven to be effective in greatly reducing weight and handling health problems in people with very high BMI [14, 15]. These treatments are essential in cases where the extreme level of obesity cannot be managed by lifestyle changes alone, showing the need for a complete care approach for patients with super-super obesity [13]. Despite their efficacy, these interventions are associated with significant risks and potential complications.
In contrast, lifestyle interventions, while essential in obesity management, have been, to some extent, overlooked in the context of extreme obesity due to their perceived limited effectiveness. However, this case report highlights the critical role of lifestyle interventions as the primary strategy in comprehensive obesity management, especially in its most severe forms, such as super-super obesity (BMI ≥ 60 kg/m2). Despite the common focus on drug and surgical options, which are associated with significant risks and complications [13], the impressive results from our case study demonstrate the success of well-planned lifestyle interventions. These interventions have resulted in significant weight loss, even in individuals with a BMI of 90.5 kg/m2, proving the effectiveness of lifestyle interventions as a crucial method for obesity treatment. The vital support from family members and the teamwork of various healthcare professionals underscores the necessity of a comprehensive approach to treatment. Additionally, the gradual integration of medications fostering the patient’s self-efficacy and independence in managing their health are crucial aspects of this case. These findings indicate that lifestyle interventions trigger weight loss and empower patients on their long-term health journey.
The implementation of a comprehensive and personalized nature of lifestyle intervention to the unique circumstances of this case is our main strength. We carefully considered her needs and collaborated with various healthcare professionals to ensure a multidisciplinary approach. Implementation of lifestyle interventions with a focus on fostering self-efficacy and independence was also a key strength of our approach. However, this case report is based on the experience of a single patient, which may limit the generalizability of our findings to the broader population. Furthermore, our approach does lack a control group, which makes it challenging to isolate and assess the specific impact of lifestyle interventions.
Learning points
This case report challenges the paradigm that lifestyle interventions are less effective for individuals with super-super obesity. It demonstrates that a comprehensive, personalized, and multidisciplinary approach can lead to a significant weight loss and health improvement before escalating to riskier pharmacological or surgical interventions. This report highlights the need for further research to explore the full potential and long-term effectiveness of lifestyle interventions in patients with super-super obesity.
In summary, a structured and personalized lifestyle intervention, based on evidence-based principles of lifestyle medicine, successfully facilitated weight loss in a patient with super-super obesity. It is worth noting that family support played a crucial role in promoting adherence to the intervention.
Acknowledgments
We are pleased to thank the patient and his family for agreeing to publish this case. We thank the Research Ethics Committee for their help obtaining approval to publish the case.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
We obtained patient consent. The patient consented for clinical information to be reported in the journal without any identification information.
Author Contributions
GG wrote the introduction, case presentation, and revised the last version. DA composed the draft, wrote the discussion of the manuscript, and revised the last version. MK helped to organize medical documentation, write the manuscript, and review it. AAK coordinated the patient’s management, initiated the process of writing the manuscript, and finally, reviewed the manuscript. All authors read and approved the final manuscript.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
| References | ▴Top |
- WHO. Obesity and overweight [Internet]. June 9, 2021. Available from: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (Assessed January 23, 2024).
- World Obesity Federation. Obesity Atlas 2023. World Obes Atlas. 2022;(March):1-289.
- Althumiri NA, Basyouni MH, AlMousa N, AlJuwaysim MF, Almubark RA, BinDhim NF, Alkhamaali Z, et al. Obesity in Saudi Arabia in 2020: prevalence, distribution, and its current association with various health conditions. Healthcare (Basel). 2021;9(3):311.
doi pubmed pmc - Global Burden of Disease Compair, Saudi Arabia [Internet]. Institute of Health Metricsa and Evaluation. 2019. Available from: https://vizhub.healthdata.org/gbd-compare/# (Assessed January 28, 2024).
- CDC. Defining Adult Overweight & Obesity [Internet]. Center for Disease Control and Prevention. Available from: https://www.cdc.gov/obesity/basics/adult-defining.html (Assessed January 29, 2024).
- Eisenberg D, Shikora SA, Aarts E, Aminian A, Angrisani L, Cohen RV, de Luca M, et al. 2022 American Society of Metabolic and Bariatric Surgery (ASMBS) and International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO) Indications for Metabolic and Bariatric Surgery. Obes Surg. 2023;33(1):3-14.
doi pubmed pmc - Bluher M. Obesity: global epidemiology and pathogenesis. Nat Rev Endocrinol. 2019;15(5):288-298.
doi pubmed - Masood B, Moorthy M. Causes of obesity: a review. Clin Med (Lond). 2023;23(4):284-291.
doi pubmed pmc - Parkinson MD, Stout R, Dysinger W. Lifestyle medicine: prevention, treatment, and reversal of disease. Med Clin North Am. 2023;107(6):1109-1120.
doi pubmed - Ryan DH, Kahan S. Guideline recommendations for obesity management. Med Clin North Am. 2018;102(1):49-63.
doi pubmed - Peterson K, Anderson J, Boundy E, Ferguson L, Erickson K. Rapid evidence review of bariatric surgery in super obesity (BMI ≥ 50 kg/m2). J Gen Intern Med. 2017;32(Suppl 1):56-64.
doi pubmed pmc - Healthy Eating Plate [Internet]. The Nutrition Source, Department of Nutrition, Harvard T.H. Chan School of Public Health. Available from: https://www.hsph.harvard.edu/nutritionsource/healthy-eating-plate/ (Assessed April 3, 2024).
- Crossan K, Sheer AJ. Surgical options in the treatment of severe obesity. Treasure Island (FL): StatPearls Publishing; 2024. Available from: https://www.ncbi.nlm.nih.gov/books/NBK576372/.
pubmed - Singla V, Gupta A, Gupta A, Monga S, Kumar A, Chekuri R, Gupta M, et al. Outcomes of laparoscopic sleeve gastrectomy (LSG) vs one-anastomosis gastric bypass (OAGB) in patients with super-super obesity (BMI ≥ 60 kg/m2). Obes Surg. 2024;34(1):43-50.
doi pubmed - Salminen P, Gronroos S, Helmio M, Hurme S, Juuti A, Juusela R, Peromaa-Haavisto P, et al. Effect of laparoscopic sleeve gastrectomy vs Roux-en-Y gastric bypass on weight loss, comorbidities, and reflux at 10 years in adult patients with obesity: The SLEEVEPASS randomized clinical trial. JAMA Surg. 2022;157(8):656-666.
doi pubmed pmc
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


