| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 14, Number 11, November 2023, pages 387-392
Cervical Radiculopathy Presenting as Ischemic Stroke After Carotid Artery Stent Placement
Itzhak Brooka, c, Bilaal Sirdarb, Andrew Stemerb
aDepartment of Pediatrics, Georgetown University School of Medicine, and the Neurology Center, Washington DC, USA
bDepartment of Neurology, Georgetown University School of Medicine, and the Neurology Center, Washington DC, USA
cCorresponding Author: Itzhak Brook, Department of Pediatrics, Georgetown University School of Medicine, and the Neurology Center, 4431 Albemarle St NW, Washington, DC 20016, USA
Manuscript submitted October 2, 2023, accepted November 10, 2023, published online November 23, 2023
Short title: Cervical Radiculopathy Presenting as Stroke
doi: https://doi.org/10.14740/jmc4162
| Abstract | ▴Top |
Abrupt loss of focal brain function is the main characteristic of the beginning of ischemic stroke. However, individuals with disorders other than stroke can also present with similar features. These conditions include seizure disorders, migraine, central nervous system abscess or tumor, head trauma, subdural hematoma, cerebral venous thrombosis, viral encephalitis, conversion reaction, hypertensive encephalopathy, multiple sclerosis, and spinal cord disorder. An 82-year-old man presented with a sudden onset of numbness in his left forearm in the distribution of C6 and C7 spinal nerves, 2 days after undergoing endarterectomy and stent placement in his right carotid artery because of stenosis. He was diagnosed with hypo-pharyngeal squamous cell carcinoma (T1, L0, M0) 17 years earlier (2006) which was treated with 70 Gy intensity-modulated radiotherapy (IMRT). The patient underwent stent insertion into his left carotid artery 3.5 years earlier because of 80% carotid artery stenosis. He was initially suspected to have an ischemic stroke. However, computed tomography angiography of the head and neck did not show stenosis or occlusion of the major intracranial arteries and no aneurysms were identified. It showed interval stenting of the cervical portion of the right carotid artery and stable appearance of left carotid artery stent. Both carotid artery stents and the vertebral arteries were patent. The cervical spine showed bilateral moderate to severe foramen stenosis in C3-C4 and C5-C6, and moderate to severe stenosis in the right C2-C3 and left C4-C5. His symptoms subsided after performing neck extension exercises. This is the first report of a patient whose cervical radiculopathy symptoms were suspected to be caused by ischemic stroke. The recent angioplasty and stent placement in the right carotid artery made the association more likely and had to be excluded. Clinicians should be aware that cervical radiculopathy could present as ischemic stroke. It is therefore important that disorders that cause symptoms similar to ischemic stroke are also considered in these individuals.
Keywords: Cervical radiculopathy; Carotid artery; Stent; Ischemic stroke; Stenosis
| Introduction | ▴Top |
Abrupt loss of focal brain function is the main characteristic of ischemic stroke [1]. However, individuals with disorders other than stroke can also present with similar symptoms. These conditions include seizure disorders, migraine, central nervous system abscess or tumor, head trauma, subdural hematoma, cerebral venous thrombosis, viral encephalitis, conversion reaction, hypertensive encephalopathy, multiple sclerosis, and spinal cord disorder (e.g., vertebral radiculopathy, compressive myelopathy, spinal dural arteriovenous fistula) [2-4].
This case report describes a patient who presented with sudden onset of sensory deficit in his left arm 2 days after undergoing endarterectomy and stent placement in his right carotid artery. He was initially suspected to suffer from an ischemic stroke, but eventually his symptoms were determined to be caused by cervical radiculopathy.
| Case Report | ▴Top |
Investigations
An 82-year-old man presented to the emergency department with sudden onset of numbness of the lateral half of his left arm. The patient underwent proximal right carotid artery angioplasty and stent placement in his right carotid artery because of 74.2% carotid artery stenosis 2 days earlier. Residual stenosis after the procedure was under 45% via North American Symptomatic Carotid Endarterectomy Trial (NASCET) criteria. Dyna brain computed tomography (CT) scan following the procedure confirmed absence of infarct or hemorrhage.
The patient was diagnosed with hypo-pharyngeal squamous cell carcinoma (T1, L0, M0) 17 years earlier (2006) which was treated with 70 Gy intensity-modulated radiotherapy (IMRT). The cancer recurred (T2, L0, M0) 2 years later (2008) requiring bilateral radical neck dissection and total laryngectomy. Restoration of his larynx was performed using a left forearm free flap. He had no signs of tumor recurrence since then. He was speaking using an esophageal-tracheal voice prosthesis.
The patient underwent angioplasty and stent insertion into his left carotid artery 3.5 years earlier because of 80% carotid artery stenosis.
The patient suffered from mild to severe osteoarthritis of his knees and shoulders, fibrosis of his neck, peripheral neuropathy in his legs, xerostomia, dysphagia, hypothyroidism, diverticulosis, mild psoriasis, and migraines. He did not smoke or consume alcohol. He developed paroxysmal hypertension 4 years after receiving the radiation therapy (2000), which was ameliorated following the placement of a stent into the left carotid artery [5].
The patient underwent periodical Doppler ultrasound examination every 6 months and a severe right carotid artery stenosis was noted 3 weeks earlier. He experienced increased dizziness, fatigue and “brain fog” in the past 4 months.
Diagnosis
On presentation, his temperature was 36.7 °C, his blood pressure was 166/86 mm Hg, pulse was 87/minute, oxygen saturation was 97%, and respiration was 18 breaths/minute. Blood gases showed pCO2 venous 36.3 mm Hg, pO2 venous 32.1 mm Hg, HCO3 26.0 mmol/L, TCO2 venous 26 mmol/L, base excess/deficit venous 2.2 mmol/L, and O2 saturation venous calculated 66.1%.
Physical examination showed the patient to be alert and oriented and in mild distress; no respiratory distress; lungs were clear to auscultation with good air exchange, no crackles, and no wheeze; heart and cardiovascular showed normal heart rate, regular rhythm, normal S1, and S2; there was no peripheral edema or venous distension; distal pulses were strong and equal in all limbs; and there was moderate right carotid artery bruit.
He had numbness of his left forearm in the distribution of C6 and C7 and C6 and C7 cervical nerves. Neurological examination did not show any muscle weakness, and all deep tendon reflexes were adequate. Vision acuity and eye movement were adequate. Pupils were equal and reactive to light. The rest of the neurological examination was intact.
Laboratory results showed Hgb 14.1 g/dL, Hct 39.9%, red blood cell count (RBC) 4.31 cells/µL, white blood cell count (WBC) 5.62 × 103/µL, lymphocytes 35.8%, monocytes 2%, eosinophils 1.4%, basophiles 0.2%, absolute neutrophils 3.4 × 103/µL, absolute lymphocytes 2.0 × 103/µL, absolute monocytes 100/µL, absolute basophiles 0/µL, platelets 1.87 × 105k/µL, mean platelet volume (MPV) 10 fL, mean corpuscular hemoglobin (MCH) 32.7 pg, mean corpuscular hemoglobin concentration (MCHC) 35.3 g/dL, red cell distribution width (RDW) 13%, prothrombin time (PT) 13.1 s, and international normalized ratio (INR) 1.0.
Sodium was 138 mEq/L, potassium was 4.2 mEq/L, chloride was 106 mEq/L, CO2 was 22 mmol/L, blood urea nitrogen (BUN) was 14 mg/dL, creatinine was 0.94 mg/dL, estimated CrCl was 58.83 mL/min, glucose was 105 mg/dL, calcium was 9.5 mg/dL, lactic acid was 1.07 mmol/L, and high-sensitivity troponin-I was 7 ng/L. liver panel test and urinalysis were within normal limits.
The patient was receiving aspirin 320 mg/day, clopidogrel 75 mg/day, synthroid 100 µg/day, atenolol 6.25/day, and doxazosin 0.5 mg/day.
CT angiography of the head and neck did not show stenosis or occlusion of the major intracranial arteries and no aneurysms were identified. It showed interval stenting of the cervical portion of the right carotid artery and stable appearance of left carotid artery stent. Both carotid artery stents and the vertebral arteries were patent (Fig. 1).
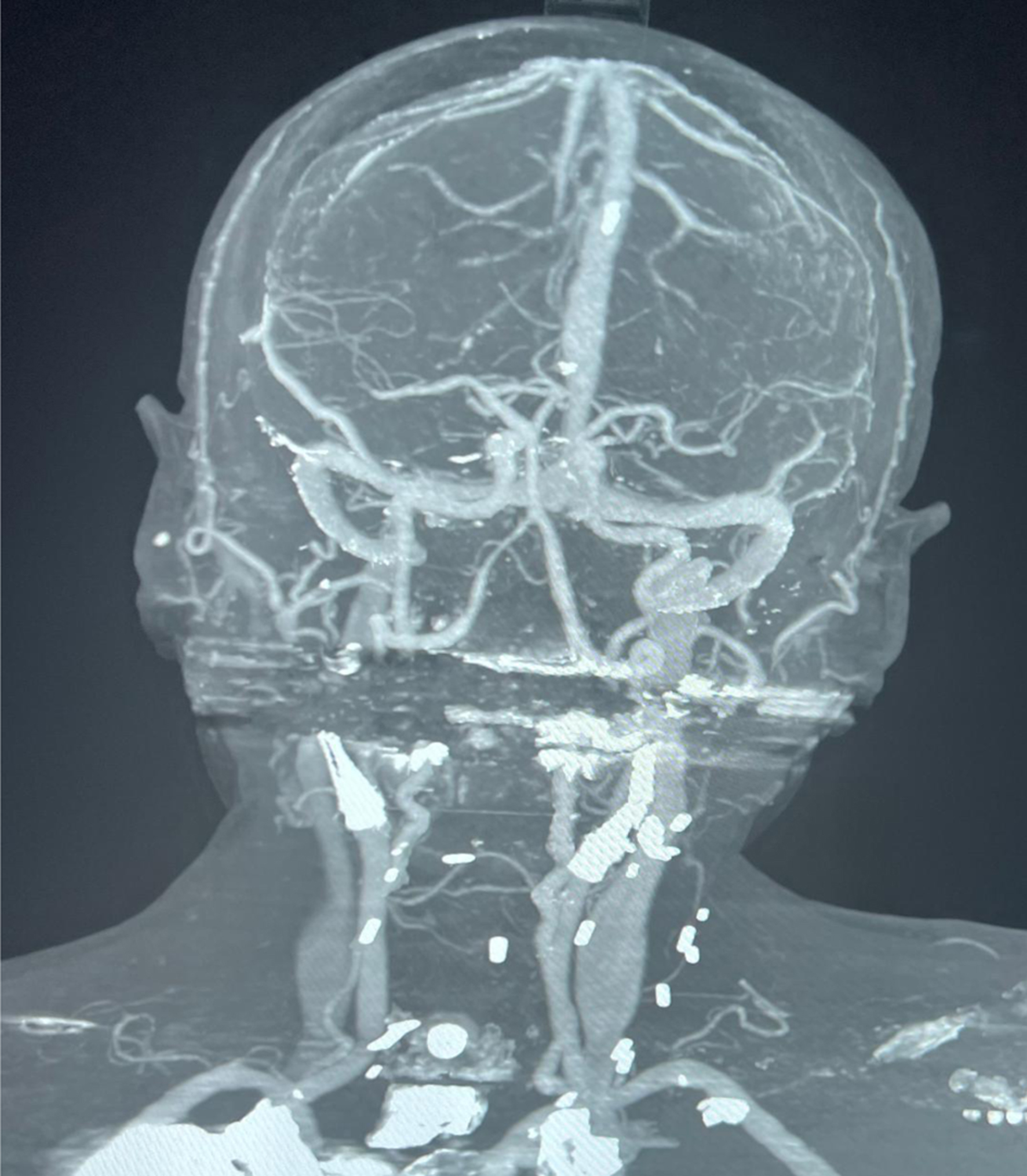 Click for large image | Figure 1. CT with contrast of the head. CT: computed tomography. |
The cervical spine showed bilateral moderate to severe foramen stenosis in C3-C4 and C5-C6, and moderate to severe stenosis in the right C2-C3 and left C4-C5 (Figs. 2 and 3).
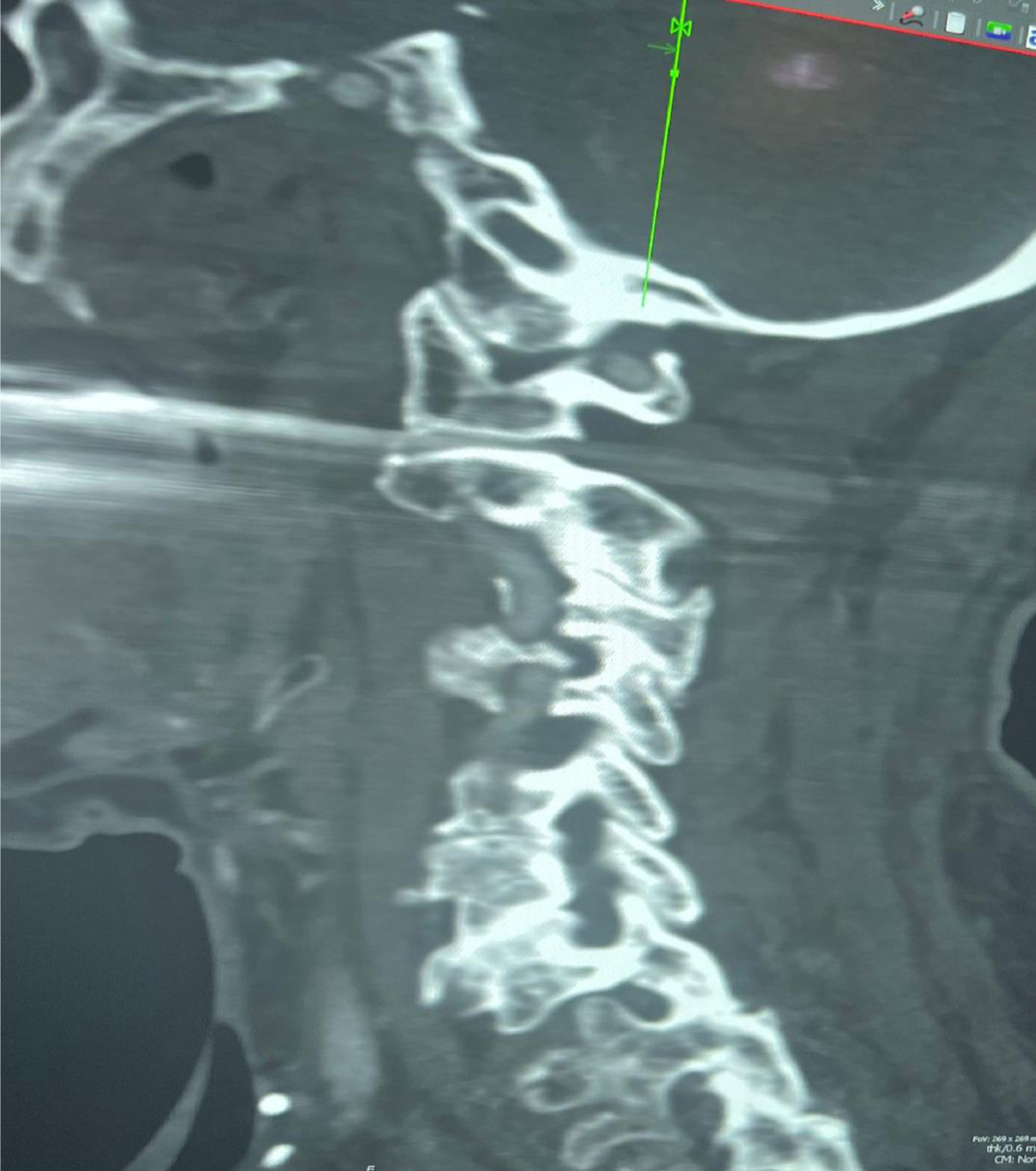 Click for large image | Figure 2. CT of the cervical spine: view of the left foramina showing moderate to severe foramen stenosis in C3-C4 and C5-C6 and severe stenosis in C4-C5. CT: computed tomography. |
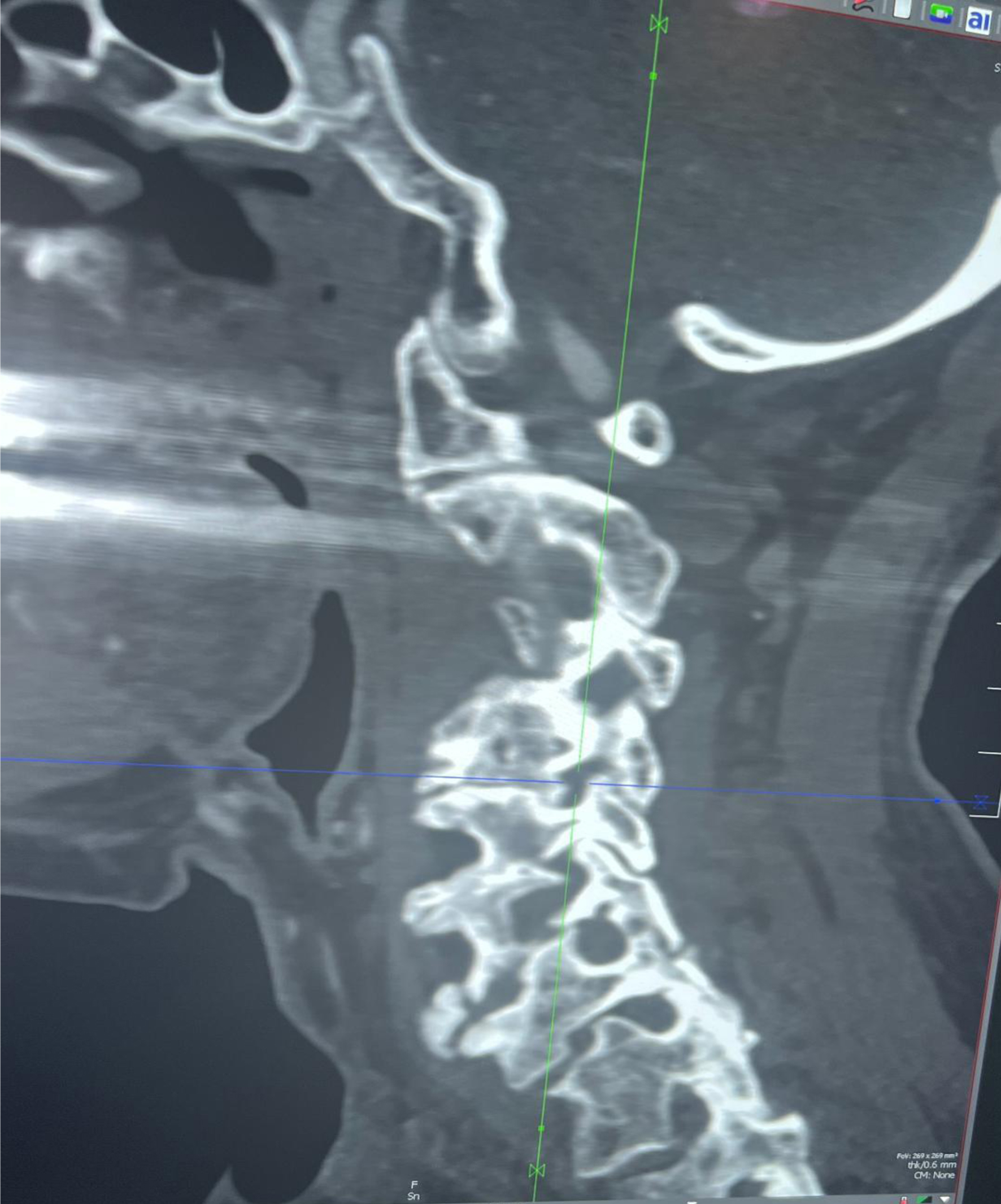 Click for large image | Figure 3. CT of the cervical spine: view of the right foramina showing moderate to severe foramen stenosis in C3-C4 and C5-C6 and severe stenosis in C2-C3. CT: computed tomography. |
Treatment
The patient recalled that he was diagnosed with cervical radiculopathy 15 years earlier. He started to perform neck extension exercises of slowly tilting his neck to the right side, holding the position for 5 s, and returning the neck to the upright, neutral position. After performing these exercises for 10 min, some of the left hand numbness subsided. It was concluded that the numbness in the left arm was due to cervical radiculopathy.
Follow-up and outcomes
The patient was discharged from the emergency department and was referred to the neurology clinic. He continued to perform neck extension exercises and the left hand numbness disappeared within 24 h.
The patient’s cervical radiculopathy was treated conservatively by physical therapy with neck extension exercises.
| Discussion | ▴Top |
We report a patient who presented with a sudden onset of sensory deficit in his left arm 2 days after undergoing endarterectomy and stent placement in his right carotid artery. It was initially suspected that he suffered from an ischemic stroke, but eventually his symptoms were determined to be caused by cervical radiculopathy. The left hand numbness disappeared after performing cervical extension exercises.
The causes of radiculopathy can be either compressive or non-degenerative. Most radiculopathies originate from nerve root compression [6]. Causes of non-degenerative radiculopathy include infections (i.e., Lyme disease, herpes zoster), infiltration by tumor or granulomatous tissue, nerve root infarction or avulsion, demyelination, and inflammatory and neurodegenerative disorders [7].
Compressive cervical radiculopathy is a common cause of arm pain with or without sensory and motor dysfunction. It can affect any of the eight cervical nerve roots emerging from the spine. Its clinical signs are most often caused by nerve root compression due to cervical spondylosis or disc herniation [6, 8]. They include neck, shoulder, or arm pain or muscle weakness, sensory symptoms, or weakened deep tendon reflexes.
The management of most patients with compressive cervical radiculopathy with radicular pain with paresthesia or numbness, or non-progressive weakness without myopathy is mainly conservative. This includes administration of oral analgesics, a short course of oral prednisone if pain is severe, and physical therapy. The value of surgery for the treatment of cervical radiculopathy has not been clearly established.
Several techniques are available for those undergoing surgery for cervical radiculopathy without myelopathy [9]. A recent trial of 265 patients with cervical radiculopathy found that the efficacy and safety outcomes were similar for individuals assigned either to posterior foraminotomy or to anterior cervical discectomy with fusion [10].
The clinical diagnosis of cervical radiculopathy is primarily based on history and clinical examination. Further testing is usually not required for those who have minimal or no motor deficit and are not at high risk of having an underlying malignant, infectious, or inflammatory cause [8].
Our report is the first to describe a patient whose cervical radiculopathy symptoms were suspected to be caused by an ischemic stroke. The recent angioplasty and stent placement in the right carotid artery made the association more likely and had to be excluded by CT scan with contrast.
Madedor et al [4] described a patient who presented with stroke symptoms of sudden balance impairment, prompting the stroke assessment protocol. However, further neurologic workup and imaging led to the ruling out of the initial diagnosis of stroke and the patient was eventually diagnosed with cervical spondylotic myelopathy.
Acute ischemic stroke is a severe and life-threatening emergency, especially when it is brought about by a large-vessel blockage. The only available two management choices are intravenous alteplase and endovascular treatment (mechanical clot removal), both of which are extremely time-dependent. Therefore, speedy patient transfer, diagnosis, and treatment are critical, and time-consuming imaging methods and overly selective management selection standards should be avoided. This is why patients who present with abrupt appearance of symptoms compatible with ischemic stroke generally generate a stroke code [3, 11-13]. Stroke protocol requires that hospital personnel and stroke team initiate diagnosis and treatment of a potential stroke as soon as the patient arrives at the emergency department [11-13].
Conclusions
Clinicians should be aware that cervical radiculopathy as well as other non-degenerative conditions could mimic an ischemic stroke. Causes of non-degenerative radiculopathy include infections (i.e., Lyme disease, herpes zoster), infiltration by tumor or granulomatous tissue, nerve root infarction or avulsion, demyelination, and inflammatory and neurodegenerative disorders [2-4]. It is therefore essential that other disorders that cause symptoms similar to ischemic stroke are also considered in these individuals especially in those who had a history of any of these conditions.
Learning points
Cervical radiculopathy could present as ischemic stroke. Disorders that cause symptoms similar to ischemic stroke should also be considered in patients who present with them.
Acknowledgments
The authors acknowledge the Jain Neil Kalpeshand, DO, and Anousheh Saya, MD, for reviewing the radiological studies.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Informed consent has been obtained.
Author Contributions
All authors contributed to the writing/editing part of this paper. Itzhak Brook MD wrote the report, reviewed literature, and contributed to the diagnosis. Bilaal Sirdar MD and Andrew Stemer MD edited and guided us in writing this manuscript.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Ozaki S, Akimoto T, Iida Y, Miyake S, Suzuki R, Shimohigoshi W, Hori S, et al. Complications and outcomes of carotid artery stenting in high-risk cases. J Stroke Cerebrovasc Dis. 2023;32(10):107329.
doi pubmed - Yaowen Hu, Junhui Su, Xinxin Cui, Jin L, Teng F. How to avoid misdiagnosing spontaneous cervical spinal epidural hematoma as ischemic stroke: 3 case reports and literature review. Cerebrovasc Dis. 2022;14:1-10.
- Wang Y, Zha H. Neuroimaging for differential diagnosis of transient neurological attacks. Brain Behav. 2022;12(12):e2780.
doi pubmed pmc - Madedor OJ, Lee S, Levey R. Cervical spondylotic myelopathy presenting as ischemic stroke: a case report. Cureus. 2019;11(3):e4291.
doi pubmed pmc - Brook I, Cohen E, Stemer A. Correction of carotid artery stenosis by stent placement ameliorated paroxysmal hypertension after radiation treatment of hypopharyngeal carcinoma: a case report. J Med Case Rep. 2022;16(1):70.
doi pubmed pmc - Devine JG, Schenk-Kisser JM, Skelly AC. Risk factors for degenerative spondylolisthesis: a systematic review. Evid Based Spine Care J. 2012;3(2):25-34.
doi pubmed pmc - Woods BI, Hilibrand AS. Cervical radiculopathy: epidemiology, etiology, diagnosis, and treatment. J Spinal Disord Tech. 2015;28(5):E251-259.
doi pubmed - Polly DW, Jr., Haselhuhn JJ, Soriano PBO, Odland K, Jones KE. Management of high-grade dysplastic spondylolisthesis. Neurosurg Clin N Am. 2023;34(4):567-572.
doi pubmed - Broekema AEH, Groen RJM, Simoes de Souza NF, Smidt N, Reneman MF, Soer R, Kuijlen JMA. Surgical interventions for cervical radiculopathy without myelopathy: a systematic review and meta-analysis. J Bone Joint Surg Am. 2020;102(24):2182-2196.
doi pubmed - Broekema AEH, Simoes de Souza NF, Soer R, Koopmans J, van Santbrink H, Arts MP, Burhani B, et al. Noninferiority of posterior cervical foraminotomy vs anterior cervical discectomy with fusion for procedural success and reduction in arm pain among patients with cervical radiculopathy at 1 year: the FACET randomized clinical trial. JAMA Neurol. 2023;80(1):40-48.
doi pubmed pmc - Kassardjian CD, Willems JD, Skrabka K, Nisenbaum R, Barnaby J, Kostyrko P, Selchen D, et al. In-patient code stroke: a quality improvement strategy to overcome knowledge-to-action gaps in response time. Stroke. 2017;48(8):2176-2183.
doi pubmed - Sanjuan E, Pancorbo O, Santana K, Minarro O, Sala V, Muchada M, Boned S, et al. Management of acute stroke. Specific nursing care and treatments in the stroke unit. Neurologia (Engl Ed). 2023;38(6):419-426.
doi pubmed - Ospel JM, Holodinsky JK, Goyal M. Management of acute ischemic stroke due to large-vessel occlusion: JACC focus seminar. J Am Coll Cardiol. 2020;75(15):1832-1843.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


