| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 14, Number 7, July 2023, pages 244-250
Late Presentation of Tricho-Rhino-Phalangeal Syndrome (TRPS1 Affected) Associated Hip Pathology
Faye Gracea, c, Elizabeth Ashbyb
aPhysiotherapy Department, Cambridge University Hospital NHS Foundation Trust, Cambridge, CB2 OQQ, UK
bDepartment of Paediatric Orthopaedics, Cambridge University Hospital NHS Foundation Trust, Cambridge, CB2 OQQ, UK
cCorresponding Author: Faye Grace, Physiotherapy Department, Cambridge University Hospital NHS Foundation Trust, Cambridge, CB2 OQQ, UK
Manuscript submitted May 31, 2023published online July 31, 2023
Short title: TRPS1 Associated Hip Pathology
doi: https://doi.org/10.14740/jmc4125
| Abstract | ▴Top |
Perthes disease typically presents between the ages of 4 and 9 years and is characterized by unilateral or bilateral avascular necrosis of the femoral head. Clinically it presents with pain and decreased range of motion and has a disease course of up to 5 years. We report the clinical and radiological findings of a female in early adolescence who was referred to pediatric physiotherapy and found to have Perthes-like changes of the hip, on a background of tricho-rhino-phalangeal syndrome type 1 (TRPS1). The patient’s first symptoms of hip pain were reported at age 10, but there was no radiographic evidence until 2.5 years later when a diagnosis of Perthe’s disease was made. This uniquely late presentation may have been due to the altered skeletal maturation seen in TRPS1, whereby skeletal age lags behind chronological age. This case highlights the importance of identifying relevant past medical history on initial assessment, and having rapid access to radiology and orthopedic support to enable timely diagnosis, as prognosis becomes poorer as age increases. Perthes-like changes should be considered as a differential diagnosis in patients presenting with non-traumatic hip pain, regardless of age of onset.
Keywords: Perthes disease; TRPS1; Tricho-rhino-phalangeal syndrome; Hip pain; Physiotherapy; Pediatric orthopedics
| Introduction | ▴Top |
Tricho-rhino-phalangeal syndrome was first described in 1966 with characteristics including sparse, slow-growing fine hair and cone-shaped epiphyses with premature fusion [1]. Tricho-rhino-phalangeal syndrome type 1 (TRPS1) is inherited in an autosomal dominant manner [2]. Over time, TRPS1 has been characterized further with additional features including hip changes such as coxa magna, hip dysplasia and Legg-Calve-Perthes disease (Perthes disease). Perthes disease is characterized by unilateral or bilateral avascular necrosis of the femoral head. Clinically it presents with pain and decreased range of motion secondary to the resultant incongruency of the femoroacetabular joint, and has a disease course of up to 5 years until bone maturation occurs [3]. These hip changes can lead to pain and decreased mobility, with early joint degeneration often necessitating orthopedic management in early adulthood [4, 5]. We present this case study of a patient with TRPS1 who was known to the orthopedic service from the age of 10 and later found to have developed hip pathology at an older age than would typically be expected.
| Case Report | ▴Top |
Investigations
The early adolescent female was born via normal spontaneous delivery at term to nonconsanguineous parents. She was well at birth with no requirement for high dependency care. Her early developmental milestones were unremarkable and she first walked at 15 months of age. She was on the lower centiles for height and weight. At the age of 7 years, she was diagnosed with TRPS1 by a clinical geneticist after her patients had raised concerns about fine, slow-growing hair, fragile nails and generalized joint laxity.
At the age of 10 years, the patient was first referred to the pediatric orthopedic department for assessment of left foot pain. At this time, she reported difficulty with running but was able to participate in thrice weekly dance lessons and physical education (PE) at school. A full examination was completed, with main findings being that of bilateral planovalgus feet. She had a full and symmetrical range of motion in both hips. Baseline X-rays revealed cone epiphyses of the great toes, a common finding in TRPS, and normal hips (Fig. 1). She was referred for custom-made orthotic insoles and given a strengthening programme. On follow-up assessment, the foot pain had improved and she was discharged from pediatric orthopedics 16 months after referral.
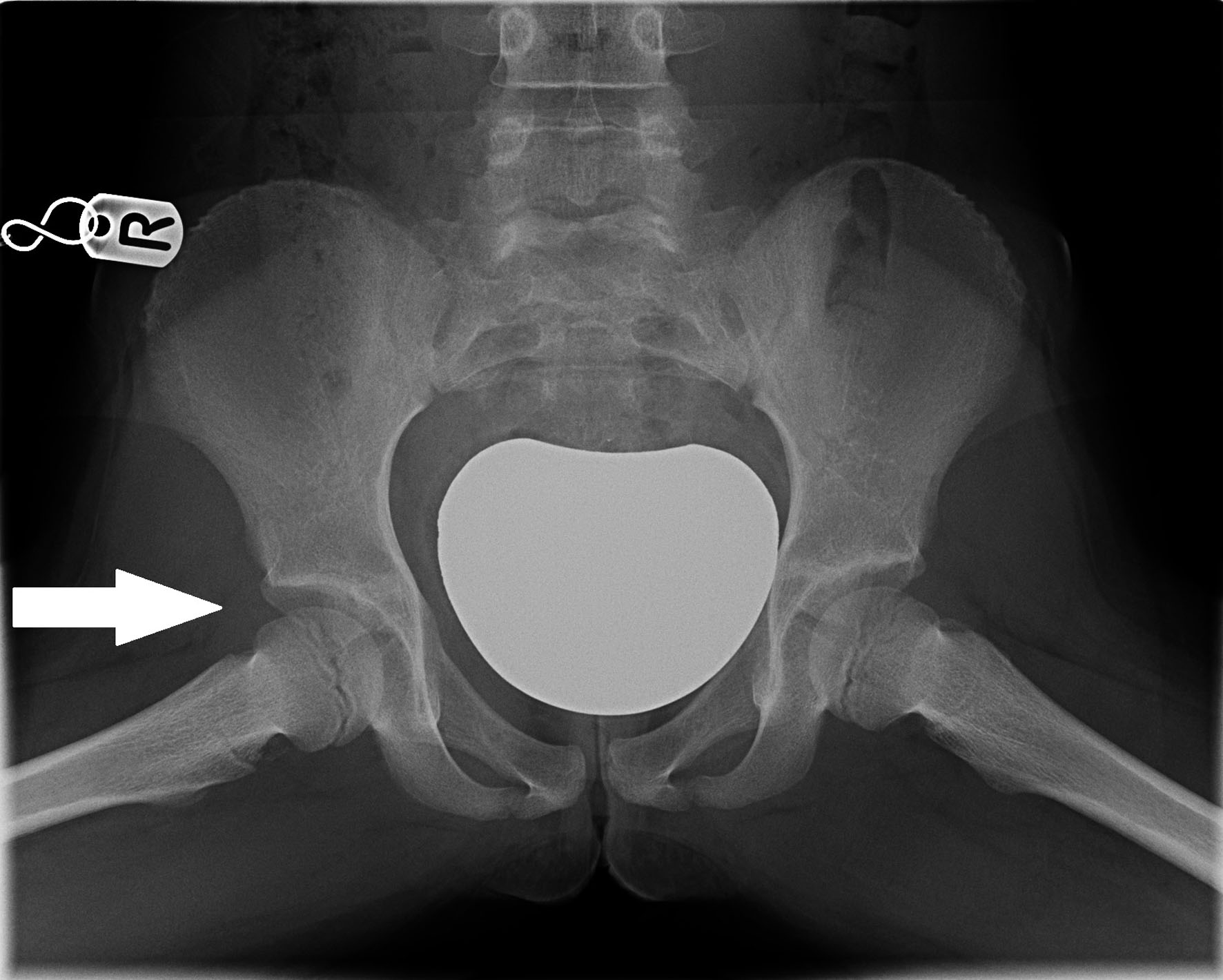 Click for large image | Figure 1. Aged 10, normal clinical assessment. |
One year later, at the age of 12 years and 11 months, the patient presented to the emergency department (ED) reporting a 2-week history of atraumatic insidious onset right-sided thigh and groin pain. On examination, she had a full passive and active range of motion in both hips. Blood tests (including full blood count (FBC), C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR)) were normal and an X-ray of both hips was unremarkable (Fig. 2). She was given a diagnosis of biomechanical hip pain and referred to the physiotherapy department.
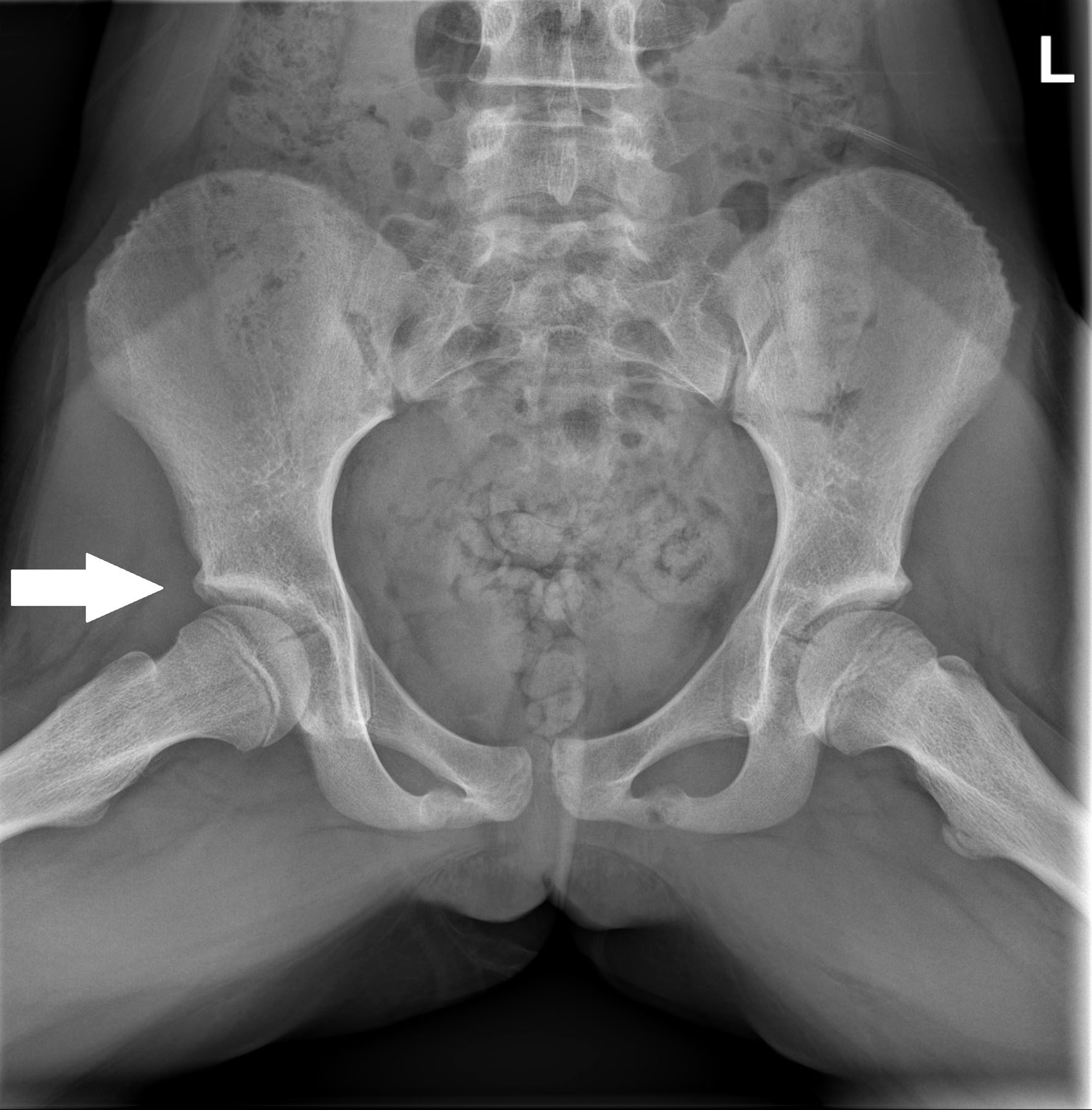 Click for large image | Figure 2. Two-week history of insidious onset pain reported. Normal clinical assessment. |
At her initial physiotherapy assessment 1 month later, the patient reported temporarily stopping all physical exercise which had led to an improvement in her symptoms. She had had no pain during activities of daily living over the preceding 2 weeks. She had then gradually restarted dance lessons and PE at school without any problems. On examination, she had a normal gait pattern; however, internal and external right hip rotation was restricted compared to the contralateral side. It was unclear whether the restriction was due to pain or true joint stiffness. A review was requested with a member of the pediatric orthopedic team and she was seen in clinic 6 weeks later. At this time, she reported improving symptoms and had regained a full passive range of right hip motion with some pain at the extremes of movement.
The patient continued to show a gradual improvement in pain and stiffness over the following 6 months. A routine physiotherapy follow-up appointment examination revealed a mild right-sided limp and increased pain at extremes of right hip movement. Three weeks later, she re-presented with a worsening limp and increasing hip pain. She had reduced weight-bearing on the right side with the right hip held in a flexed position. She was Trendelenburg positive on the right side. Passive range of right hip motion was restricted with 110° flexion, 5° fixed flexion, 20° abduction with the hip flexed, 20° internal rotation and 20° external rotation. An X-ray performed on this day showed flattening of the right femoral head, more obvious on the frog-lateral view (Fig. 3). The patient was diagnosed with avascular necrosis of the femoral head, or Perthes disease, 6 months after her presentation to ED, at the age of 13. This was 2.5 years after she was first seen by the pediatric orthopedic team with foot pain and occasional hip pain.
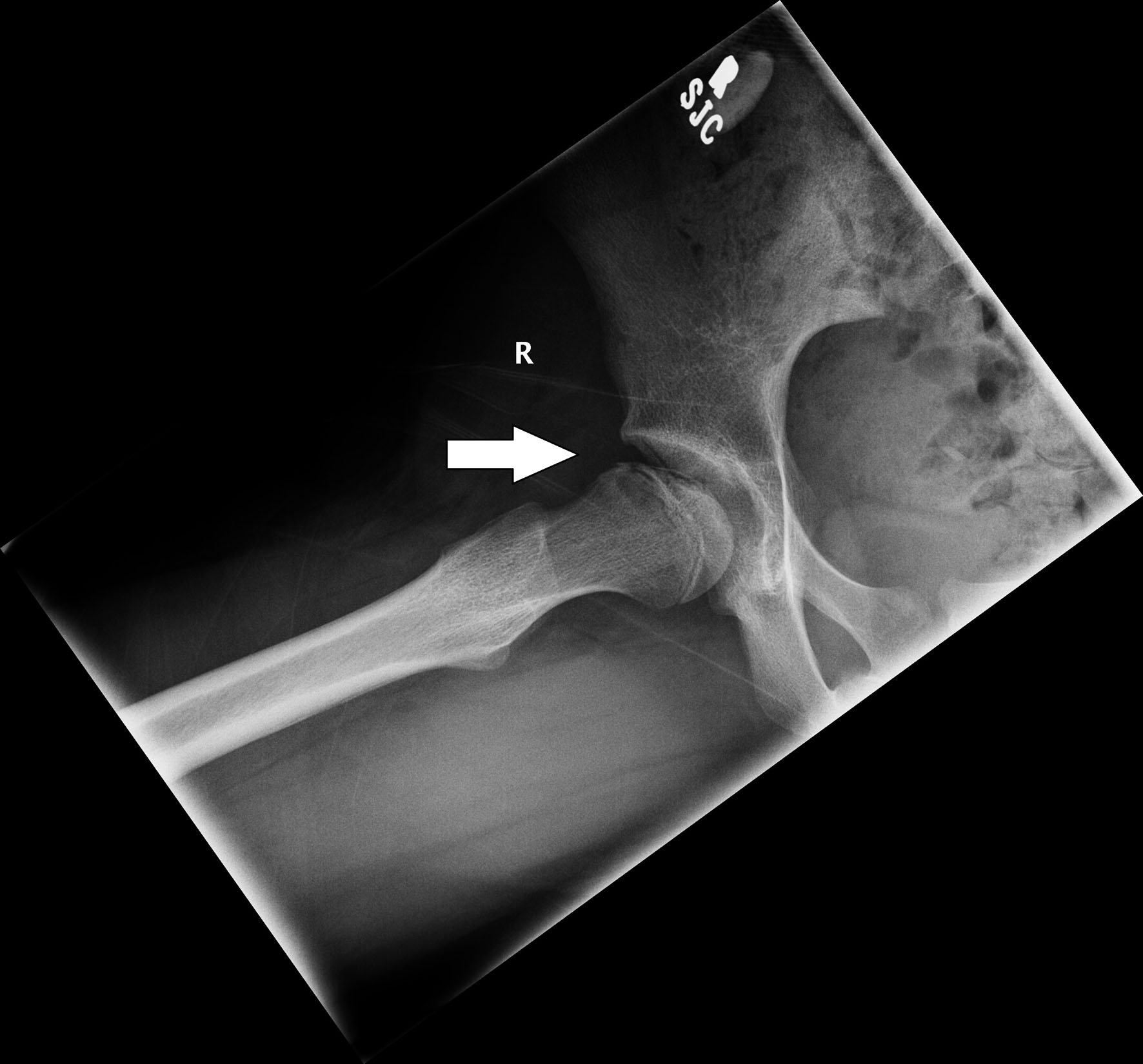 Click for large image | Figure 3. Reduced range of movement on assessment and flattening of femoral head noted on imaging. |
Diagnosis
During the months following initial physiotherapy referral, the clinical and radiographic findings were consistent with possible hypermobility related biomechanical joint pain or femoracetabular impingement. There was evidence of slightly reduced muscle tone and a Beighton score of 6/9. There were no other differential diagnoses at this time and Perthes disease was not suspected as radiographic findings were normal. Magnetic resonance imaging (MRI) was not requested, as patient reported symptoms and clinical examination including hip range of motion and strength was improving.
When the patient’s symptoms worsened, this original diagnosis was questioned. New hip X-rays revealed avascular necrosis of the femoral head and Perthes disease was diagnosed. Subsequent serial X-rays of the right hip showed gradual reduction in the height of the femoral epiphysis, together with metaphyseal cyst formation, confirming the diagnosis (Figs. 4, 5). The patient was prescribed low level strengthening exercises in non-weight bearing positions for the hip abductors and external rotators, and advised to continue with low impact activity such as swimming.
 Click for large image | Figure 4. Antero-posterior radiograph of both hips showing progressive signs of avascular necrosis of the right hip with loss of height of the epiphysis. |
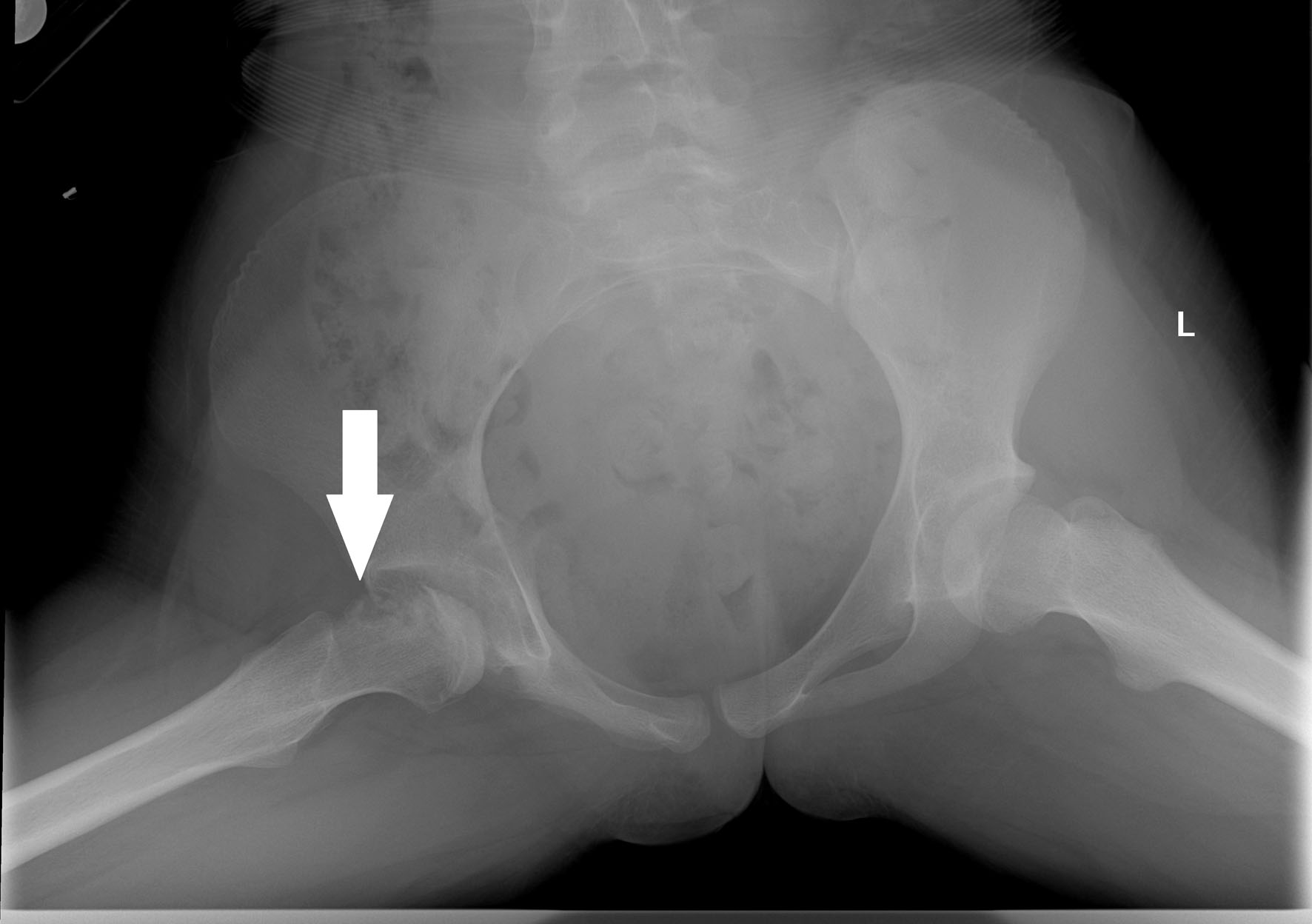 Click for large image | Figure 5. Frog-lateral view of both hips showing loss of epiphyseal height together with metaphyseal cysts. |
Treatment
Physiotherapy input continued following the diagnosis of Perthes disease. Physiotherapy sessions were provided more frequently with more focus on regaining hip joint range of motion as well as pain management advice. The patient participated in physiotherapist-lead hydrotherapy sessions as well as the continuation of a home exercise program. Initial exercises in both the land and water-based sessions involved active and passive stretches into hip flexion and internal rotation which were noted to be the most restricted at that time. A wheelchair and crutches were used for symptomatic relief when needed but maintenance of active mobility was encouraged. Management of pain was an ongoing problem. The aspherical femoral head led to abnormal hip biomechanics causing inflammation and synovitis. A steroid injection was given which provided good pain relief and allowed better engagement with physiotherapy. Exercises were able to be progressed to include more strengthening work at this time, predominantly for the gluteal muscles which had become severely deconditioned as range of motion had become more restricted.
Follow-up and outcomes
The steroid injection provided reasonable pain relief for 4 months and the patient was able to wean off crutches for all functional activities of daily living, including school. It allowed ongoing engagement with physiotherapy, and progressive strengthening exercises led to functional improvements. A hip arthrogram performed at the time of steroid injection confirmed the absence of hinge abduction. She continued to walk with an antalgic gait and she had ongoing stiffness of all hip movements, most notably internal and external rotation but this was much less painful. Hydrotherapy and land-based physiotherapy sessions continued with the aim of further improving strength and range of motion. Physiotherapy still continues at this time in the form of a home exercise program with clinical reviews at regular intervals, together with oral anti-inflammatory medication, with the aim of maintaining a congruent hip, managing symptoms and optimizing long-term outcomes.
| Discussion | ▴Top |
Pathological hip changes in patients with TRPS1 have been reported with a prevalence as high as 70% across different types of TRPS [5]. In 2015, Maas et al evaluated the phenotype and genotype of 103 patients with TRPS and found evidence of coxa plana in 40%, and hip dysplasia in 38% patients with TRPS1 [6]. Age of symptom onset and the specific disease process has not been reported in the literature.
One case study describes avascular necrosis of the femoral head in a 7-year-old female with TRPS1, consistent with the expected age of presentation for Perthes disease [7]. Naselli et al describe a case study of twin girls with TRPS1, with one twin presenting with hip pain at first admission. There was no record of when the hip pain started but arthrotomy and excision of part of the femoral head was performed at 12 years of age [8]. Similarly, Sawano et al reported a 12-year-old female with hip pain after long distance running with radiography revealing bilateral acetabular dysplasia. In this case, both femoral heads remained spherical with no evidence of Perthes-like changes. Acetabular osteotomies were performed sequentially at ages of 13 and 14 years [3].
In idiopathic Perthes disease, presentation is most commonly seen between the age of 4 and 9 years. Rarely, the onset of Perthes disease is in adolescence where the usual pattern of disease evolution, with revascularization of the femoral head, remains incomplete. This leads to significantly poorer longer-term outcomes [9]. In this case study, the age of presentation is much later than expected for Perthes disease. A possible cause of this is the abnormal skeletal maturation seen in TRPS, whereby skeletal age lags behind chronological age [8].
The pathogenesis of Perthes disease remains unclear and there is evidence of a different pathological disease process in patients with TRPS. As a consequence, the term “Perthes-like” disease is often used to describe the avascular hip changes. It is clear that the hip pathologies described in this population lead to pain, decreased mobility and often surgical intervention, particularly in those with later onset.
Age at diagnosis and the extent of femoral head involvement are the most common classifications used to predict long-term outcomes. A prospective study of 425 affected hips over a 5-year period concluded that there was no difference in prognosis between conservative and surgical treatments for those under the age of 6, but for those over the age of 6 with greater than 50% femoral head involvement, there were significantly improved outcomes following surgical intervention (proximal femoral varus osteotomy) [10]. Various surgical options are available, with the primary aim of containing the head of the femur within the acetabulum in order to restore joint congruency and reduce femoracetabular impingement. It has been suggested that for older patients who have less remodelling potential, a combined treatment involving a pelvic osteotomy as well as a femoral osteotomy has improved outcomes [11].
Early identification of hip joint changes is crucial in ensuring that the patient receives optimal treatment, as prognosis worsens as age increases. This includes regular therapy input for pain management and maintenance of hip range of movement. This supports the remodelling and revascularization process of the femoral head with the aim of reducing the risk of hinge abduction (the head of the femur failing to remain enlocated and instead hinging on the lateral edge of the acetabulum) occurring that leads to further joint incongruency [12]. With this in mind, keeping Perthes disease at the forefront of our minds during physiotherapy assessments irrespective of age, ensuring that a thorough past medical history is obtained, and having the service provision to obtain X-ray imaging and refer quickly for an orthopedic opinion is vital to ensure that these cases are not missed.
Learning points
Presentation of hip pathology may be later in patients with tricho-rhino-phalangeal syndrome.
Keep a high index of suspicion for Perthes disease in patients presenting with non-traumatic hip pain regardless of age of onset.
Timely diagnosis of Perthes-like disease is important to allow early commencement of potentially joint-preserving therapy input and advice.
Acknowledgments
None to declare.
Financial Disclosure
A bursary covering publication costs was awarded to the first author from the Association of Chartered Paediatric Physiotherapists, UK.
Conflict of Interest
The authors declare no conflict of interest.
Informed Consent
Informed consent for publication of this report was obtained from the patient and her legal guardian.
Author Contributions
Both authors were directly involved in the patient’s care. The first author Faye Grace (Specialist Paediatric Physiotherapist) was responsible for drafting of the text; sourcing and editing of clinical images; and was responsible for obtaining informed consent from the patient and legal guardians. The second author Elizabeth Ashby (Consultant Paediatric Orthopaedic Surgeon) was the clinician in charge of the clinical care of the patient and supervised the preparation of the manuscript.
Data Availability
Any inquiries regarding supporting data availability of this study should be directed to the corresponding author.
Abbreviations
CRP: C-reactive protein; ED: emergency department; ESR: erythrocyte sedimentation rate; FBC: full blood count; PE: physical education; TRPS1: tricho-rhino-phalangeal syndrome type 1
| References | ▴Top |
- Giedion A. [Tricho-rhino-phalangeal syndrome]. Helv Paediatr Acta. 1966;21(5):475-485.
pubmed - Giedion A, Burdea M, Fruchter Z, Meloni T, Trosc V. Autosomal-dominant transmission of the tricho-rhino-phalangeal syndrome. Report of 4 unrelated families, review of 60 cases. Helv Paediatr Acta. 1973;28(3):249-259.
pubmed - Sawano K, Nyuzuki H, Nagasaki K, Suzuki H, Suda K, Miyasaka D, Imai N, et al. A case of adolescent trichorhinophalangeal syndrome undergoing pelvic osteotomy for bilateral acetabular dysplasia. J Orthop Sci. 2021.
doi pubmed - Dunbar JD, Sussman MD, Aiona MD. Hip pathology in the trichorhinophalangeal syndrome. J Pediatr Orthop. 1995;15(3):381-385.
doi pubmed - Ludecke HJ, Schaper J, Meinecke P, Momeni P, Gross S, von Holtum D, Hirche H, et al. Genotypic and phenotypic spectrum in tricho-rhino-phalangeal syndrome types I and III. Am J Hum Genet. 2001;68(1):81-91.
doi pubmed pmc - Maas SM, Shaw AC, Bikker H, Ludecke HJ, van der Tuin K, Badura-Stronka M, Belligni E, et al. Phenotype and genotype in 103 patients with tricho-rhino-phalangeal syndrome. Eur J Med Genet. 2015;58(5):279-292.
doi pubmed - Minguella I, Ubierna M, Escola J, Roca A, Prats J, Pintos-Morell G. Trichorhinophalangeal syndrome, type I, with avascular necrosis of the femoral head. Acta Paediatr. 1993;82(3):329-330.
doi pubmed - Naselli A, Vignolo M, Di Battista E, Papale V, Aicardi G, Becchetti S, Toma P. Trichorhinophalangeal syndrome type I in monozygotic twins discordant for hip pathology. Report on the morphological evolution of cone-shaped epiphyses and the unusual pattern of skeletal maturation. Pediatr Radiol. 1998;28(11):851-855.
doi pubmed - Joseph B. Natural history of early onset and late-onset Legg-Calve-Perthes disease. J Pediatr Orthop. 2011;31(2 Suppl):S152-S155.
doi pubmed - Wiig O, Terjesen T, Svenningsen S. Prognostic factors and outcome of treatment in Perthes' disease: a prospective study of 368 patients with five-year follow-up. J Bone Joint Surg Br. 2008;90(10):1364-1371.
doi pubmed - Maleki A, Qoreishy SM, Bahrami MN. Surgical treatments for Legg-Calve-Perthes disease: comprehensive review. Interact J Med Res. 2021;10(2):e27075.
doi pubmed pmc - El-Harbiti A, Hailer YD. Range of abduction in patients with Legg-Calve-Perthes disease - a nationwide register-based cohort study. BMC Musculoskelet Disord. 2020;21(1):718.
doi pubmed pmc
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


