| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 14, Number 7, July 2023, pages 255-259
Mucosa-Associated Lymphoid Tissue Lymphoma of the Ascending Colon Successfully Removed With Endoscopic Submucosal Dissection
Grigorios Petrousisa, e, Simone Ignatovab, Maria Xintarac, Spyridon Vrakasd, Dimitrios Karapiperisa
aDepartment of Internal Medicine, Section of Gastroenterology, Vrinnevi Hospital, Norrkoping, Sweden
bDepartment of Pathology, Linkopings University Hospital, Linkoping, Sweden
cDepartment of Ophthalmology, Linkopings University Hospital, Linkoping, Sweden
dDepartment of Gastroenterology Tzaneion General Hospital, Piraeus, Greece
eCorresponding Author: Grigorios Petrousis, Department of Internal Medicine, Section of Gastroenterology, Vrinnevi Hospital, Norrkoping, Sweden
Manuscript submitted June 10, 2023, accepted July 18, 2023, published online July 31, 2023
Short title: ESD Successfully Removed Colonic MALToma
doi: https://doi.org/10.14740/jmc4121
| Abstract | ▴Top |
Mucosa-associated lymphoid tissue (MALT) lymphoma is a type of non-Hodgkin lymphoma with characteristic histopathological features and can occur in various extranodal sites, including the gastrointestinal tract. While gastric MALT lymphoma has been extensively researched, primary lymphoma presentation in the colorectal mucosa is rare and lacks any association with Helicobacter pylori infection. Furthermore, there are currently no standardized treatment guidelines for this condition. This report presents a rare case of primary MALT lymphoma that manifested as a broad-based polyp. The diagnosis was confirmed through histopathological and immunohistochemical examination, and the polyp was resected endoscopically with the endoscopic submucosal dissection technique.
Keywords: Mucosa-associated lymphoid tissue lymphoma; Colonoscopy; Endoscopic submucosal dissection; Ascending colon
| Introduction | ▴Top |
Mucosa-associated lymphoid tissue (MALT) lymphoma is a type of non-Hodgkin lymphoma (NHL) that appears in different extranodal sites, and the gastrointestinal (GI) tract emerges to be the most common [1]. Compared to the stomach which is the most frequent site of occurrence in the GI tract, primary colonic MALT lymphoma (MALToma) is rare and shares no typical association with Helicobacter pylori (HP) infection [1-3]. MALToma of the colon can present with a broad spectrum of clinical signs and symptoms [4] and different endoscopic manifestations [2]. As a result of its rarity, the etiopathogenesis of this condition along with treatment guidelines are not yet established [5]. We present an uncommon case of a primary MALToma of the colon, discovered during a colonoscopy and successfully resected with endoscopic submucosal dissection (ESD) without the use of adjuvant chemotherapy or immunotherapy.
| Case Report | ▴Top |
Investigations
Our case report describes a 75-year-old female with a history of bowel habit changes who was referred to the Endoscopic Department of our hospital to undergo a colonoscopy. The patient presented numerous times to her primary care physician in the past year due to repeated episodes of abnormal loose and watery stools, lasting several weeks. These episodes resolved spontaneously, followed by periods where the patient described normal bowel habits. The patient has a past medical history of hypertension, hyperlipidemia, right-sided nephrectomy due to a benign kidney tumor, and a lateral intraductal papillary mucinous neoplasm (IPMN) localized in the head of the pancreas. She has no history of excessive alcohol use or smoking. Physical examination revealed no signs of systemic illness, and laboratory test results were unremarkable.
A follow-up computed tomography (CT) of the abdomen and pelvis for her IPMN demonstrated a round, well-demarcated lesion in the ascending colon and no other signs of enlarged lymph nodes in the abdominal cavity or hepatosplenomegaly. Considering the patient’s previous history of sudden changes in her bowel habits and this radiological finding, we performed a colonoscopy, which revealed an approximately 2 cm broad-based polypoid lesion in the ascending colon (Fig. 1).
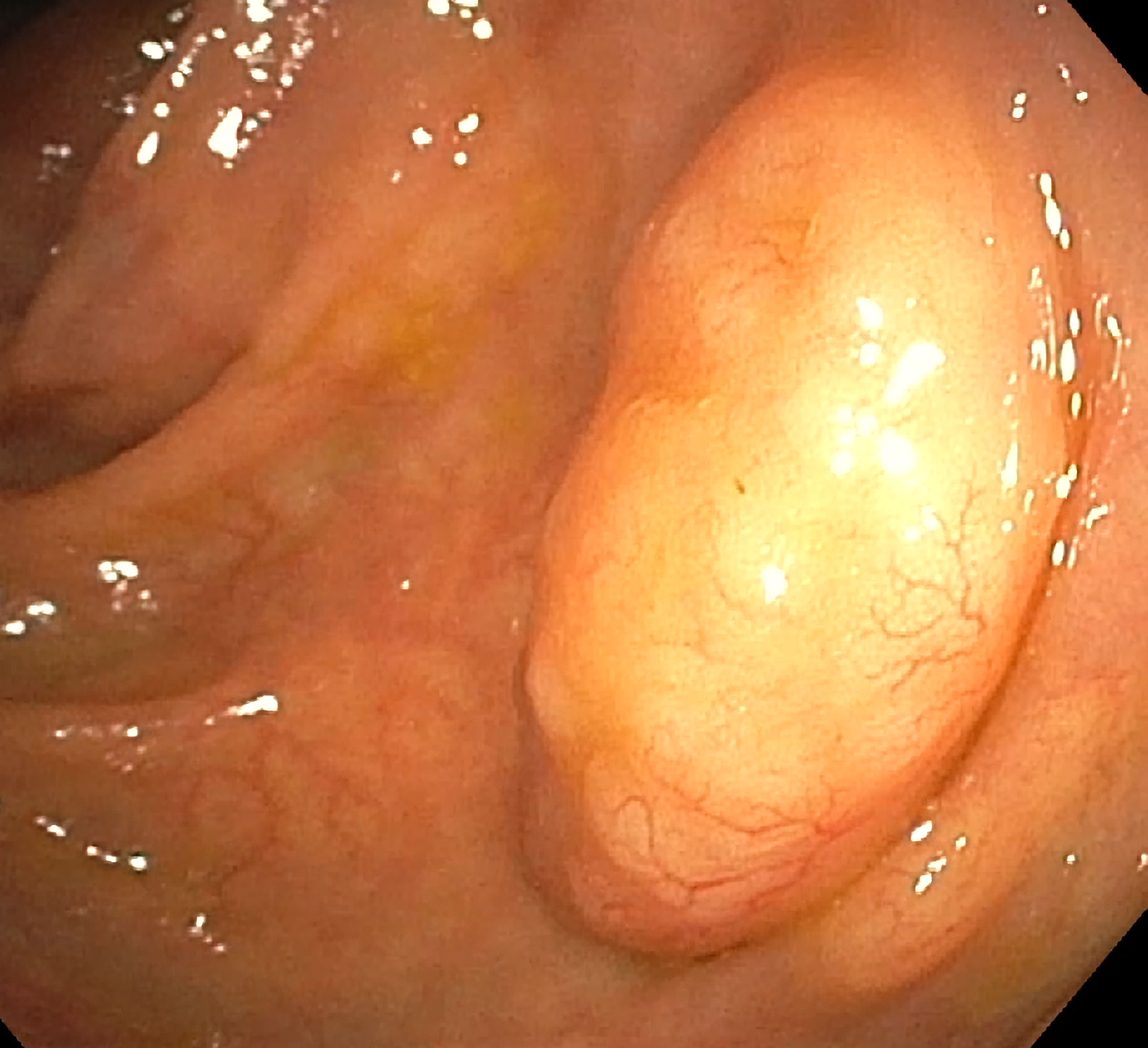 Click for large image | Figure 1. Colonoscopy image of the broad-based polyp in the ascending colon. |
Histologic analysis of the biopsy specimens disclosed diffuse lymphocytic infiltration of the colonic mucosa and submucosa (Fig. 2), which immunohistochemically stained positive for B-lymphocyte markers CD20 and Bcl-2 (Fig. 3), and negative for CD3, CD5, CD10, and cyclin D1. Immunostaining of the light chains revealed a dominance in the expression of the lambda chains with a 1/10 kappa to lambda chain ratio. Furthermore, the Ki-67 proliferation index was 36%. These findings were compatible with non-Hodgkin B-cell marginal zone lymphoma.
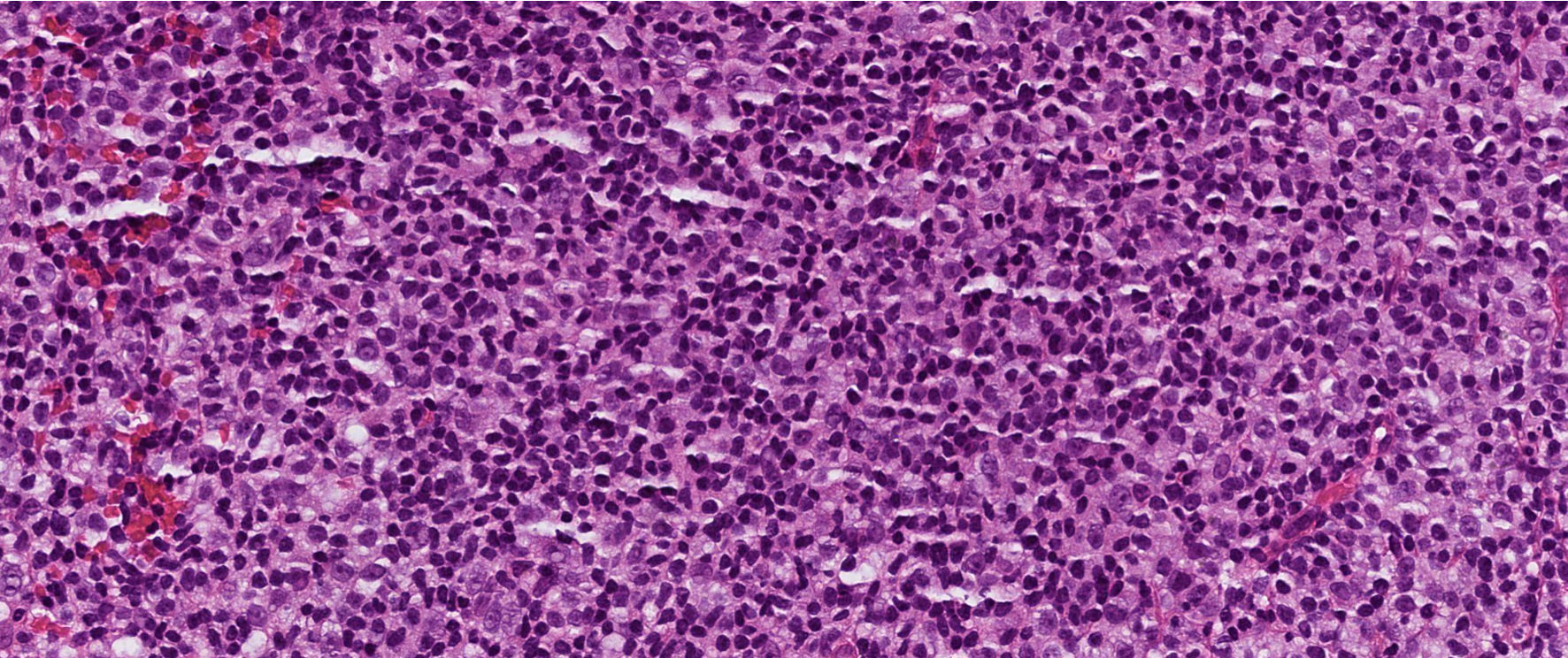 Click for large image | Figure 2. Histologic findings in hematoxylin and eosin stain revealing a vaguely nodular infiltration of small- to medium-sized lymphocytes with only a few scattered atypical cells in the mucosa and submucosa. |
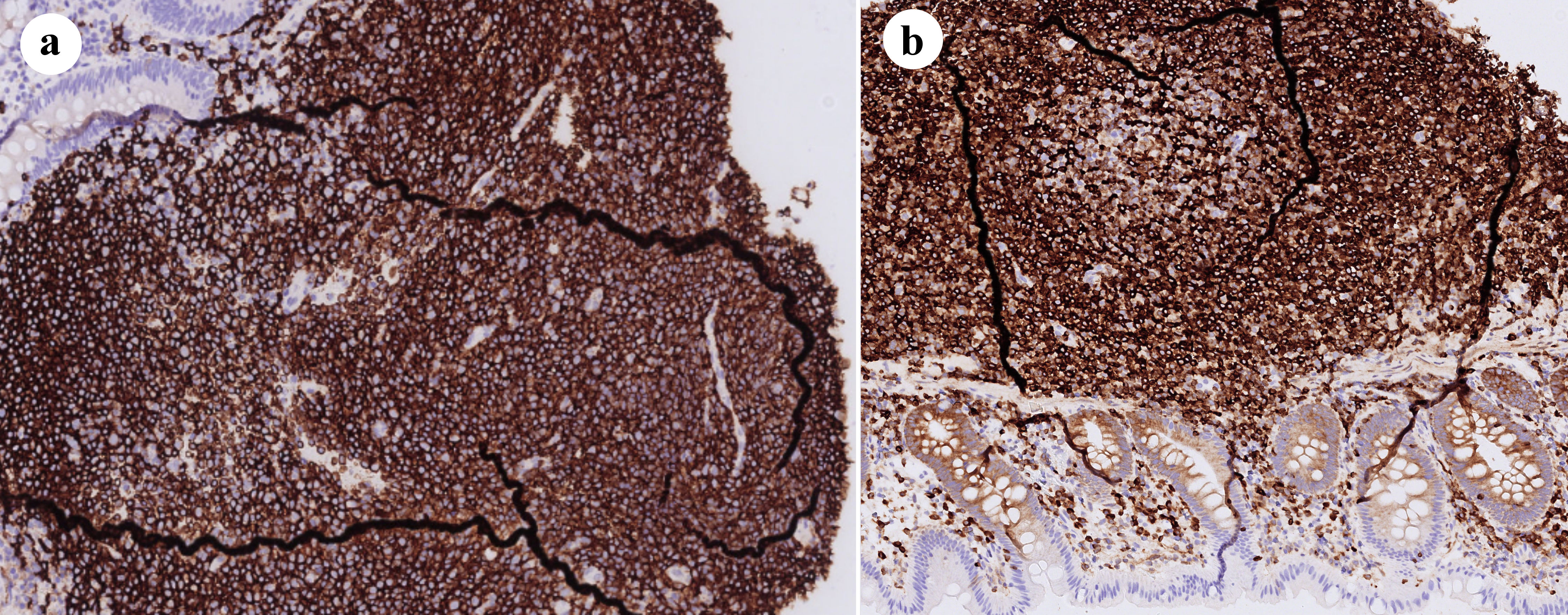 Click for large image | Figure 3. (a) Immunohistochemical stain for CD20 showed that the infiltrate dominates almost entirely of CD20+ B cells. (b) Immunohistochemistry was positive for Bcl-2. |
Diagnosis
An esophagogastroduodenoscopy (EGD) with multiple biopsies was normal and revealed no sign of HP infection. Additional imaging with CT of the neck and chest revealed a borderline enlarged submental lymph node. Ultrasound-guided fine needle aspiration biopsy was performed, and the results showed no signs of lymphocytic infiltration. All these findings were sufficient to set the diagnosis of primary extranodal MALToma of the colon. The patient was classified as stage IE, according to the Lugano lymphoma staging classification.
Treatment
After a multidisciplinary team meeting, the therapeutic decision was to perform a polypectomy with an ESD procedure without additional treatment with rituximab or adjuvant chemotherapy. Histological and immunohistochemical analysis of the dissected polypoid lesion reconfirmed the diagnosis.
Follow-up and outcomes
The patient’s condition remains stable, and she is undergoing follow-up care through the Hematology Section of our hospital. A control colonoscopy has been scheduled for her in the coming months.
| Discussion | ▴Top |
MALToma is a widely-known malignancy that was first introduced by Isaacson et al in 1983 [6] and is an uncommon type of NHL that occurs in extranodal sites, such as the GI tract. Other extranodal sites vary and can involve the lungs, the salivary glands, the ocular adnexa, the breast, the skin, and the soft tissue [1, 7]. In the majority, these sites do not comprise native lymphoid tissue, however numerous specific chronic immune responses due to infectious and other stimulus agents result in lymphoid transformation and stepwise lymphoid growth. Even though MALToma emerges in many different anatomical sites, the histopathological and immunohistochemical characteristics are the same. The most predominant site of appearance is the stomach and is thoroughly known to be strongly associated with HP infection [2, 3, 7]. Primary colonic MALToma is a rare type of B-cell NHL, representing only 2.5% of all MALTomas [8] and less than 0.6% of all colorectal malignancies [9]. It manifests with the highest frequency between the fifth and the seventh decade of life [1]; and recent reviews demonstrate a female predominance with a 2:1 ratio in comparison to the males [1, 3, 10]. Treatment approaches are currently under debate and include a variety of immunosuppressive and surgical strategies or even a combination of them.
The etiopathogenesis of colonic MALToma is not yet clarified, possibly due to its rarity. However, some proposed pathophysiological mechanisms include not only the well-known immune cross-reactivity induced by chronic infections (HP, hepatitis C virus) but also the chronic inflammatory response of the mucosa driven by autoimmune or immune-mediated diseases [3, 11].
Histology stands as the gold standard to set the diagnosis of colon MALToma. According to the World Health Organization (WHO) classification of lymphoid neoplasms revised in 2017, the diagnosis is established and estimated by the origin of the cellular proliferation along with certain morphological and immunohistochemical criteria [2, 5, 12, 13].
There is no standardized staging procedure for colorectal MALToma, but a typical screening that includes EGD, ileocolonoscopy, CT thorax and abdomen, and a bone marrow biopsy is recommended as a first approach [7], completed by secondary targeted imaging based on clinical evaluation [14].
Clinical aspects of MALToma of the colon differ from asymptomatic cases with incidental lymphoma findings during a routine control [8, 10], to rare cases with acute intestinal obstruction [10]. From an endoscopic perspective, the right colon and the rectum are the most typical sites of manifestation [9, 10, 15], usually presenting as a single flat, elevated, or semi-pedunculated polypoid lesion [2, 3, 9, 10].
Due to its rarity, colonic MALToma has not been exhaustively studied and a standard treatment process has not yet been designed [1, 5, 7, 8]. First-line treatment is currently under debate and varies from watch-and-wait strategies to combination therapy with immunosuppression and surgery [7, 10]. Merely 20% of extragastric MALToma tested positive for HP and most cases that were first treated with eradication therapy received supplementary treatment to achieve clinical remission [7, 15]. A large number of patients with advanced disease were treated with surgery, radiotherapy, chemotherapy, immunotherapy with rituximab, or a combination of these, with the majority of the therapeutic approaches demonstrating successful results [1-3, 7, 9, 15]. Nowadays, for patients with low-grade localized lymphoma, many case studies describe treatment approaches with endoscopic resection. Low-invasive techniques with endoscopic mucosal resection (EMR) or ESD have shown prosperous results with a low rate of lymphoma regression during follow-ups, either as monotherapy [1, 3, 10, 16-20] or as a complementation therapy, in patients with large obstructive lesions, after a downsize treatment [3].
Conclusions
Colonic MALT lymphoma is a rare subtype of B-cell NHL, with typical histological and immunophenotypical findings, occurring with a variety of clinical manifestations as well as endoscopic appearances. Even though there is still a debate over the therapeutic approaches, endoscopic interventions such as EMR and ESD for resectable lesions, are gaining ground in patients with localized disease compared to surgical procedures and chemotherapy or immunotherapy.
Learning points
MALT lymphoma is a rare type of colon cancer and shares no association with HP infection. Even though there are no standardized guidelines for treatment and follow-up, a wide variety of first-line treatment options, such as surgery and/or chemotherapy, and immunotherapy, appear to have good therapeutic results. In the current era of advanced endoscopy, minimally invasive techniques such as ESD, appear to achieve growing recognition as an effective therapeutic option for the treatment of colonic MALToma.
Acknowledgments
None to declare.
Financial Disclosure
The authors of this publication do not have any relevant financial disclosure.
Conflict of Interest
None to declare.
Informed Consent
Informed consent was obtained from the patient prior to publication.
Author Contributions
All authors contributed equally and actively to the writing process of this article. GP was the corresponding author, providing the clinical information, reviewing the literature, designing the work with DK. SI was involved by providing the histological and immunohistochemical pictures and by writing the histological and pathophysiological part of the case report. MX and SV contributed actively to the writing process by writing the therapy part of the manuscript, reviewing the literature, and participating in the final corrections before the manuscript was sent.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Won JH, Kim SM, Kim JW, Park JH, Kim JY. Clinical features, treatment and outcomes of colorectal mucosa-associated lymphoid tissue (MALT) lymphoma: literature reviews published in English between 1993 and 2017. Cancer Manag Res. 2019;11:8577-8587.
doi pubmed pmc - Hollie N, Asakrah S. MALT lymphoma of the colon: a clinicopathological review. J Clin Pathol. 2020;73(7):378-383.
doi pubmed - Ishikawa E, Nakamura M, Satou A, Shimada K, Nakamura S. Mucosa-associated lymphoid tissue (MALT) lymphoma in the gastrointestinal tract in the modern era. Cancers (Basel). 2022;14(2):446.
doi pubmed pmc - Panneerselvam K, Goyal S, Shirwaikar Thomas A. Ileo-colonic lymphoma: presentation, diagnosis, and management. Curr Opin Gastroenterol. 2021;37(1):52-58.
doi pubmed - Matsuo S, Mizuta Y, Hayashi T, Susumu S, Tsutsumi R, Azuma T, Yamaguchi S. Mucosa-associated lymphoid tissue lymphoma of the transverse colon: a case report. World J Gastroenterol. 2006;12(34):5573-5576.
doi pubmed pmc - Isaacson P, Wright DH. Malignant lymphoma of mucosa-associated lymphoid tissue. A distinctive type of B-cell lymphoma. Cancer. 1983;52(8):1410-1416.
doi pubmed - Abbas H, Niazi M, Makker J. Mucosa-associated lymphoid tissue (MALT) lymphoma of the colon: a case report and a literature review. Am J Case Rep. 2017;18:491-497.
doi pubmed pmc - Nagra N, Singhvi AR, Singhvi G. Mucosa-associated lymphoid tissue lymphoma of colon: a case report and literature review of rare entity. Cureus. 2020;12(3):e7438.
doi pubmed pmc - Dionigi G, Annoni M, Rovera F, Boni L, Villa F, Castano P, Bianchi V, et al. Primary colorectal lymphomas: review of the literature. Surg Oncol. 2007;16(Suppl 1):S169-S171.
doi pubmed - Jeon MK, So H, Huh J, Hwang HS, Hwang SW, Park SH, Yang DH, et al. Endoscopic features and clinical outcomes of colorectal mucosa-associated lymphoid tissue lymphoma. Gastrointest Endosc. 2018;87(2):529-539.
doi pubmed - Teixeira Mendes LS, Wotherspoon A. Marginal zone lymphoma: Associated autoimmunity and auto-immune disorders. Best Pract Res Clin Haematol. 2017;30(1-2):65-76.
doi pubmed - Kuper-Hommel MJ, van Krieken JH. Molecular pathogenesis and histologic and clinical features of extranodal marginal zone lymphomas of mucosa-associated lymphoid tissue type. Leuk Lymphoma. 2012;53(6):1032-1045.
doi pubmed - Swerdlow SH, et al. WHO classification of tumours of haematopoietic and lymphoid tissues. Accessed: June 04, 2023. [Online]. Available: https://publications.iarc.fr/Book-And-Report-Series/Who-Classification-Of-Tumours/WHO-Classification-Of-Tumours-Of-Haematopoietic-And-Lymphoid-Tissues-2017.
- Raderer M, Vorbeck F, Formanek M, Osterreicher C, Valencak J, Penz M, Kornek G, et al. Importance of extensive staging in patients with mucosa-associated lymphoid tissue (MALT)-type lymphoma. Br J Cancer. 2000;83(4):454-457.
doi pubmed pmc - Okamura T, Suga T, Iwaya Y, Ito T, Yokosawa S, Arakura N, Ota H, et al. Helicobacter pylori-negative primary rectal MALT lymphoma: complete remission after radiotherapy. Case Rep Gastroenterol. 2012;6(2):319-327.
doi pubmed pmc - Ahlawat S, Kanber Y, Charabaty-Pishvaian A, Ozdemirli M, Cohen P, Benjamin S, Haddad N. Primary mucosa-associated lymphoid tissue (MALT) lymphoma occurring in the rectum: a case report and review of the literature. South Med J. 2006;99(12):1378-1384.
doi pubmed - Kim MH, Jung JT, Kim EJ, Kim TW, Kim SY, Kwon JG, Kim EY, et al. A case of mucosa-associated lymphoid tissue lymphoma of the sigmoid colon presenting as a semipedunculated polyp. Clin Endosc. 2014;47(2):192-196.
doi pubmed pmc - Chakinala RC, Haq KF, Barsa JE, Solanki S, Chawla L, Khan MA, Farooq T, et al. Incidentally discovered extranodal marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue in the colon. Case Rep Med. 2017;2017:1505706.
doi pubmed pmc - Schwartz BL, Lowe RC. Successful endoscopic resection of mucosa-associated lymphoid tissue lymphoma of the colon. ACG Case Rep J. 2019;6(10):e00228.
doi pubmed pmc - Han J, Zhu Z, Zhang C, Xie HP. Successful endoscopic resection of primary rectal mucosa-associated lymphoid tissue lymphoma by endoscopic submucosal dissection: a case report. Front Med (Lausanne). 2021;8:715256.
doi pubmed pmc
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


