| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 13, Number 9, September 2022, pages 456-461
Resolution of Odontogenic Sinus Pathosis by Endodontic Microsurgery
Pablo Alejandro Rodrigueza , Romina Chaintiou Piornoa
, Eugenia Pilar Consoli Lizzia, b
aDepartment of Endodontics, School of Dentistry, University of Buenos Aires, Buenos Aires, Argentina
bCorresponding Author: Eugenia Pilar Consoli Lizzi, Department of Endodontics, School of Dentistry, University of Buenos Aires, Buenos Aires, Argentina
Manuscript submitted July 17, 2022, accepted September 8, 2022, published online September 28, 2022
Short title: Resolution of Odontogenic Sinus Pathosis
doi: https://doi.org/10.14740/jmc3982
| Abstract | ▴Top |
A case report is presented, in which a tooth with a chronic apical abscess that has caused a maxillary sinusitis was treated with an endodontic microsurgery. A 65-year-old female patient reported discomfort in a maxillary tooth gingiva. Clinically, a dental metal-ceramic bridge with adequate marginal adaptation, involving teeth from maxillary right canine to maxillary right second molar, was observed. The periapical radiograph showed the adequate adaptation of the crown and post in the maxillary right first premolar, an apical lesion, and the heavy thickening of the maxillary sinus floor mucosa. The diagnosis established in the maxillary right first premolar was of a previously treated tooth and a chronic apical abscess. Considering the accurate fixed prosthesis adaptation and the impossibility of disassembling the five-piece-metal-ceramic bridge to perform a new endodontic treatment and the prosthetic restoration, an endodontic microsurgery of this tooth was performed. The post-treatment follow-up of 12-month recall showed a normal thickness sinus membrane and a regenerating cortical bone. The proposed microsurgery has enabled the maintenance of the existing prosthetic rehabilitation of the tooth that caused the sinus pathosis.
Keywords: Endodontics; Cone-beam computed tomography; Microsurgery
| Introduction | ▴Top |
Endodontics is the branch of dentistry which is concerned with the morphology, physiology and pathosis of human dental pulp and periradicular tissues. Its study and practice encompass the basic clinical sciences including biology of the normal pulp, etiology, diagnosis, prevention and treatment of pulp diseases and injuries, as well as associated periradicular conditions [1]. A widely described technique for the periradicular and apical pathosis is endodontic surgery. The primary objective of this procedure is the same as that of the conventional root canal treatment: to promote suitable conditions for achieving the periradicular tissues healing and repair. This technique involves removing the necrotic tissue as well as the tissue degradation products, the bacteria remaining in the root canal systems, and the root apex. Likewise, it proposes the creation of a fluid-tight seal at the root-end by using biocompatible materials [2, 3].
Endodontic surgery has evolved over the last decades into what is currently termed “endodontic microsurgery”. The microsurgery enables more conservative and predictable surgical maneuvers, the use of biomaterials induces an adequate tissue repair response [4], and the gingival and periodontal tissues are maintained intact from functional and aesthetic viewpoints [5].
The need of treating persistent periradicular lesions seen in long-term follow-ups, the unreachable root access or non-preserved apical anatomy, or cases of advanced calcification of the root canal and lesions involving more than three teeth are indications for endodontic microsurgery [6]. Its application has been even described in the case of a lateral canal and lateral perforations treatment [7, 8].
Sinusitis is a pathological entity characterized by the inflammation of the sinus mucosa, and when resulting from a dental condition is defined as odontogenic sinusitis [9]. The maxillary posterior teeth in closer anatomical proximity to the maxillary sinus floor, and the maxillary premolars in a lesser degree of proximity, are the teeth with the highest closeness to the maxillary sinus [10]. The aim of this work is to present a case report of a patient with an odontogenic sinus pathosis resolved by means of an endodontic microsurgical approach, and to describe the successful resolution in a medium-term clinical and tomographic follow-up.
| Case Report | ▴Top |
Investigations
A 65-year-old female patient with an uneventful medical history presented to the Department of Endodontics, School of Dentistry of the University of Buenos Aires, Argentina, reporting discomfort in a maxillary tooth gingiva. The patient consultation was carried out during the pandemic of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), a period in which mandatory quarantine and lockdown measures were enacted by the national executive branch.
Diagnosis
Clinically, a metal-ceramic bridge with adequate marginal adaptation, involving teeth from 13 to 17, was observed. In the teeth 13, 14 and 17, abutments with metal intraradicular retention were seen. A sinus tract in the attached gingiva at the buccal aspect of the tooth 15, part of the bridge span, was checked (Fig. 1a, b). In the periapical radiograph, the adequate adaptation of the crown and post in the tooth 14, an apical lesion associated with this tooth and the heavy thickening of the maxillary sinus floor mucosa were detected (Fig. 1c). A cone-beam computed tomographic scan (CBCT) scan was requested to evaluate the current dimensions of the sinus lesion and to design the treatment plan (Fig. 2). The diagnosis established in the tooth 14 was of a previously treated tooth and a chronic apical abscess.
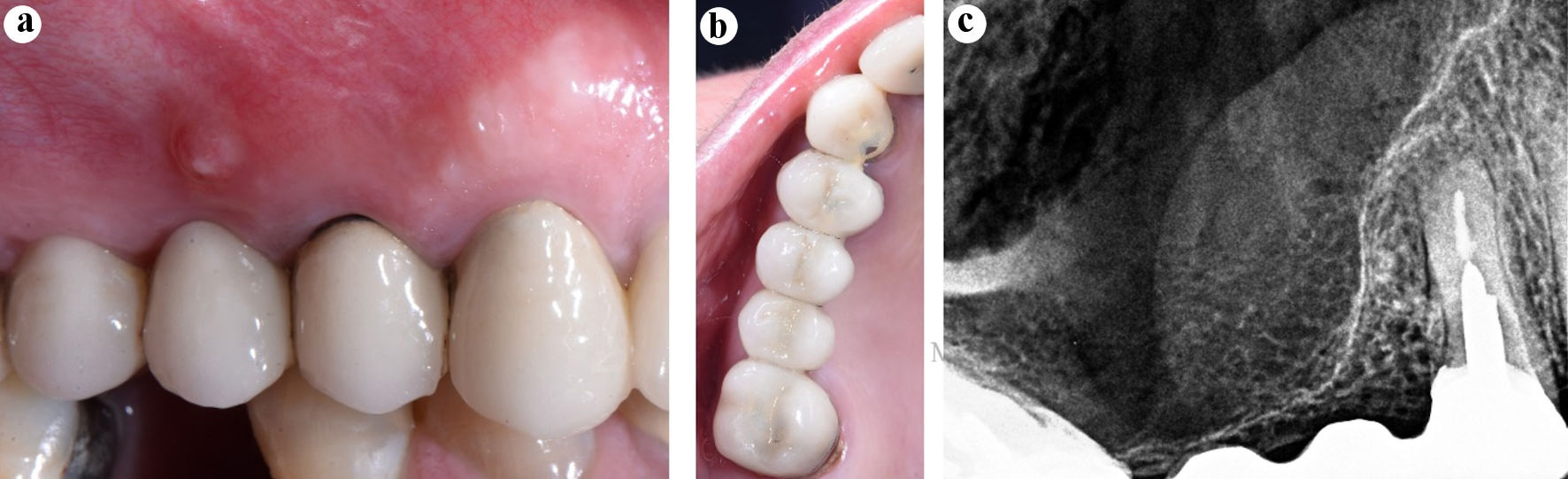 Click for large image | Figure 1. Diagnosis. (a) Preoperative clinical image, the sinus tract in the attached gingiva of the tooth 15 (bridge span). (b) Preoperative clinical image, occlusal view. (c) Preoperative periapical radiograph of the tooth 14. |
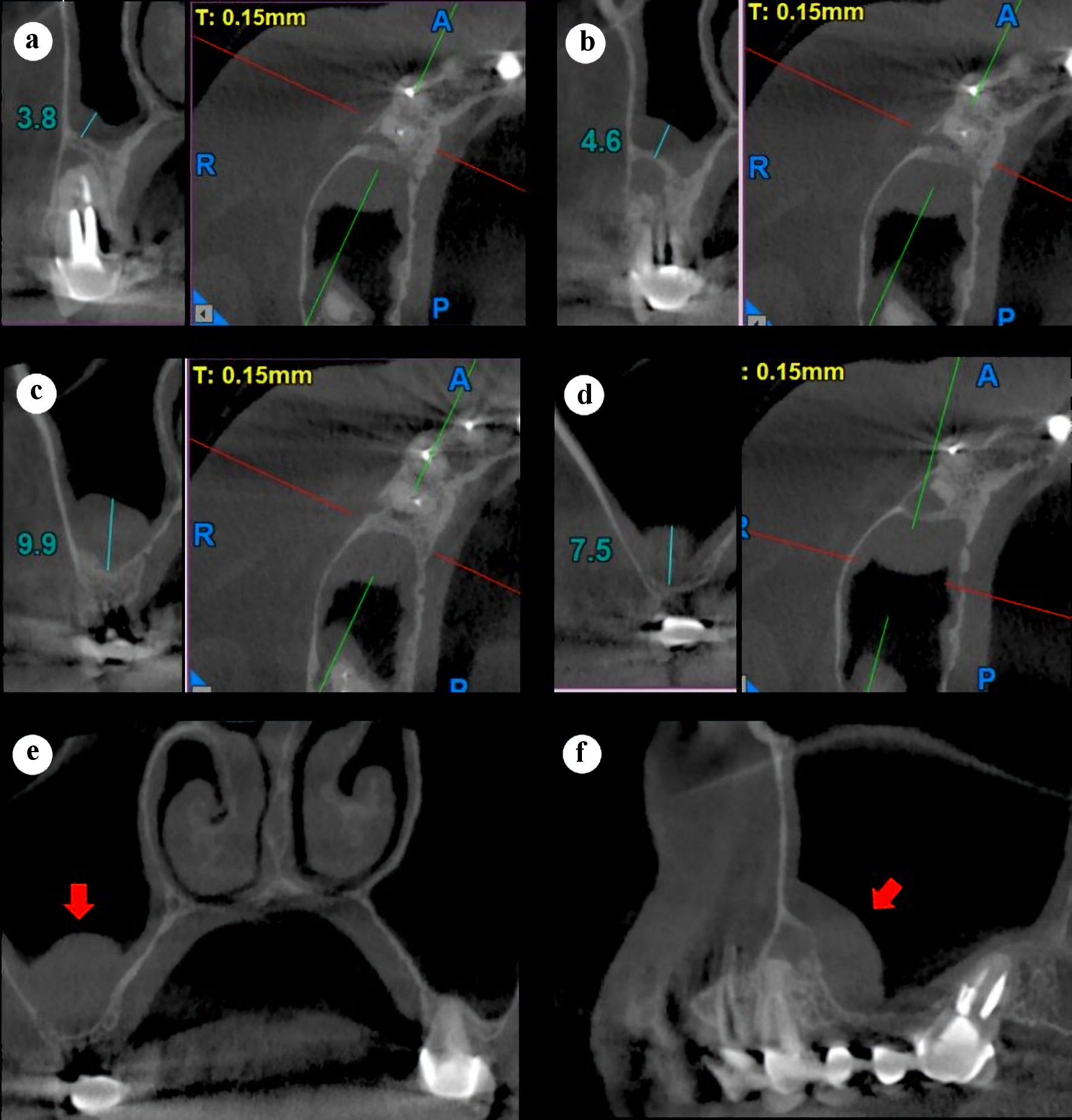 Click for large image | Figure 2. Preoperative right maxillary CBCT scan, sagittal and axial slices (a-d). (a) Center, tooth 14. (b) Distal, tooth 14. (c) 3 mm distal to the tooth 14. (d) Distal of the sinus thickening. (e) Coronal slice showing the thickened sinus membrane (red arrow). (f) Panorex slice showing thickened sinus membrane (red arrow). CBCT: cone-beam computed tomography. |
Treatment
An endodontic microsurgery in the tooth 14 was performed, based on the following rationale: 1) The accurate fixed prosthesis adaptation and the impossibility of disassembling the five-piece-metal-ceramic bridge to perform a new endodontic treatment and the prosthetic restoration; 2) The strict compliance of the mandatory lockdown quarantine measures which forced to limit to the minimum the number of the scheduled visits.
The microsurgery approach advocated by Kim et al [4] was performed, by using the operative microscope magnification, ultrasonic tips and bioceramic materials. The next clinical sequence was followed: 1) Anesthesia: served to prevent pain during surgical procedures and to achieve localized hemostasis; 2) Flap design: full-thickness vertical and horizontal incisions were performed; 3) Mucoperiostic flap reflection: a full mucoperiosteal flap was reflected by means of microinstruments; 4) Ostectomy: to reach the lesion and the root apex, the cortical bone was removed, and the ultrasonic tip B1 was used (W&H Dentalwerk, Burmoos GmbH, Austria) to perform this procedure; 5) Apical resection: to perform the apex exeresis, the ultrasonic tip B6 (W&H Dentalwerk, Burmoos GmbH, Austria) was used perpendicular to the tooth long axis, keeping a 0-degree bevel; 6) Debridement of the pathologic tissue and curettage of the adjacent bone: the diseased material removed was sent for histopathological examination to the Department of Pathological Anatomy (School of Dentistry of the University of Buenos Aires) proving to be an inflammatory cyst; 7) Localized hemostasis: it was performed with the aim of minimizing the surgical time, the intraoperative bleeding and the postoperative swelling. According to the Department of Endodontics of School of Dentistry of the University of Buenos Aires protocol, bismuth subgallate was used to achieve the adequate hemostasis (compounding preparation, Pharmacy REX, CABA, Argentina). The tooth presented two root canals, and the palatal canal had been negotiated but not the buccal canal. It was concluded that this was the cause of the endodontic failure (Fig. 3a); 8) Ultrasonic root-end preparation: the ultrasonic tip R3D (W&H Dentalwerk, Burmoos GmbH, Austria) with 3 mm of active area, specifically designed for this maneuver, was used. The buccal root canal was negotiated, and the removal of the filling material as well as the root-end preparation of the palatal root canal was done. The confluence of both canals was observed (Fig. 3b); 9) Root-end filling material: Bio-C Sealer (Angelus, Londrina, PR, Brazil) was applied in the most coronal portion of the cavity (2 mm) and immediately over it, the actual apical sealing (1 mm) with Bio-C Repair (Angelus, Londrina, PR, Brazil) was performed (Fig. 3c); 10) Cleaning of the surgical site: the visual and radiographic inspection of the area was done. To ensure the removal of any remaining biomaterial or hemostatic substance, the site of the osteotomy was flushed with saline; 11) Flap repositioning and suturing: collagen material Foundation® (Morita, Irvine, CA, USA) was placed as bone substitute and absorbable membrane, acting as a physical barrier to prevent the connective tissue invagination inward the bone defect, and suture was performed with monofilament nylon 6-0 (Ethicon, Johnson & Johnson Medical Devices & Diagnostics Group, Somerville, NJ, USA); 12) Following the surgical procedure, a postoperative radiograph was taken (Fig. 3d).
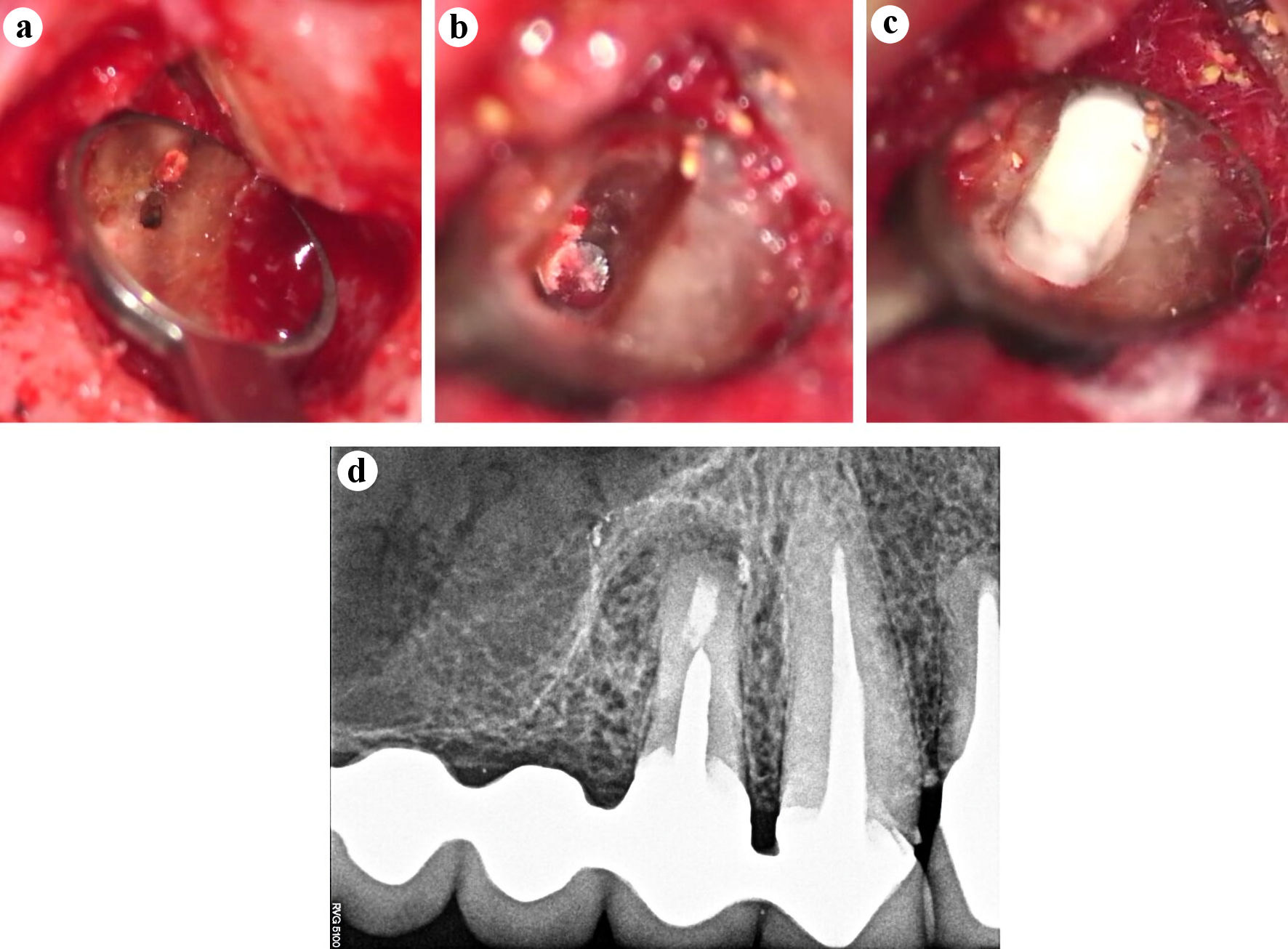 Click for large image | Figure 3. Intra-surgical images documented with operative microscope (Zeiss Extaro 300, Carl Zeiss, Oberkochen, Germany) (a-c). (a) Absence of buccal root canal preparation and filling (× 16). (b) The apical portion of the metal post at the bottom of the ultrasonic root-end preparation is seen (× 25). (c) Apical seal with Bio-C Repair (Angelus, Londrina, PR, Brazil) (× 25). (d) Postoperative periapical radiograph. |
Postoperative care instructions for this type of surgery were provided, including flushing of the area with 0.12% chlorhexidine twice a day for 7 days, and the administration of 600 mg ibuprofen for 72 h.
Follow-up and outcomes
The clinical course was checked by a video conferencing call and the patient was scheduled 10 days later for suture removal and clinical follow-up. During this appointment, the patient reported not to have pain nor postoperative edema. Twelve months later, another follow-up was performed, and a CBCT scan was taken. A normal thickness sinus membrane and a regenerating cortical bone was observed (Fig. 4).
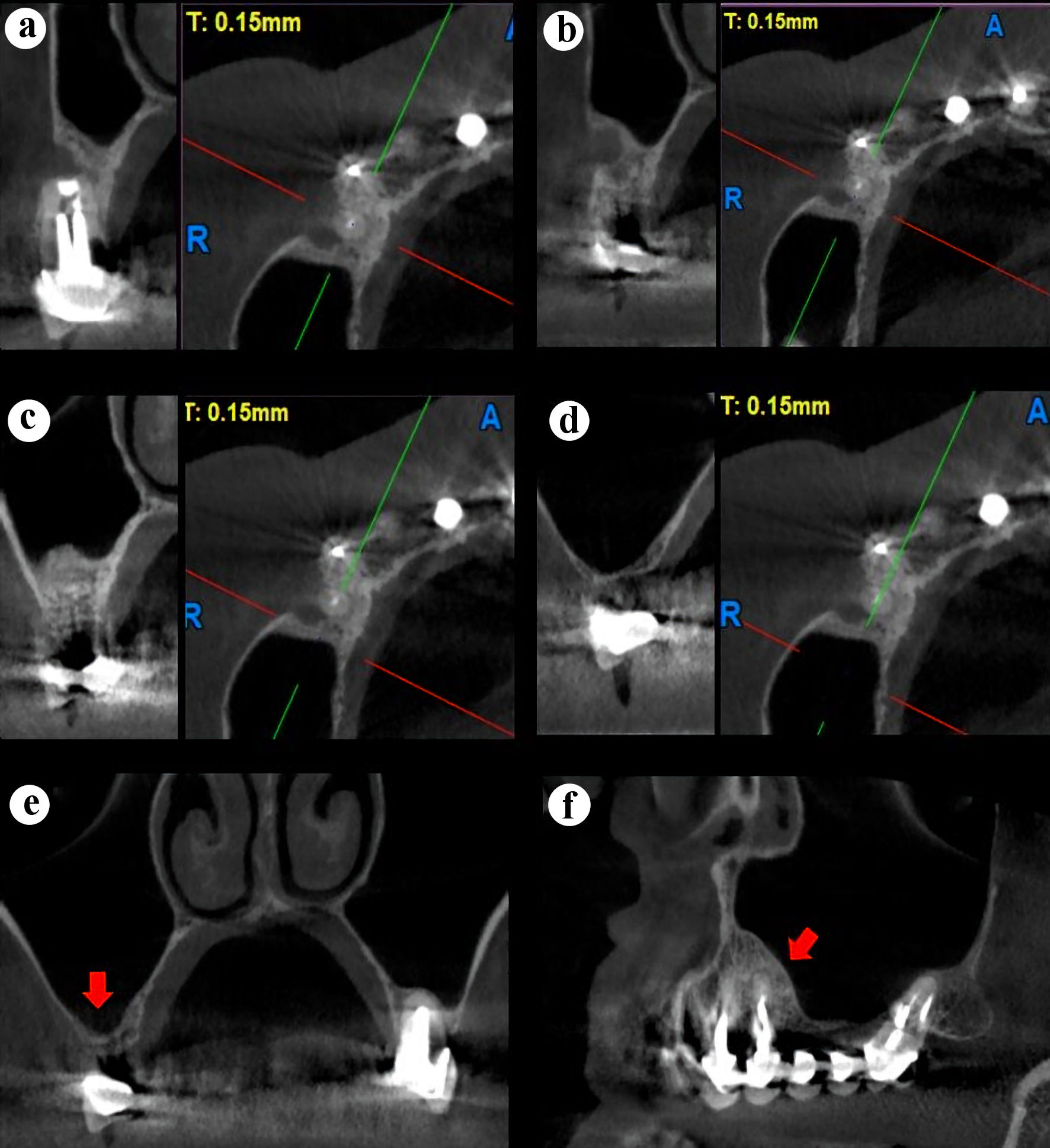 Click for large image | Figure 4. Right maxillary CBCT scan, sagittal and axial slices (a-d). (a) Center, tooth 14. (b) Distal, tooth 14. (c) 3 mm distal to the tooth 14. (d) Total healing of the sinus membrane. (e) Coronal slice showing a normal sinus membrane (red arrow). (f) Panorex slice showing a normal sinus membrane (red arrow). CBCT: cone-beam computed tomography. |
| Discussion | ▴Top |
The association of the maxillary premolars and molars with the maxillary sinus is widely reported in the literature, displaying different types of relationship. The Schneiderian membrane is a mucous membrane, which lines the maxillary sinus periosteum. In proper health, this membrane of approximately 1 mm thick should not be visualized in the periapical radiograph nor in the CBCT scans. A sinus mucosal thickening of more than 2 mm in depth should be considered to be a pathologic condition [11]. This close and varying relationship between the teeth apices and the maxillary sinus fosters the spreading of the odontogenic infections towards the maxillary sinus, favoring, in specific scenarios, odontogenic sinusitis [12]. According to a report carried out at the University of Buenos Aires School of Dentistry, in which 179 CBCTs were analyzed, the main causes of the sinus membrane thickening related to an odontogenic pathosis were dental caries and endodontic treatment [13].
The appropriate diagnosis of the odontogenic sinus conditions depends on the type of radiologic assessment and of the evaluator’s ability when establishing the diagnosis [14, 15], which, ideally, should be achieved in the first appointment, since this fact is essential for the successful treatment outcome. In this case report, a clinical-radiological assessment of the tooth 14 was done. An accurate adaptation of the crown was observed, and when the preoperative periapical radiograph was analyzed, an associated sinus pathosis was suspected. With the aim of guiding the ensuing treatment, a large field of view (FOV), with the sinus-nasal osteum visible, CBCT scan was ordered. CBCT scan is a noninvasive imaging study which enables the exhaustive assessment of the internal and external anatomy of the teeth and the adjacent structures, such as the maxillary sinus [16, 17]. The CBCT scan was helpful to confirm the diagnosis when a sinus pathosis was suspected and also to measure the relationship of the diseased tooth with the maxillary sinus and the membrane thickening, which aided to establish an accurate treatment. In the medium-term follow-up, the cone-beam scan has shown sinus recovery and the periradicular tissues suitable healing.
Regarding the election of an accurate technique, when a non-surgical retreatment is unfeasible or does not improve the current clinical status, the endodontic microsurgery would be indicated for teeth with specific clinical characteristics, as those described in the case report. This type of microsurgery combines the use of magnification and illumination, microinstruments and biomaterials, resulting in a high precision technique [4], with an up to 95.2% survival rate [18].
Conclusions
An accurate diagnosis enables a correct treatment planning in such challenging cases. The precision of the surgical technique execution is of outmost importance in order to allow a positive health outcome in the follow-up.
Learning points
The proposed endodontic microsurgery has enabled the maintenance of the existing prosthetic rehabilitation of the tooth that caused the sinus pathosis and the approach for the resolution required a single treatment appointment. The clinical and tomographic medium-term outcomes were more than acceptable because not only the patient became asymptomatic, but also the sinus membrane tomographic image turned out to be consistent with absence of pathosis, and a cortical bone healing process was observed.
Acknowledgments
None to declare.
Financial Disclosure
The authors declare no financial support or funding for study.
Conflict of Interest
The authors declare no conflict of interest.
Informed Consent
Patient’s informed consent for publication of this report was obtained.
Author Contributions
Conceptualization: Rodriguez PA. Data curation: Consoli Lizzi EP, Chaintiou Piorno R. Formal analysis: Rodriguez PA. Investigation: Consoli Lizzi EP, Chaintiou Piorno R. Methodology: Consoli Lizzi EP. Project administration: Chaintiou Piorno R. Resources: Rodriguez PA. Software: Rodriguez PA. Supervision: Rodriguez PA. Validation: Consoli Lizzi EP. Visualization: Chaintiou Piorno R. Writing - original draft: Consoli Lizzi EP, Chaintiou Piorno R. Writing - review and editing: Rodriguez PA.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
Abbreviations
CBCT: cone-beam computed tomography
| References | ▴Top |
- American Association of Endodontists: Guide to clinical endodontics. 6th edition. https://www.aae.org/specialty/clinical-resources/guide-clinical-endodontics/. Accessed September 29, 2021.
- Lui JN, Khin MM, Krishnaswamy G, Chen NN. Prognostic factors relating to the outcome of endodontic microsurgery. J Endod. 2014;40(8):1071-1076.
doi pubmed - Song M, Jung IY, Lee SJ, Lee CY, Kim E. Prognostic factors for clinical outcomes in endodontic microsurgery: a retrospective study. J Endod. 2011;37(7):927-933.
doi pubmed - Kim S, Kratchman S. Modern endodontic surgery concepts and practice: a review. J Endod. 2006;32(7):601-623.
doi pubmed - American Association of Endodontists. Endodontics: Colleagues for excellence. Contemporary endodontic microsurgery: procedural advancements and treatment planning considerations. https://www.aae.org/specialty/wp-content/uploads/sites/2/2017/07/efefall2010final.pdf. Accessed September 29, 2021.
- Johnson BR, Fayad MI. Periradicular surgery. In: Hargreaves KM, Berman LH, eds. Cohen's pathways of the pulp expert consult. 11th ed. St. Louis, MO: Elsevier Health Sciences; 2015. p. 388-389.
- Kim HJ, Yu MK, Lee KW, Min KS. Surgical management of an accessory canal in a maxillary premolar: a case report. Restor Dent Endod. 2019;44(3):e30.
doi pubmed - Hirsch V, Kohli MR, Kim S. Apicoectomy of maxillary anterior teeth through a piezoelectric bony-window osteotomy: two case reports introducing a new technique to preserve cortical bone. Restor Dent Endod. 2016;41(4):310-315.
doi pubmed - Little RE, Long CM, Loehrl TA, Poetker DM. Odontogenic sinusitis: A review of the current literature. Laryngoscope Investig Otolaryngol. 2018;3(2):110-114.
doi pubmed - Gu Y, Sun C, Wu D, Zhu Q, Leng D, Zhou Y. Evaluation of the relationship between maxillary posterior teeth and the maxillary sinus floor using cone-beam computed tomography. BMC Oral Health. 2018;18(1):164.
doi pubmed - Lu Y, Liu Z, Zhang L, Zhou X, Zheng Q, Duan X, Zheng G, et al. Associations between maxillary sinus mucosal thickening and apical periodontitis using cone-beam computed tomography scanning: a retrospective study. J Endod. 2012;38(8):1069-1074.
doi pubmed - Goller-Bulut D, Sekerci AE, Kose E, Sisman Y. Cone beam computed tomographic analysis of maxillary premolars and molars to detect the relationship between periapical and marginal bone loss and mucosal thickness of maxillary sinus. Med Oral Patol Oral Cir Bucal. 2015;20(5):e572-579.
doi pubmed - Branas GV, Grisolia BG, Iuliano RG, Gualtieri A, Lenarduzzi A, Renou SJ, Rodriguez PA. Relation between periapical lesions and sinus membrane thickening assessed by Cone Beam Computed Tomography. Acta Odontol Latinoam. 2018;31(3):164-169.
- Simuntis R, Kubilius R, Padervinskis E, Ryskiene S, Tusas P, Vaitkus S. Clinical efficacy of main radiological diagnostic methods for odontogenic maxillary sinusitis. Eur Arch Otorhinolaryngol. 2017;274(10):3651-3658.
doi pubmed - Shukairy MK, Burmeister C, Ko AB, Craig JR. Recognizing odontogenic sinusitis: A national survey of otolaryngology chief residents. Am J Otolaryngol. 2020;41(6):102635.
doi pubmed - Patel S, Brown J, Pimentel T, Kelly RD, Abella F, Durack C. Cone beam computed tomography in Endodontics - a review of the literature. Int Endod J. 2019;52(8):1138-1152.
doi pubmed - Nair UP, Nair MK. Maxillary sinusitis of odontogenic origin: cone-beam volumetric computerized tomography-aided diagnosis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;110(6):e53-57.
doi pubmed - Huang S, Chen NN, Yu VSH, Lim HA, Lui JN. Long-term success and survival of endodontic microsurgery. J Endod. 2020;46(2):149-157.e144.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


