| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 13, Number 8, August 2022, pages 408-413
Traumatic Humeral Diaphysis Extrusion and Replantation With Periosteal Involvement
Wyatt McGilverya, b, d , Christian Hassona, Montri Daniel Wongworawatc
, Maciej Witkosb
aA.T. Still University College of Osteopathic Medicine, Mesa, AZ, USA
bEmergency Department, Loma Linda University, Loma Linda, CA, USA
cDepartment of Orthopedic Surgery, Loma Linda University, Loma Linda, CA, USA
dCorresponding Author: Wyatt McGilvery, A.T. Still University College of Osteopathic Medicine, Mesa, AZ, USA
Manuscript submitted June 14, 2022, accepted July 27, 2022, published online August 19, 2022
Short title: Humeral Diaphysis Extrusion and Replantation
doi: https://doi.org/10.14740/jmc3975
| Abstract | ▴Top |
Open fractures that produce an extruded long bone diaphysis, such as this case, are an exceedingly rare incident, with even fewer cases documented, leading to difficult medical decision-making for the operative management of such situations. Options for operative management include replantation following sterilization of the extruded fragment, bone transport, a vascularized fibular graft, and even allograft reconstruction. Each option is associated with high and variable levels of risk. The authors report a case study of a 35-year-old female, status post motor vehicle collision (MVC), who sustained a fracture and expulsion of her humeral diaphysis during the incident. She presented to the emergency department by ambulance after colliding into a light post at 50 miles per hour. Upon presentation and examination, the patient scored 14 on the Glascow Coma Scale (GCS) with a positive Focused Assessment with Sonography in Trauma (FAST) exam, consistent with splenic and hepatic injuries. In addition to this, the patient exhibited a flaccid left upper extremity combined with an absent left radial pulse and a small puncture wound on the left anterolateral antecubital area. Radiographic imaging revealed a 6-inch fragment of mid to distal humeral diaphysis missing. Moments later the initial Emergency Medical Services (EMS) crew returned from the scene of the accident with the missing 6-inch fragment of humerus contained in an emesis bag, which was found on the floorboard of the patient’s vehicle. This fragment was preserved at -20 °C for 2 days and later used as an autograft in an open reduction internal fixation surgery. This case highlights and details the techniques for proper storage, treatment, and sterilization of the bone fragment during the period of patient stabilization following trauma, to optimize the replantation and union of the fragment. This includes contrasting the different techniques that could be utilized to preserve and sterilize bony fragments, such as autoclaving, gamma radiation, chemical sterilization with iodine, or deciding whether the fragment needs to be discarded altogether with the utilization of allograft.
Keywords: Extrusion; Replantation; Humerus; Internal fixation; Fracture; Sterilization; Periosteum; Osteogenesis
| Introduction | ▴Top |
A 35-year-old woman who sustained a 6-inch expulsion of her humeral diaphysis following a motor vehicle collision (MVC) received replantation of her bone fragment with successful union, without postoperative infection despite the bone being exposed to the outside elements. This was believed to be possible due to the utilization of depressed temperature preservation, followed by chemical sterilization with 10% povidone-iodine which allowed for the preservation of the periosteum and its osteogenic capabilities.
Replantation, as in this case study, carries a high risk of infection, nonunion, and the need for additional surgeries later. In addition to this, there is the question of the sterilization method utilized for the extruded fragment. There have been reports of successful replantation following both thermal and chemical sterilization. However, the degree and location of intact periosteum may be the deciding factor for the use of replantation, and the method by which the extruded bone fragment is sterilized. From this report, and the review of related literature, it is hypothesized that thermal sterilization via autoclaving may be indicated on bone that has already been stripped of the periosteum, while bone fragments with intact periosteal sheaths may benefit from chemical sterilization such as betadine, as to preserve its osteogenesis capabilities.
| Case Report | ▴Top |
Investigations
A 35-year-old female presented to the emergency department (ED) via Emergency Medical Services (EMS) after being a passenger in a motor vehicle collision. Per the EMS report, the vehicle had impacted a telephone pole at an estimated 45 - 50 miles per hour. At the scene there were 2 - 3 feet of passenger space intrusion, indicating a high-degree mechanism of injury (MOI). The patient was unable to recall if she was wearing her seatbelt or if she had a loss of consciousness. However, the driver of the vehicle was found to be dead on arrival and had been thrown onto the patient during the collision further contributing to the MOI. Following the patient’s extrication from the vehicle, a piece of bone was found on the floorboard of the vehicle that was presumed to be from the patient’s left arm.
Upon arrival to the ED, the patient was oriented to person, place, and time with a Glascow Coma Scale (GCS) of 14. Her head appeared to be normocephalic and atraumatic. However, during the physical exam, the patient was noted to have +2 radial pulses on the right and 0 on the left. The only external pathological finding on the patient’s left upper extremity was a small, 3 cm puncture wound to the left anterolateral antecubital region. This laceration appeared to be oozing in nature, and bleeding was controlled. In addition to this, the patient’s left upper extremity appeared to be flaccid, whereby she was unable to flex, extend, abduct, or adduct at the elbow and shoulder articulations. Suspecting a transverse or comminuted fracture of the left humerus, portable radiography was obtained of the patient’s left upper extremity.
Diagnosis
The radiographs revealed not only a complete transverse fracture of the humerus but there appeared to be complete proximal and distal transverse fractures of the humerus, leading to extrusion of the humeral diaphysis, as displayed by the complete lack of osteo-opacity in the middle of the arm (Fig. 1a).
 Click for large image | Figure 1. (a) The initial radiograph diagnosing the absence of a 6-inch humeral diaphysis. (b) Extruded fragment of bone present in the hands of emergency department personnel immediately following the MVC. |
It was at this time when the pre-hospital EMS crew presented an emesis bag containing a 6-inch diaphyseal bony extrusion that visually matched the patient’s missing bone in structure (Fig. 1b), length, and geometric fragments. This extruded fragment had been found on the floorboard of the patient’s vehicle. The suspected MOI that could have caused such an extrusion was deemed to be due to high impact force placing direct posterior pressure on the patient’s arms being extended straight out in front of her, flexed at the shoulder, when bracing for impact. The force was then transmitted to her humorous in a longitudinal pattern, causing complete transverse fractures at both the proximal and mid-distal ends of the humeral diaphysis. However, the extreme force continued to push back posteriorly, allowing for this now free-floating diaphyseal portion of bone to puncture the anterolateral antecubital space, allowing for complete extrusion of the humeral diaphysis, leaving only a 3-cm puncture wound. Although rare, there has been one other report of a similar accident taking place in 1962, where a man’s femur went through a similar fracture and ejection pattern [1].
In addition to this, the patient exhibited generalized abdominal tenderness accompanied by a positive Focused Assessment with Sonography in Trauma (FAST) exam of the bilateral upper quadrants consistent with splenic and hepatic laceration. Initial measures were taken to ensure hemodynamic stability (two units of O-negative blood transfusions and initiating fluid resuscitation with a level one rapid infuser).
Treatment
The patient was then taken for an emergent exploratory laparotomy, where hepatic laceration packing and splenectomy were performed by the trauma team due to internal bleeding. Two days later, orthopedic surgery was initiated to debride necrotic tissue and replant the patient’s extruded humeral diaphysis. A deltopectoral incision was made, and the anterior approach to the humerus was developed. The brachialis was split, and a separate incision was made at the elbow for olecranon osteotomy. Excisional debridement was performed, with the removal of necrotic and devitalized tissue using scissors and a scalpel. The wound appeared severely mangled with wound depths involving the skin, soft tissue, tendon, muscle, and bone. Some necrotic bone fragments were excised as well. The extruded fragment was found with the periosteum still intact and attached, it was therefore cleaned and washed in 10% povidone-iodine solution. From the time the fragment was found on the floorboard of the vehicle, until the time of reattachment, it was kept in the freezer for 48 h. Multiple 2.0-mm drill holes were made along the shaft, and it was filled with InFuse and demineralized bone matrix (DBX) putty. The transcondylar-intra-articular fracture was addressed through a separate elbow incision. Olecranon osteotomy was performed after pre-drilling, tapping, and selecting the 75 mm by 7.3 mm cannulated screw. The fragments were aligned and there was a sliver of 3-mm thick central trochlea that was a separate fragment. K-wires were placed to obtain preliminary alignment. Finally, medial and lateral Synthes variable angle plating was performed, and fluoroscopic images were taken to confirm alignment (Fig. 2). The patient was placed on Keflex for 7 days and no signs of infection or necrosis were noted.
 Click for large image | Figure 2. Intraoperative fluoroscopic imaging of the patient’s left humerus before autograft replantation of the extruded bone fragment (a) and post-surgical internal fixation of humerus and olecranon (b and c). The images demonstrate the placement of complex internal fixation of the distal humerus and a single fixation screw within the olecranon, with normal articulation intraoperatively. |
Follow-up and outcomes
The patient then followed up in the clinic postoperatively at 2 and 5 months. There was noted mild lateral displacement of the distal humerus at the 2-month follow-up (Fig. 3). However, there was union of the fragmented segments, and an increased periosteal formation is noted with no signs of infection or necrosis. Further healing is noted in the 5-month follow-up radiographs (Fig. 4), where there is progressive osseous bridging. At this point, the patient has full motor control and active range of motion in the left glenohumeral and elbow joints.
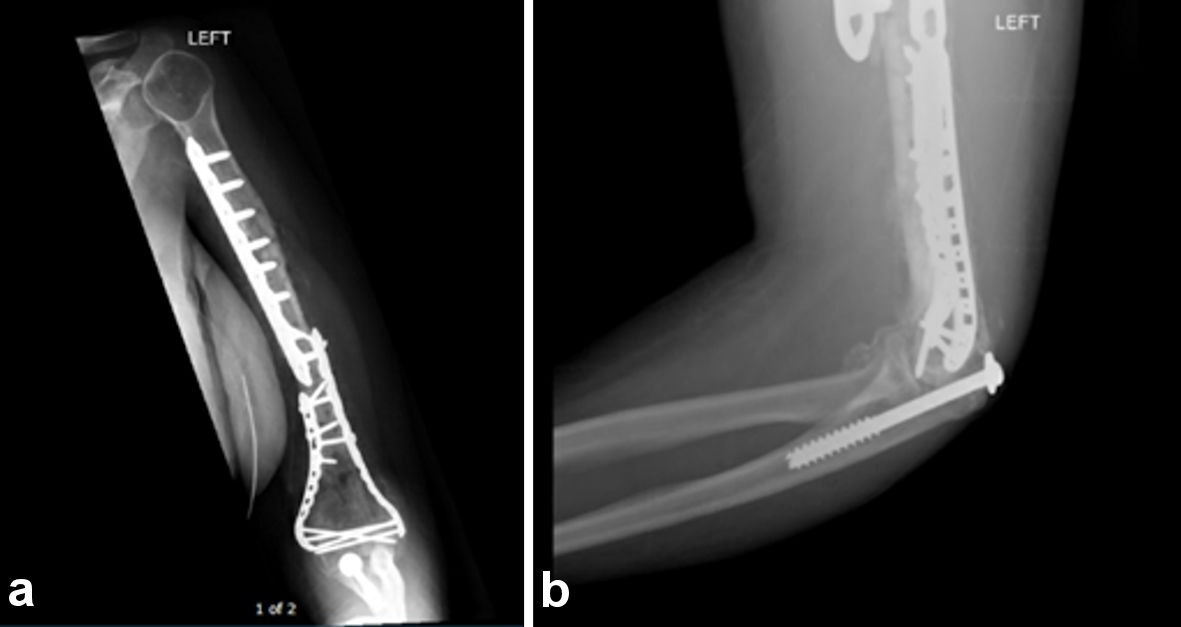 Click for large image | Figure 3. Two-month postoperative radiographs of the left humerus (a) and left lateral olecranon fixation (b). There is demonstration of the extensive plate and screw fixation of the full length of humerus traversing the extensive comminuted mid to distal left humeral fracture with mild lateral displacement of the primary distal fracture fragment. There is also partial visualization of screw fixation of the proximal ulnar fracture. Periosteal reaction and bridging bone formation are seen at the fracture sites. |
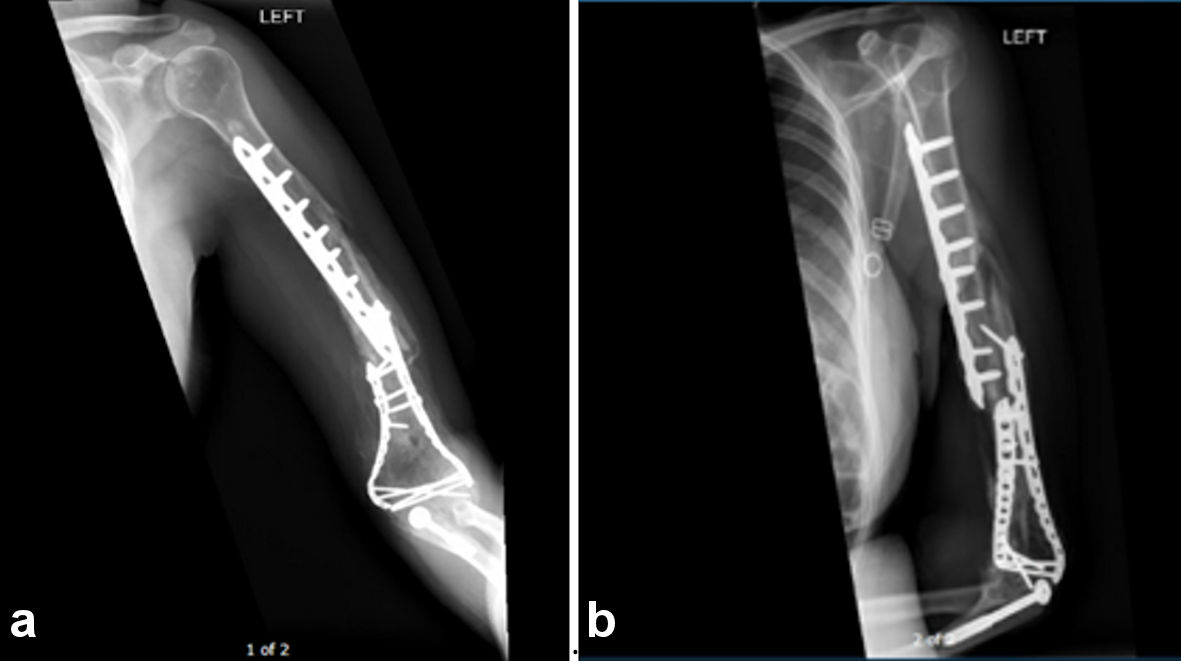 Click for large image | Figure 4. Five-month postoperative radiographs of an anterior/posterior view (a) and lateral view (b). The patient’s follow-up imaging at 5 months postoperative demonstrated intact internal fixation hardware of a segmented left mid and distal humeral diaphyseal fracture, with a mild interval increase in apex lateral angulation at the distal humeral diaphyseal fracture site but with progressive osseous bridging when compared to previous radiographs. |
| Discussion | ▴Top |
Replantation of an extruded bone, status post a high energy impact collision is a precarious procedure. The sterilization and disinfection techniques mentioned in previous literature [2-5] highlight the drawbacks including a high risk of infection, the potential adverse effects on the biological and mechanical properties of the bone and the implications regarding the possibility of bone fragment nonunion. Autoclaving (121 °C, for 20 min at 1.3 bars) before surgery has been shown to be an effective sterilization method [6]. In addition to this, current sterilization procedures via gamma radiation are effective in terms of sterilization alone. However, this process causes damage to the polypeptides of collagen, induces cross-linking, and releases free radicals. Despite reduced bone integrity, this sterilization process is necessary due to high risk of infection and disease transmission [3].
The reintroduction of extruded bone fragmentation has been successful in the past, as documented in 1962 [1] and again in 2006 [6] with large femur fragments. While there are many risks associated with the replantation of an extruded bone, there is a lower rate of complication regarding union, weight-bearing, and delayed hypertrophy [7] compared to other methods of bone grafting.
There are instances where replantation of an extruded cortical fragment carries greater risk than benefit. Both of which weigh heavily on the decision to attempt a replantation. Documented in a case report of two 20-year-old males involved in an MVC, where one of which had a femoral cortical fragment ejected from the lateral thigh entering the passenger’s tibia, we see this difficult decision being made. Rather than risk infection, disease transmission, or nonunion through a replantation surgery, it was decided to proceed using a rod and series of nails to replace the missing cortical fragment. This presents another dimension to the decision-making process of such a rare occurrence. Given the location of this cortical fragmentation, being a non-articular surface, the safest route was to discard the fragment and use sterile hardware to reconstruct the femur and reduce risk [4].
In the previously discussed case of bone extrusion, the fragment remained mostly intact. In other instances, such as a gunshot wound, or other traumatic causes of diffuse fragmentation, the fragmentation is far too numerous to replant. In such cases, allograft along with a series of nailing can provide an alternative method with a relatively fast weight-bearing ability provided by the allograft and healing bone. Despite the absence of any neurologic or vascular injury, the healing process took 13 months [1]. Allograft is a preferred method in situations with large quantities of fragmentation, in large part due to the ability to bare load rapidly (which is necessary for the formation of the bony callus and thus proper union) as well as the reduction of this for nonunion between those fragments [4].
The difficult decision for physicians to make is to allograft or replant the extruded bone fragment. With very few reported incidences, and even fewer literature case studies involving replantation, and autograft via the patient’s bone that had been traumatically extruded, there is a lack of guidelines and uniform compliance among the medical community when it comes to managing these patients. Accidental amputations provide us with knowledge of similar instances and are much more common at nearly 30,000 instances annually. These cases provide us with the important indicators of a potentially successful replantation.
However, there have been a few published case studies involving replantation of extruded bone segments, in particular, long bone diaphysis of femurs and the humerus. One of the earliest cases was reported in 1962 by Kirkup [1], in which a 20-year-old male struck a vehicle while riding his motorcycle, causing an obvious femoral deformity and a 4-inch transverse laceration over the patella as the only epithelial injury. Due to the time era of this accident, radiographic images were not of sufficient quality. Consequently, the 10-inch missing fragment of the femur initially went without detection. Due to the delay in finding the absent femoral diaphysis on imaging, there was an increase in delay in finding the patient’s femur at the scene of the accident. Eventually, the patient’s femoral extrusion was found by a police canine (K9) in a bush near the accident, over 24 h later. This extruded fragment was cleaned, boiled, and then cultured for bacteria, which proved to be aseptic. Twelve days later, the femoral extrusion was autoclaved and replanted in the patient. The autoclave was used rather than betadine because the periosteum, in this case, was not attached to the bone such as in the previously discussed case. The patient was successfully placed on a 10-day course of unknown antibiotics. Two years post operation, the patient had returned to work, and walked with a “barely noticeable limp [1]”.
Forty-four years later a very similar incident occurred and is outlined in a case study by Rouvillain et al [6]. Similar to the previous case [1], a 17-year-old patient suffered from a motorcycle collision where an 11-cm femoral fragment was extruded through a 5-cm lateral wound at the suprapatellar level. Although this femoral extrusion was brought into the emergency department with the patient, the replantation surgery did not occur until 20 days later. This interim period was likely used to stabilize the patient, assess, and repair soft tissue damage, and prepare the implantation site. Prior to bone replantation, patient health, stability, and bone and wound sterilization are evaluated [6]. On the day of operation, the fragment was autoclaved at 121 °C, for 20 min at 1.3 bars. The patient was administered 10 days of an undocumented postoperative antibiotic and had no issues with infection. Similarly, at the 2-year follow-up there was complete healing of the two fracture lines, and the individual was able to re-engage in sports activities.
These two cases are strikingly similar regarding many aspects that likely played a role in the beneficial outcomes. Both cases involved young males, whose capability for healing and recovery is exceptional compared to their elder counterparts. In addition to this, both cases autoclaved the fragment prior to replantation for infection prevention. However, the most striking similarity was both authors described their patient as having an intact periosteal sheath and vasculature where the femoral fragment used to reside, despite the severe trauma. Rouvillian et al described the extruded fragment as having “no soft tissue left on the bone fragment, more specifically no periosteum” [6]. Kirkup explained in 1962 that “Given a periosteum tube, loss of bone does not necessarily infer non-union, and healthy periosteum will replace bone throughout its length in the same ways scars heal, irrespective of their length” [1]. Having an intact periosteal sheath means proper vascularization to the replanted bone which allows sufficient nutrient supply and decreased risk of infection. The main risk during replantation is an infection that would cause further necrosis and likely lead to amputation. Having the periosteal sheath intact provides a positive indicator for the replantation to take and return to normal function after sufficient healing time [8]. Both authors then went on to state another large reason for the replantation of bone was due to this approach allowing for early mobilization to further promote the healing process.
Both claims have been supported by more recent research regarding periosteum stem cells for regenerative medicine [9]. Authors Ferretti and Belmonte demonstrate that periosteum provides a niche for pluripotent cells and a source for molecular factors that modulate cell behavior. In addition, they state the increased ability of periosteal cells to migrate and expand to and across injury sites, ultimately leading to a stronger and faster healing process due to the periosteal influence and contribution to constructing the extracellular matrix (ECM) organization in addition to osteoblastic activity from the pluripotent cells. Ferretti and Belmonte conclude “Periosteum plays a key role in ECM architecture and cell cytoskeletal reorganization under mechanical stress, by the activation of the mechanosensing signaling. Its expression is upregulated in the presence of mechanical stress to preserve bone tissue integrity and function. It also ensures a correct collagen fibrillogenic and matrix organization, opening intriguing perspectives in designing future strategies for bone tissue regeneration” [9].
While these two cases provide examples of successful replantation of a femur segment, there are significant differences between the replantation of a femur and that of a humerus. As we see with the extruded humerus, the increased risk is associated with more damage to surrounding soft tissues. In most cases, there is less soft tissue in an arm than a leg, therefore providing less protection from trauma-related injuries, leaving a humerus more susceptible to post-surgical complications. The results are higher levels of nerve damage, specifically the ulnar nerve, as well as damage to surrounding vasculature, making it difficult to heal and clear infection. To treat this, some procedures may require fibular grafts which are complex but have shown to increase healing and decrease infection [10].
Table 1 summarizes all the three cases we mentioned above [1, 4, 6].
 Click to view | Table 1. Summary of the Three Cases |
Conclusions
Replantation of a traumatically extruded bone is rarely reported in current literature. Many factors need to be considered when deciding the method of repair to utilize. This includes, but is not limited to, the extent of fragmentation and presence of intact periosteum, hemodynamic stability of the patient, degree of contamination of the fragment, and even the anatomical location from which the fragment originated. As highlighted in this case, it was believed that the best outcome for this patient was to utilize preservation of the fragment at -20 °C until utilization, followed by a 10% povidone-iodine wash prior to replantation in order to preserve the osteogenesis capabilities of the intact periosteum.
Learning points
While the presence of complete diaphyseal bone extrusion and replantation is minimal in the English literature, there have been a few rare cases that highlight some of the key important features that might serve as the beginning basis of guidelines that could be implemented in practice. The rarity of bone extrusion prompts a niche for research involving sterilization and replantation techniques and guidelines arising from the few reported cases existing today between the femur cases that supported this case study as well as the case study itself, which seems to be novel in the literature regarding humoral extrusion and replantation. However, it seems evident that the periosteum plays a major role in the reconstruction of bone, and the rigidity/proper healing coordinated by the ECM it provides. The patient in this case report did not have an intact periosteum sheath with a blood supply in the injured arm. Instead, the periosteum remained on the extruded fragment of bone. Circumstantially, a decision was made to clean the fragmented bone with betadine rather than to be autoclaved, to preserve the periosteum for growth and healing post operative. In addition to this, we have seen that replantation allows for early mobilization, and replantation may be performed many hours or even days following the traumatic accident.
Acknowledgments
None to declare.
Financial Disclosure
No funding was provided for this study.
Conflict of Interest
None to declare.
Informed Consent
Signed consent from the patient allowing us to use medical records/information/pictures/images for research/publication and teaching purposes was obtained. Ultimately an IRB review process was completed, and permission was signed and granted through Loma Linda University IRB for the writing of this case study, including all pertinent patient information, pictures, imaging, labs, etc. (without any patient identifiers of course).
Author Contributions
Wyatt McGilvery wrote manuscript, contributed to the literature review, and patient chart review. Christian Hasson contributed to manuscript writing, the literature review, and study design/layout. Maciej Witkos provided oversight to emergency department management of the patient, proofread, and made edits to the manuscript. Montri Daniel Wongworawat provided oversight to orthopedic surgery intervention and management of the patient, proofread, and made edits to the manuscript.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
Abbreviations
FAST: Focused Assessment with Sonography in Trauma; EMS: Emergency Medical Services; ED: emergency department; MOI: mechanism of injury; GCS: Glascow Coma Scale; MVC: motor vehicle collision; DBX: demineralized bone matrix; K9: canine; ECM: extracellular matrix
| References | ▴Top |
- Kirkup JR. Traumatic femoral bone loss. J Bone Joint Surg Br. 1965;47:106-110.
doi pubmed - Goldstein SA. Tissue engineering solutions for traumatic bone loss. J Am Acad Orthop Surg. 2006;14(10 Spec No.):S152-S156.
doi pubmed - Nguyen H, Morgan DA, Forwood MR. Sterilization of allograft bone: effects of gamma irradiation on allograft biology and biomechanics. Cell Tissue Bank. 2007;8(2):93-105.
doi pubmed - Rossman SR, Shaath MK, Graf KW. Head-on allograft transplantation: a unique case report where a large piece of femoral bone was extruded from one patient's body and impaled another patient's Tibia. J Orthop Case Rep. 2017;7(5):50-53.
- Shanmuganathan R, Chandra Mohan AK, Agraharam D, Perumal R, Jayaramaraju D, Kulkarni S. Successful reimplantation of extruded long bone segments in open fractures of lower limb—a report of 3 cases. Injury. 2015;46(7):1389-1392.
doi pubmed - Rouvillain JL, Navarre T, Noseda O, Garron E. Traumatic femoral bone defect reconstruction with an autoclaved autologous femoral segment. A 10-year follow-up. Acta Orthop Belg. 2006;72(2):229-233.
- Wood MB. Upper extremity reconstruction by vascularized bone transfers: results and complications. J Hand Surg Am. 1987;12(3):422-427.
doi - Han KJ, Chung NS, Lee HS, Lee YS. Reimplantation of an extruded humeral segment into an intact periosteal envelope in a child: a case report. JBJS Case Connect. 2012;2(3):e48.
doi pubmed - Ferretti C, Mattioli-Belmonte M. Periosteum derived stem cells for regenerative medicine proposals: Boosting current knowledge. World J Stem Cells. 2014;6(3):266-277.
doi pubmed - Hasan SA, Alla S, Yuen JC. Traumatic extrusion of 13-cm segment of humerus and complete transection of ulnar nerve treated with vascularized fibular graft and acute nerve repair: case report. J Shoulder Elbow Surg. 2013;22(11):e17-22.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


