| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 13, Number 4, April 2022, pages 163-167
Unusual Finding of Type 1 and Type 2 Spontaneous Coronary Artery Dissection in a Multiparous Female: A Case Report
Aditya Patela, c, Jenna DaCostaa, Ruhma Alia, c, Paul Bellafiorea, Muhammad Nadeemb, Addi Suleimanb
aDepartment of Internal Medicine, Saint Michael’s Medical Center, Newark, NJ, USA
bDepartment of Cardiology, Saint Michael’s Medical Center, Newark, NJ, USA
cCorresponding Author: Aditya Patel and Ruhma Ali, Department of Internal Medicine, Saint Michael’s Medical Center, Newark, NJ 07102, USAand
Manuscript submitted February 2, 2022, accepted March 3, 2022, published online March 25, 2022
Short title: Types 1 and 2 SCAD in a Multiparous Female
doi: https://doi.org/10.14740/jmc3909
| Abstract | ▴Top |
Spontaneous coronary artery dissection (SCAD) is an uncommon disease which can lead to acute coronary syndrome especially in young females. The risk factors associated with SCAD include connective tissue disorder, atherosclerosis, hormonal disturbances, history of physical and emotional stressors. Based on angiographic assessment SCAD is divided into three types. We present a unique case of multiparous female with concomitant type 1 and type 2 angiographic features of SCAD. The patient was started on medical therapy with close follow-up. This case highlights the importance of physician awareness about the occurrence of this rare cardiac condition in a young female without any significant risk factors.
Keywords: Spontaneous coronary artery dissection; Acute coronary syndrome; Multiparous female; Angiography
| Introduction | ▴Top |
Spontaneous coronary artery dissection (SCAD) is defined as epicardial coronary artery dissection that occurs in a patient without trauma or significant risk factors for atherosclerotic disease. It is frequently seen in young women and diagnosed via angiography. The patient presentation will vary from asymptomatic to acute coronary syndrome (ACS). Patients may also present with arrhythmia or sudden cardiac death. We present a case of a 41-year-old female with chest pain, diagnosed with concurrent type 1 and type 2 SCAD within the left anterior descending (LAD) artery with multiple risk factors.
| Case Report | ▴Top |
Investigations
A 41-year-old female with a past medical history of chronic migraines presented to the emergency department (ED) with the complaint of chest pain and chest tightness for the past 10 h. The pain was 8/10 in intensity, located in the middle of her chest and radiating to the left arm. It was associated with nausea, vomiting and shortness of breath. The pain was aggravated with exertion and relieved with rest. The patient denied any cough, palpitations, epigastric pain, headache, dizziness, and lower extremity swelling. The patient had no previous cardiac history or any history of sudden cardiac death in the family. She had four previous pregnancies. She also reported feeling anxious and overwhelmed after the sudden, unexpected loss of her 45-year-old sister 3 days prior to admission. The patient does not take any medications and has no significant history of alcohol, smoking or illicit drug use. On admission the patient was afebrile with blood pressure of 112/78 mm Hg, heart rate of 67/min and saturating 99% on room air. On cardiac examination, rate and rhythm were regular with no murmurs, rubs and gallop. The rest of the physical examination was unremarkable.
Diagnosis
The initial laboratory values are shown in Table 1. Electrocardiogram (EKG) showed sinus rhythm with normal axis, normal R wave progression and no significant ST-T wave changes. The patient had a negative urine drug screen and thyroid function tests were within normal limits. The D-dimer was elevated. Computed tomography angiogram (CTA) of the chest was negative for pulmonary embolism. High-sensitivity (HS) troponins were elevated, and the patient was started on aspirin, high intensity statin, therapeutic dose of enoxaparin and ticagrelor. The patient continued to have an increase in HS troponins with a peak of 8,844 ng/L. Serial EKGs showed nonspecific T wave abnormalities in the anterior-lateral leads as shown in Figure 1. Echocardiogram showed apical septum and apical lateral hypokinetic function with left ventricular ejection fraction (LVEF) of 55-60%.
 Click to view | Table 1. Laboratory Parameters |
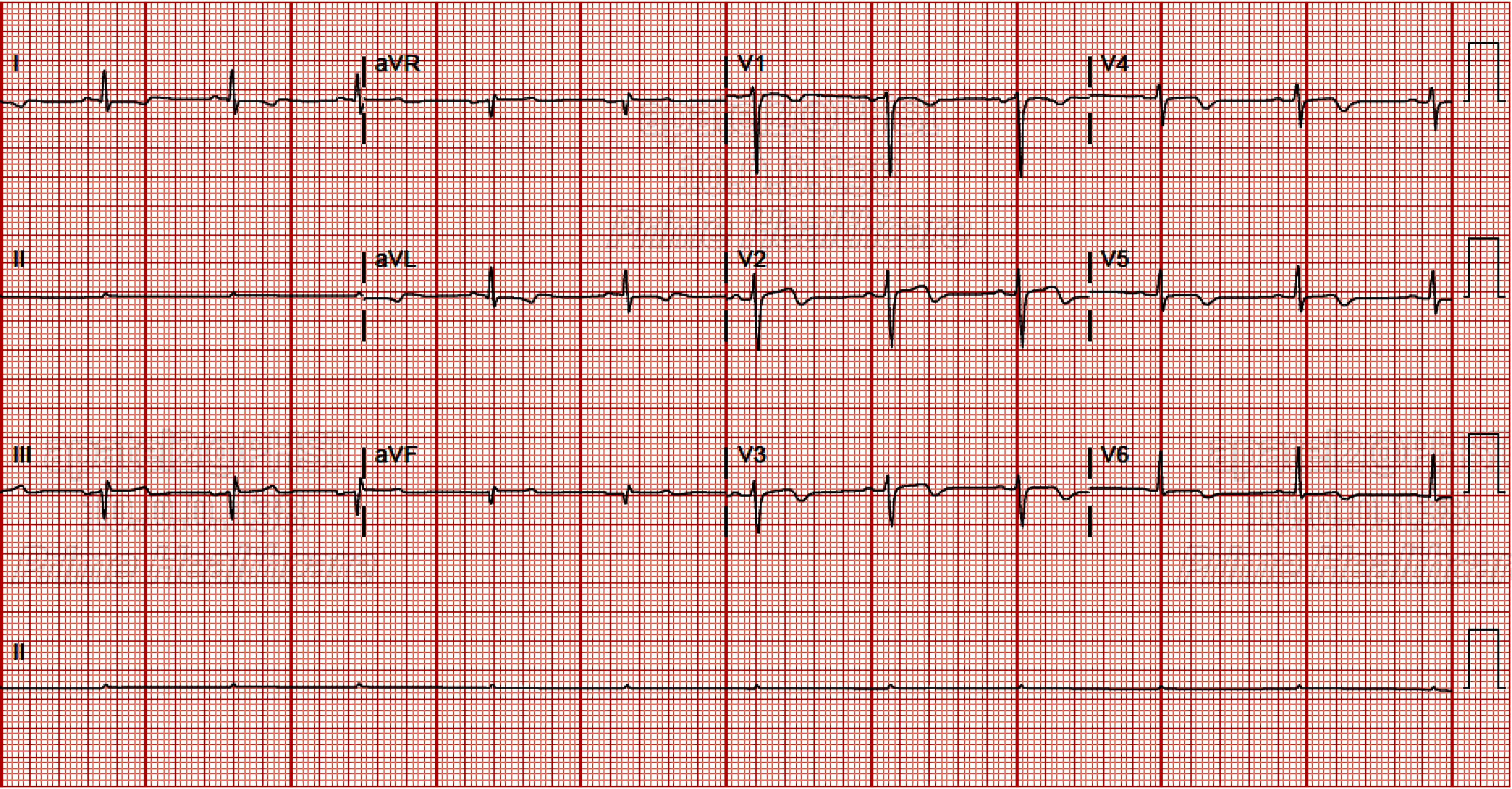 Click for large image | Figure 1. Nonspecific T wave abnormalities in the anterior-lateral leads. |
Treatment
Cardiac catheterization showed a large sized LAD artery with segmental stenosis in the mid-segment secondary to type 2 angiographic SCAD resulting in 70-80% stenosis as shown in Figure 2. In the distal region of the LAD, subtotal occlusion secondary to spontaneous dissection more consistent with type 1 SCAD was observed. No stents were placed during the catheterization. On further questioning, history for fibromuscular dysplasia (FMD) was negative.
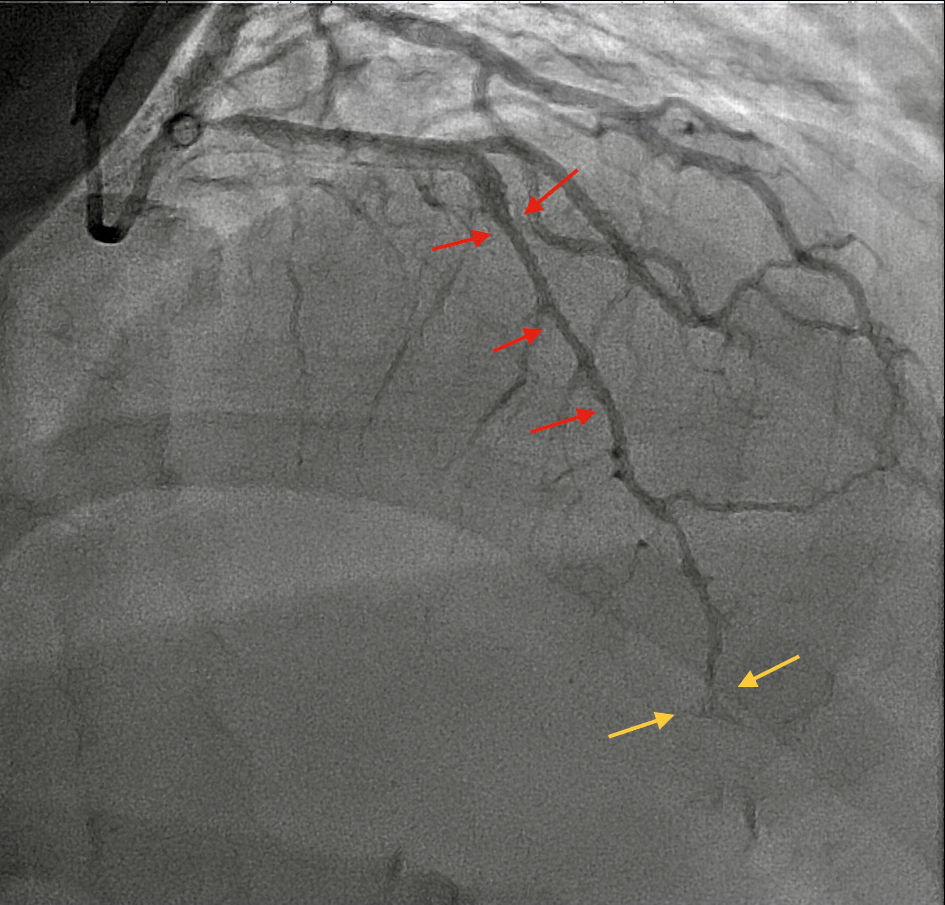 Click for large image | Figure 2. Angiographic finding of type 1 (yellow arrow) and type 2 (red arrow) SCAD in left anterior descending (LAD) artery. SCAD: spontaneous coronary artery dissection. |
Follow-up and outcomes
The patient was discharged home on aspirin, atorvastatin, and a beta-blocker with follow-up in the cardiology clinic. Screening for vascular studies for FMD was recommended as outpatient.
| Discussion | ▴Top |
SCAD is defined as a spontaneous, non-traumatic, non-atherosclerotic and non-iatrogenic separation of the coronary artery wall by intramural hemorrhage [1]. SCAD can manifest with or without an initial intimal tear. There are two proposed mechanisms for the intramural hematoma (IMH) formation in SCAD. The first involves an intimal tear which results in blood collection in the intimal space from the endoluminal space forming false lumen which is termed as “inside-out”. The second mechanism involves rupture of the vasa vasorum resulting in false lumen filled with hematoma which has also been referred to as “outside-in” [1, 2]. Both these mechanisms lead to luminal encroachment and narrowing resulting in subsequent coronary artery obstruction causing myocardial ischemia and infarction.
The overall reported incidence of SCAD is estimated to be between 0.28% to 1.1% based on angiographic assessment [3]; however, they do not consider the notable number of sudden deaths that occur due to spontaneous dissections which might lead to an increase in the actual incidence of SCAD [4]. The increased use of intracoronary imaging for chest pain evaluations have significantly improved our understanding of this distinct pathology. The female to male ratio of this disease is 2:1. Young women without any heart disease account for 70% of the cases with 30% women being in the peripartum period [5]. The prevalence of SCAD in young females without any risk factors for coronary artery disease (CAD) played a major role in the underdiagnosis of this condition in the past. SCAD has been attributed as a significant cause of acute myocardial infarction (MI) [6]. It is estimated that SCAD is the underlying cause of ACS in 1.7-4% of the patient population [7].
Varied etiologies have been associated with SCAD [8] which includes patients with a defective arterial wall due to hereditary connective tissue disorder like Ehler-Danlos syndrome, Marfan syndrome, and FMD. Due to the strong association of SCAD with FMD it is recommended to screen all patients with SCAD for FMD [9]. Patients with underlying atherosclerosis are also at a risk of having SCAD. Peripartum women are also susceptible with highest risk within day 1 to 3 month postpartum. Hormonal disturbance, increased blood flow and stress are thought to have a contributing role in this period [10]. SCAD is also associated with idiopathic risk factors. Other notable associated risk factors include systemic inflammatory disorders, multiparity, oral contraceptives, pregnancy, history of migraine, mechanical and emotional stressors [11]. Mechanical stressors including strenuous exercise have been classically associated with SCAD in males whereas emotional stressors are linked to SCAD in females [2]. A study conducted by Tweet et al reported that the incidence of pregnancy-related SCAD is more in multiparous women [12]. Our patient did not have a family history of CAD. However, she had a history of migraine, was multiparous with four children and recently had a death in the immediate family which was an emotional stressor. The LAD artery is the most frequent site of dissection followed by the left circumflex coronary artery and right coronary artery [13]. In our patient the dissection was in the LAD. The clinical features of SCAD are varied and depend on the limitation of flow of the coronary artery dissection. Chest pain is the most prevalent presenting symptom [14]. Ventricular arrhythmias, cardiogenic shock, and sudden cardiac death account for SCAD presentation in 3-11% of the reported cases [4, 15].
Various imaging modalities have been used in the diagnosis of SCAD. Coronary angiogram, cardiac computed tomography angiography (CCTA), optical coherence tomography (OCT) and intravascular ultrasound (IVUS) can be utilized [16]. Early coronary angiography has been recommended in patients with a high index of suspicion for SCAD. Since coronary angiogram is a two-dimensional imaging technique, the arterial wall is difficult to visualize with this modality. SCAD predominantly affects the arterial wall; and in controversial and complicated cases for the further diagnosis OCT and IVUS should be used. OCT has been superior in visualizing intimal tears, intraluminal thrombi, false lumen, and IMH; however, IVUS is better in visualizing deeper vessels and complete extent of the IMH [1]. Based on the coronary angiogram three variants of SCAD appearance have been classified as per Yip-Saw classification [17]. Type 1 involves multiple lumen and contrast staining of the arterial wall. Type 2 involves stenosis of the arteries with abrupt change in vessel caliber. Type 3 mimics atherosclerosis. Our patient had both type 1 and type 2 angiographic findings which makes our case unique.
Optimal management in SCAD patients has been uncertain. Patients who are clinically stable with no high-risk anatomy can be conservatively treated with beta-blockers, aspirin, and statins. Beta-blockers have been used as a mainstay of treatment as it has shown to have a protective role with lower risk of recurrent SCAD [7]. For patients who have left main or severe proximal two-vessel dissection or active ischemia, coronary artery bypass grafting (CABG) and percutaneous coronary intervention (PCI) have also been considered. But several studies have recommended a strategy of conservative management with prolonged observation in place of PCI, considering high rates of procedure failure and complications [18, 19]. Our patient was medically managed with beta-blockers, aspirin, and statin. Recent studies have also raised the question of generalized coronary fragility in SCAD women patients, considering higher rates of iatrogenic dissection during cardiac catheterization when compared with age-matched women without SCAD [20].
SCAD is an underdiagnosed condition and can result in substantial morbidity and mortality in patients with no traditional cardiovascular risk factors. A high index of suspicion for SCAD is required for appropriate management and prevention. Although physician awareness is increasing regarding this disease mostly through observational and retrospective research, prospective studies are the need of the hour for the development of guideline-directed therapy.
Learning points
SCAD is an underdiagnosed disease which presents as ACS. Physician awareness is required for prompt recognition and diagnosis of this uncommon pathology to reduce the morbidity and mortality associated with this condition. Further large-scale prospective studies are required to develop therapies for SCAD management and prevention.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Informed consent was obtained.
Author Contributions
Aditya Patel MD, Jenna DaCosta DO, Ruhma Ali MD, Paul Bellafiore DO, Muhammad Nadeem MD: diagnosis and management of the patient, discussion, writing and drafting of the case, final approval of the case report. Addi Suleiman MD: management of the patient, revision, and final approval of the case report.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Saw J. Coronary angiogram classification of spontaneous coronary artery dissection. Catheter Cardiovasc Interv. 2014;84(7):1115-1122.
doi pubmed - Ravipati H, Rodrigues S, Rao S, Hatharaliyadda B, Junia C. The young heart tears easily apart: a case report of spontaneous coronary artery dissection. Cureus. 2021;13(6):e15590.
doi pubmed - Kumar T, Prajapati A, Shah MM. Spontaneous coronary artery dissection involving all major arteries LAD, LCX and RCA -A case report. J Family Med Prim Care. 2019;8(11):3739-3741.
doi pubmed - Mokhberi V, Bagheri B, Navidi S, Amini SM. Spontaneous coronary artery dissection: a case report. J Tehran Heart Cent. 2015;10(3):159-162.
- Schmid J, Auer J. Spontaneous coronary artery dissection in a young man - case report. J Cardiothorac Surg. 2011;6:22.
doi pubmed - Mortensen KH, Thuesen L, Kristensen IB, Christiansen EH. Spontaneous coronary artery dissection: a Western Denmark Heart Registry study. Catheter Cardiovasc Interv. 2009;74(5):710-717.
doi pubmed - Saw J, Humphries K, Aymong E, Sedlak T, Prakash R, Starovoytov A, Mancini GBJ. Spontaneous coronary artery dissection: clinical outcomes and risk of recurrence. J Am Coll Cardiol. 2017;70(9):1148-1158.
doi pubmed - Sabatine MS, Jaffer FA, Staats PN, Stone JR. Case records of the Massachusetts General Hospital. Case 28-2010. A 32-year-old woman, 3 weeks post partum, with substernal chest pain. N Engl J Med. 2010;363(12):1164-1173.
doi pubmed - Ya'qoub L, Modi K. Acute de novo multivessel spontaneous coronary artery dissection: a case report and review of literature. JACC Case Rep. 2019;1(1):32-35.
doi pubmed - Butler R, Webster MW, Davies G, Kerr A, Bass N, Armstrong G, Stewart JT, et al. Spontaneous dissection of native coronary arteries. Heart. 2005;91(2):223-224.
doi pubmed - Vijayaraghavan R, Verma S, Gupta N, Saw J. Pregnancy-related spontaneous coronary artery dissection. Circulation. 2014;130(21):1915-1920.
doi pubmed - Tweet MS, Hayes SN, Codsi E, Gulati R, Rose CH, Best PJM. Spontaneous coronary artery dissection associated with pregnancy. J Am Coll Cardiol. 2017;70(4):426-435.
doi pubmed - Zampieri P, Aggio S, Roncon L, Rinuncini M, Canova C, Zanazzi G, Fiorencis R, et al. Follow up after spontaneous coronary artery dissection: a report of five cases. Heart. 1996;75(2):206-209.
doi pubmed - Luong C, Starovoytov A, Heydari M, Sedlak T, Aymong E, Saw J. Clinical presentation of patients with spontaneous coronary artery dissection. Catheter Cardiovasc Interv. 2017;89(7):1149-1154.
doi pubmed - Tweet MS, Hayes SN, Pitta SR, Simari RD, Lerman A, Lennon RJ, Gersh BJ, et al. Clinical features, management, and prognosis of spontaneous coronary artery dissection. Circulation. 2012;126(5):579-588.
doi pubmed - Maehara A, Mintz GS, Castagna MT, Pichard AD, Satler LF, Waksman R, Suddath WO, et al. Intravascular ultrasound assessment of spontaneous coronary artery dissection. Am J Cardiol. 2002;89(4):466-468.
doi - Ghafoor HU, Bose A, El-Meligy A, Hannan J. A case report of recurrent spontaneous coronary artery dissection and Takotsubo cardiomyopathy: a treatment dilemma. Eur Heart J Case Rep. 2020;4(1):1-6.
doi pubmed - Tweet MS, Eleid MF, Best PJ, Lennon RJ, Lerman A, Rihal CS, Holmes DR, Jr., et al. Spontaneous coronary artery dissection: revascularization versus conservative therapy. Circ Cardiovasc Interv. 2014;7(6):777-786.
doi pubmed - Saw J, Aymong E, Sedlak T, Buller CE, Starovoytov A, Ricci D, Robinson S, et al. Spontaneous coronary artery dissection: association with predisposing arteriopathies and precipitating stressors and cardiovascular outcomes. Circ Cardiovasc Interv. 2014;7(5):645-655.
doi pubmed - Fahey JK, Chew A, Ihdayhid AR, Rashid HN, Zaman S, Nicholls SJ, White AJ. Women with spontaneous coronary artery dissection are at increased risk of iatrogenic coronary artery dissection. Heart Lung Circ. 2021;30(1):e23-e28.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


