| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 3, Number 1, February 2012, pages 20-22
Kernohan-Woltman Notch Phenomenon Related to Chronic Subdural Hematoma: A Case Report
Serdal Albayraka, Necati Uclerb, c, Omer Aydena, Hakan Cakinb
aDepartment of Neurosurgery, Elazig Education and Research Hospital, Elazig, Turkiye
bDepartment of Neurosurgery, School of Medicine, Firat University, Elazig, Turkiye
cCorresponding author: Necati Ucler, Department of Neurosurgery, School of Medicine, Firat University, 23200, Elazig, Turkiye
Manuscript accepted for publication November 1, 2011
Short title: Kernohan-Woltman Notch Phenomenon
doi: https://doi.org/10.4021/jmc390w
| Abstract | ▴Top |
Kernohan-Woltman notch phenomenon defines the neurological picture caused by a compressive injury of the cerebral peduncles at the tentorial edge due to the contralateral supratentorial lesion and leads to ipsilateral hemiparesis or hemiplegia and mydriasis. We have represented this case of Kernohan-Woltman notch phenomenon that developed secondary to chronic subdural hematoma in a 88-year-old patient as a very rarely reported case. We conclude that advanced brain atrophy contributes to the formation of Kernohan-Woltman notch phenomenon resulted from chronic subdural hematoma. Additionally, investigation of cerebral peduncles via magnetic resonance imaging is important in determination of the clinical picture and evaluation of the response to the treatment in such cases.
Keywords: Kernohan-Woltman notch phenomenon; Chronic subdural hematoma; Cerebral peduncle; Tentorialedge
| Introduction | ▴Top |
Kernohan-Woltman notch phenomenon (KWNP) is defined as compression of the cerebral peduncle against the tentorial edge caused by the displacement of the brain tissue at the ipsilateral side of the paradoxically supratentorial-localized lesion such that it may lead to hemiparesis or hemiplegia and mydriasis [1]. This phenomenon is usually reported secondary to brain tumours and severe head injuries [2]. The development of KWNP secondary to chronic subdural hematomas has been rarely reported. Although, there are various etiological factors, compression of cerebral peduncles at the tentorial edge is the essential mechanism in development of this phenomenon. We have discussed this case of KWNP secondary to chronic subdural hematoma (CSH) with its clinical and radiological findings in the view of literature.
A 88-year-old male patient, that was operated for right-sided chronic subdural hematoma 3 months ago, has reapplied our clinic with complaints of headache and weakness on his right-side. Glasgow Coma Score was 14 in his neurological examination. The case had dyphasia, mydriasis on his right-pupil and right hemiparesis. Brain Computed Tomography (CT) showed recurrence of right frontoparietal CSH and an evident shift to left side of brain (Fig. 1). When compared with right side of basilar cisterns and cerebral peduncle, Magnetic Resonance Imaging (MRI) revealed an obliteration in the basilar cisterns and a narrowed distance between left cerebral peduncle and tentorial edge at the left side secondary to subdural hematoma (Fig. 2). Additionally, MRI showed no different pathology such as cerebral ischemic attack that may be associated with present neurological picture. For treatment of CSH, burr hole defects of previous operation were widened to remove hematoma and a drain was placed into the subdural distance. The neurological picture of the patient was completely recovered in the early postoperative period.
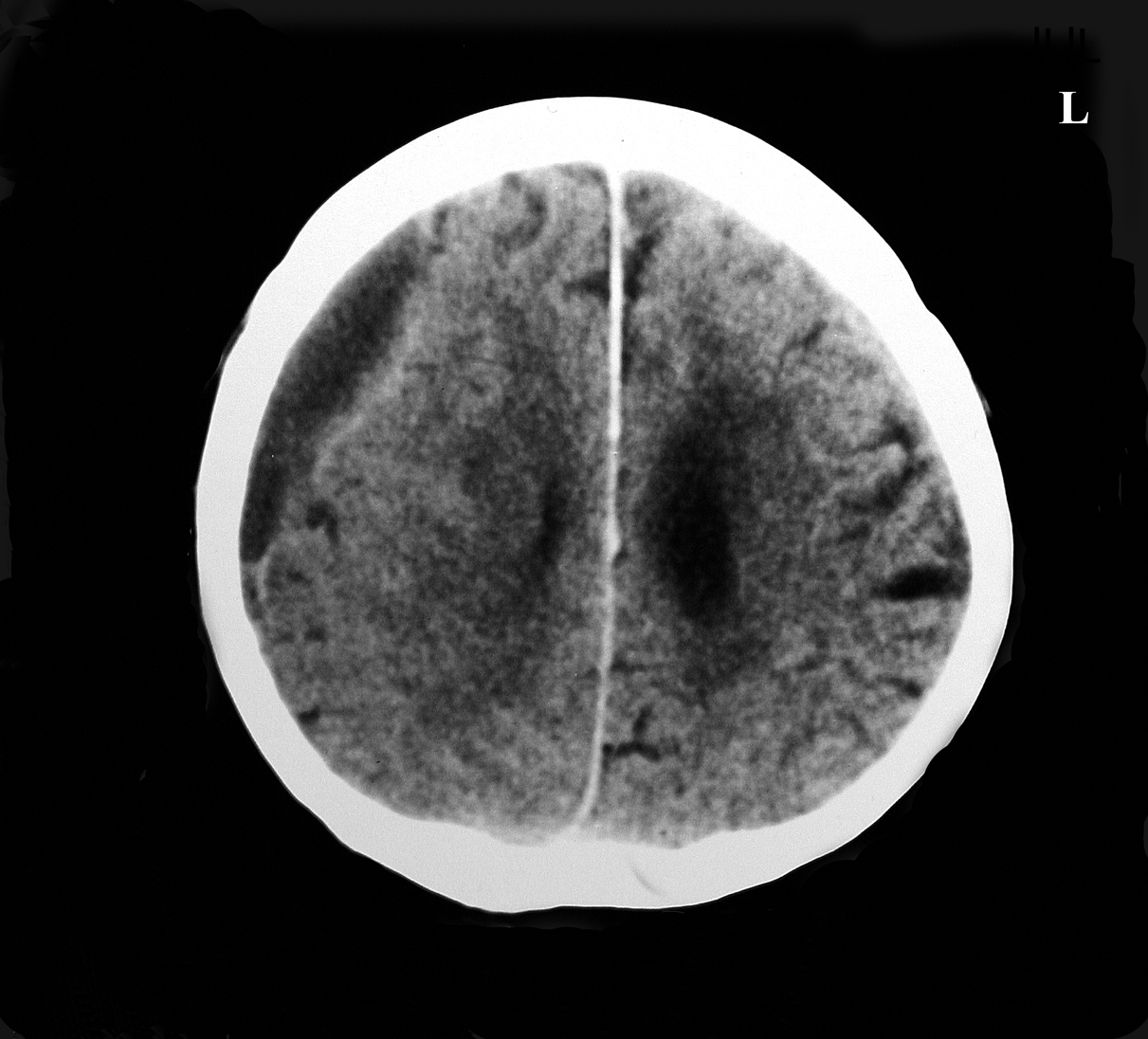 Click for large image | Figure 1. Brain CT showing CSH at right frontoparietal and an evident shift to left side of brain. |
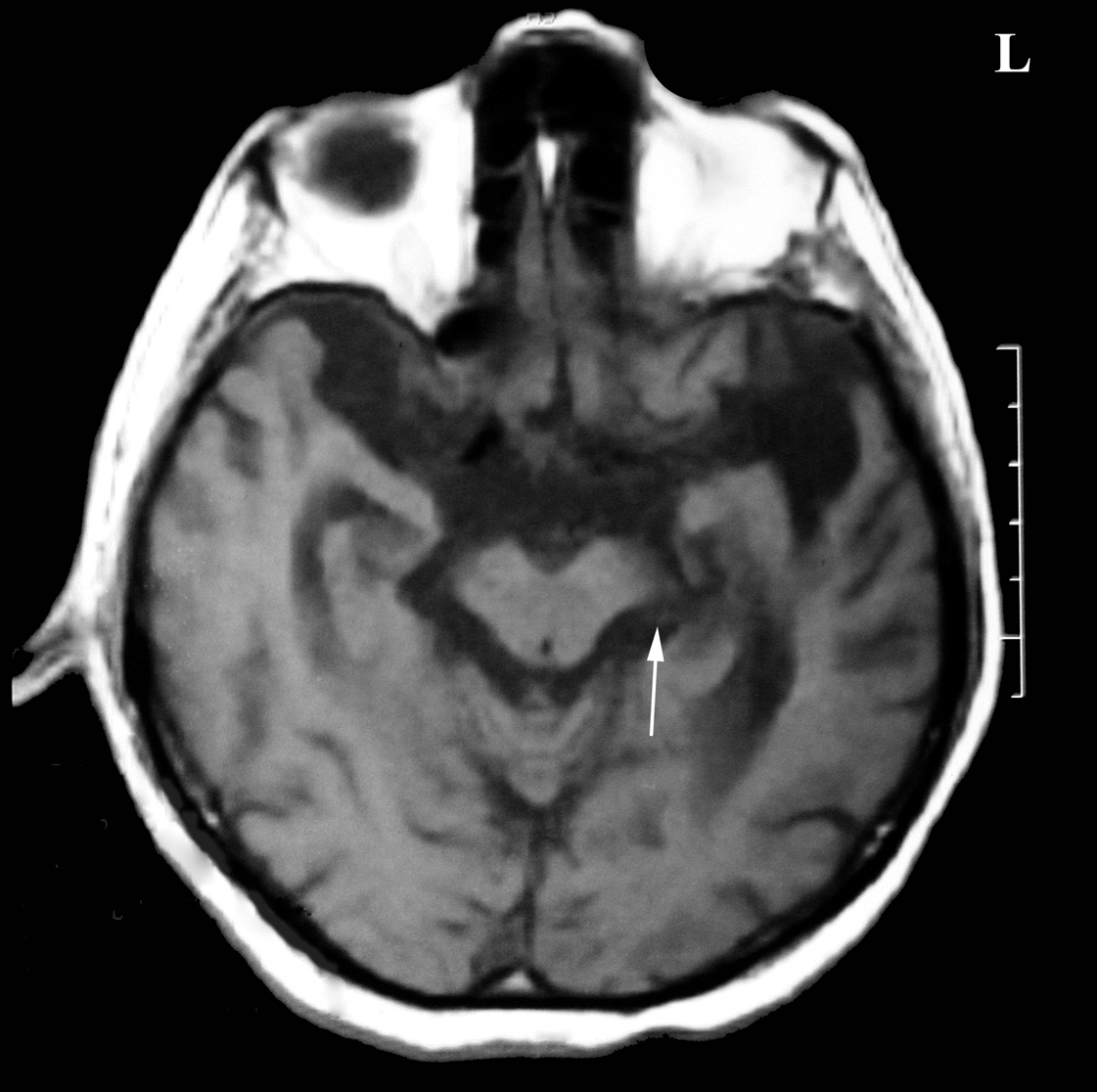 Click for large image | Figure 2. MRI showing compression and a narrowing of the left cerebral peduncle at the tentorial edge when compared with right side. |
| Discussion | ▴Top |
Kernohan and Woltman have described at 1929 that any supratentorial-localized mass may compress the contralateral cerebral peduncles at the tentorial edge [3]. It has been reported that injury of corticospinal motor neurons in the contralateral cerebral peduncles may cause the ipsilateralisation in the course of KWNP [4]. As though, there is no comprehensive clinical trial concerned with the incidence of KWNP, nevertheless, there is limited number of case of KWNP secondary to CSH [4-6].
Chronic subdural hematoma is a frequent situation following head traumas in usually old patients. Traumas easily cause injury of bridging-venous structures of the brain in the old patients because of the decreased volume of brain tissue. A progressive hematoma may develop even following a mild head trauma. The brain atrophy of the old people also causes easier displacements of the central brain structures due to any space-occupying lesion at the supratentorial distance (hematoma, tumour etc). Our case had remarkable brain atrophy depending on his age. The displacement of the mid-line structures was monitored. When the mechanism of Kernohan-Woltman notch phenomenon was considered, we conclude that remarkable brain atrophy of our case was a facilitating factor in development of KWNP secondary to wide subdural hematoma.
The clinical evaluation is the gold standard in diagnosis of Kernohan-Woltman notch phenomenon. Although, presence of lateralization findings and the lesion at the same-side and non-existence of another accompanying pathology that may lead to KWNP are efficient for diagnosis, it is critically important to investigate the signal changes through the cerebral peduncles and compression of basilar cisterns by MRI. Moon et al have reported that there is a correlation between the signal changes through cerebral peduncles and recovery of neurological deficits occurring in the course of KWNP and that cases without any signal change showed a much faster and stronger recovery [4]. Itoyoma et al have evaluated the cerebral peduncles in case with CSH pre- and post-operatively and stated that hemiparesis of the patient recovered secondary to the improvement of the deformity in the cerebral peduncles during the postoperative period [5]. In our case, no signal change was monitored although a compression was encountered in the cistern surrounding the peduncle by MRI. The completely recovery of neurological picture of our case in the early postoperative period supported the reports of Moon et al [4].
Conclusion
CSH may rarely cause KWNP in the cases with advanced age and remarkable brain atrophy. The investigation of cerebral peduncles via preoperative MRI would provide an important contribution in the definition of the neurological deficits and evaluation of the treatment outcomes in such cases.
| References | ▴Top |
- Carrasco R, Pascual JM, Navas M, Martinez-Florez P, Manzanares-Soler R, Sola RG. Kernohan-Woltman notch phenomenon caused by an acute subdural hematoma. J Clin Neurosci. 2009;16(12):1628-1631.
pubmed doi - Kunii N, Morita A, Yoshikawa G, Kirino T. Subdural hematoma associated with dural metastasis—case report. Neurol Med Chir (Tokyo). 2005;45(10):519-522.
pubmed doi - Kernohan JW, Woltman HW. Incisura of the crus due to contralateral brain tumor. Arch Neurol Psychiatry. 1929;21:274–278.
- Moon KS, Lee JK, Joo SP, Kim TS, Jung S, Kim JH, Kim SH, et al. Kernohan's notch phenomenon in chronic subdural hematoma: MRI findings. J Clin Neurosci. 2007;14(10):989-992.
pubmed doi - Itoyama Y, Fujioka S, Ushio Y. Kernohan's notch in chronic subdural hematoma: findings on magnetic resonance imaging. J Neurosurg. 1995;82(4):645-646.
pubmed doi - Yamasaki F, Kodama Y, Hotta T, Yuki K, Taniguchi E, Hashizume A. Magnetic resonance imaging of Kernohan's notch in chronic subdural hematoma. No To Shinkei. 1997;49(6):563-566.
pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


