| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 13, Number 4, April 2022, pages 151-154
A Diagnosis of Choriocarcinoma in a Parturient Presenting With Intracranial Hemorrhage
Deborah A. Romeoa, David A. Gutmanb, d, Joel Siriannic, Michael Marottab
aAnesthesia and Perioperative Medicine, Pediatric Anesthesia, Medical University of South Carolina, Charleston, SC 29425, USA
bAnesthesia and Perioperative Medicine, Obstetric Anesthesia, Medical University of South Carolina, Charleston, SC 29425, USA
cAnesthesia and Perioperative Medicine, Medical University of South Carolina, Charleston, SC 29425, USA
dCorresponding Author: David A. Gutman, Anesthesia and Perioperative Medicine, Obstetric Anesthesia, Medical University of South Carolina, Charleston, SC 29425, USA
Manuscript submitted January 5, 2022, accepted February 16, 2022, published online March 25, 2022
Short title: Choriocarcinoma in a Parturient
doi: https://doi.org/10.14740/jmc3898
| Abstract | ▴Top |
Choriocarcinoma in a viable pregnancy is uncommon. The diagnosis can easily be missed when there is an explanation for the clinical symptoms that the cancer can mimic. We present the case of a primigravid patient whose choriocarcinoma was initially missed as a result of seemingly obvious explanations for her atypical history and disease manifestation. The patient is a Caucasian female at 30 weeks and 5 days of gestation who presented with persistent headaches and new-onset tonic-clonic seizures found on brain magnetic resonance imaging (MRI) to have a left intracranial hematoma, a 5 mm midline shift, and multiple foci of restricted diffusion. Cerebral angiogram demonstrated arteriovenous malformations (AVMs). The fetus was emergently delivered 1 week into hospitalization for non-reassuring fetal heart tracings in the setting of maternal lethargy secondary to continued AVM hemorrhage. The patient’s hospital course was complicated by four episodes of intracranial bleeding and edema requiring neurosurgical intervention. Three weeks after hospitalization she was discharged to a rehabilitation center, shortly after which placental biopsy demonstrated choriocarcinoma. MRI after readmission demonstrated extensive metastatic disease and human chorionic gonadotropin (hCG) levels were greater than 225,000 mIU/mL. Despite two additional neurosurgical procedures and extensive chemotherapy the patient died 3 months after initial presentation. Choriocarcinoma is extremely rare in viable pregnancies, but it should be considered when a parturient presents with intracranial bleeding. A high level of suspicion and serial serum hCG levels may lead to early and potentially life-saving multidrug chemotherapy. With a broader differential, earlier hCG measurement, and earlier treatment, our patient may have survived.
Keywords: Choriocarcinoma; Intracranial hemorrhage; Human chorionic gonadotropin; Gestational trophoblastic disease; Arteriovenous malformation
| Introduction | ▴Top |
Choriocarcinoma is a malignant disorder within the spectrum of gestational trophoblastic diseases that ranges from benign partial and complete hydatiform mole to malignant gestational trophoblastic neoplasia. Choriocarcinomas are highly vascular epithelial tumors that arise from villous trophoblasts and produce human chorionic gonadotropin (hCG). These tumors can occur at any time during or after any type of gestation, with an incidence of 1:50,000 deliveries [1]. Metastasis of the disease is very common with spread outside of the pelvis to the lungs, liver and brain. Pulmonary metastasis is most prevalent. Diagnosis is made by measuring elevated hCG values and pelvic ultrasound to ascertain pregnancy status. This is followed by full body computed tomography (CT) imaging, with emphasis on the lungs and brain, to evaluate for metastatic spread. Treatment is primarily chemotherapy and surgery, with excellent long-term outcomes in the setting of an early diagnosis and close monitoring of hCG levels [1, 2]. Here we describe a case of a primigravid female at 30 weeks and 5 days of gestation presenting with new-onset seizures who was found to have a pial arteriovenous malformation (AVM).
| Case Report | ▴Top |
Investigations
We present the case of a 26-year-old Caucasian female, gravida 1, para 0, at 30 weeks and 5 days of gestation whose care was transferred to our tertiary academic medical center due to persistent headaches, new-onset tonic-clonic seizures, and a brain CT scan at the outside hospital showing acute intracranial hemorrhage (Fig. 1). The patient had no prior medical problems, no prior surgeries, a negative family history, and took no medications. Magnetic resonance imaging (MRI) of her brain on arrival was concerning for a left intraparenchymal hematoma, a 5 mm midline shift, and multiple foci of restricted diffusion throughout the brain.
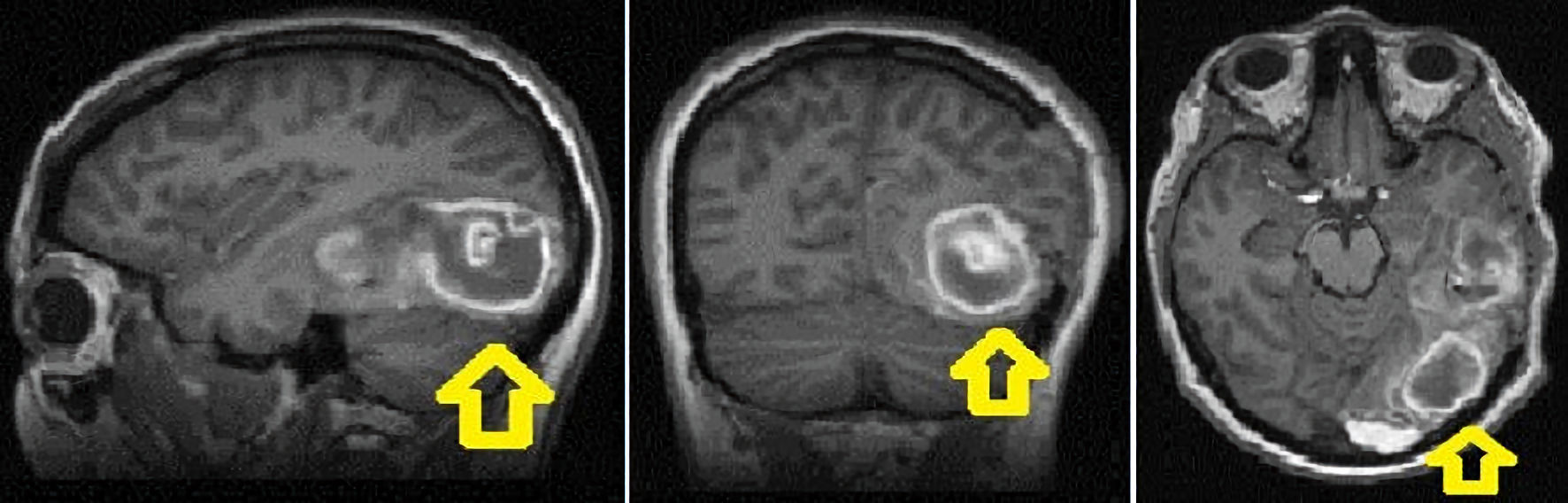 Click for large image | Figure 1. Brain MRI showed left temporal occipital intraparenchymal hematoma (as shown by arrows) measuring 3.4 × 2.4 × 3.2 cm with surrounding edema, and rightward midline shift with subfalcine and uncal herniation. MRI: magnetic resonance imaging. |
Neurosurgery was consulted, and the patient underwent an angiogram with neurointerventional radiology. A left posterior pial AVM remnant with stagnant venous flow was the presumptive diagnosis from this procedure. An interdisciplinary meeting was held including critical care, neurosurgery, obstetrics, and anesthesia. The decision was made to start the patient on anticonvulsants, repeat the cerebral angiogram in 4 weeks, and proceed with cesarean delivery at 37 weeks to avoid peri-delivery Valsalva maneuver.
Diagnosis
On hospital day 7, the patient reported worsening headache. She was taken emergently for brain MRI which showed increasing hemorrhage with 9 mm midline shift and uncal herniation. She underwent embolization of a bleeding left dural AVM under general anesthesia with invasive blood pressure monitoring. The patient tolerated anesthesia well and was hemodynamically stable throughout. She was extubated and taken to the neuro-intensive care unit (ICU) at the conclusion of the procedure.
Treatment
On post-embolization day 1 (at 31 weeks and 5 days of gestation) the patient had increased lethargy and repeat imaging revealed continued hemorrhage of the AVM. A family meeting was held, and goals of care for the mother and baby were discussed at length. In light of non-reassuring fetal heart tracings and in accordance with the family’s wishes, the decision was made to proceed with emergent cesarean delivery. Mother and baby both tolerated the procedure well under general anesthesia and, following extubation, the mother was taken again to the neuro-ICU. Later in the evening the patient once more demonstrated worsening mental status with repeat imaging that showed increasing hematoma and cerebral edema. For the fourth time in her hospital stay, the patient was emergently taken to the operating room, this time for a left craniectomy and hematoma evacuation. She underwent general anesthesia, tolerated the procedure well, and was extubated without apparent anesthetic sequela.
Follow-up and outcomes
Her hospital course over the following weeks was complicated by weakness and aphasia that progressively improved. Additional repeat imaging revealed stable hematoma. She was discharged on hospital day 21 to a rehabilitation facility. One day after discharge, placental pathology returned showing the malignant gestational trophoblastic disease, choriocarcinoma. The patient was readmitted, and a new brain MRI confirmed new areas of brain infarction along with new evidence of post-embolization dural AVM bleeding. Concern for metastatic hemorrhagic choriocarcinoma prompted full body imaging which revealed lung, labial, and brain metastases (Fig. 2).
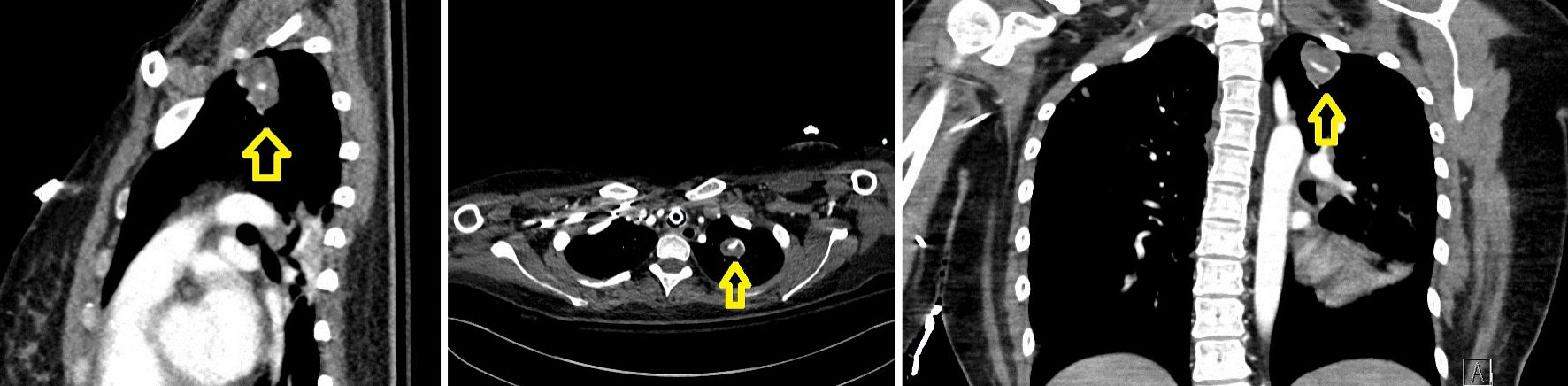 Click for large image | Figure 2. Chest CT showed left upper lobe lesion measuring 2.7 cm with prominent feeding vessel (as shown by arrows). CT: computed tomography. |
The hCG values were measured and trended throughout this admission. Initial values were greater than 225,000 mIU/mL and trended down to 30 mIU/mL after two cycles of treatment with etoposide, methotrexate, actinomycin D and cisplatin. She underwent two more neurosurgical procedures and extensive chemotherapy, but her condition deteriorated further. Increasing cerebral edema and midline shift required prolonged intubation and subsequent tracheostomy and percutaneous endoscopic gastric (PEG) tube placement. Unfortunately, her neurologic exam continued to decline. In light of a poor prognosis, the patient was made “allow natural death” and after consulting with palliative care, the family eventually decided to pursue comfort care. The patient died 3 months after initial presentation despite aggressive surgical intervention, multidrug chemotherapy, and progressively decreasing hCG levels.
| Discussion | ▴Top |
Treatment of choriocarcinoma largely depends on how aggressive the disease is and generally has very good outcomes. Mild disease without metastasis may only require long-term surveillance. More aggressive disease with metastasis generally requires multidrug chemotherapy with or without the addition of surgery and/or radiation treatment [3]. Earlier diagnosis can lead to treatment with multidrug chemotherapy before the disease becomes overwhelming, and 5-year survival can be upwards of 90%. This rate drops drastically as metastatic disease burden grows before treatment can be initiated [1]. By the time of diagnosis and chemotherapy initiation, our patient’s disease was very advanced with chest, liver, labial, and brain metastases.
While a diagnosis of choriocarcinoma is rare, the intraoperative anesthetic approach to our patient was complicated by urgency and the myriad of challenges presented by performing non-obstetrical operations on a parturient. Induction of general anesthesia, particularly after 16 weeks’ gestation, is complicated by physiologic changes of pregnancy including rapid desaturation, respiratory mucosa engorgement, progressively more difficult airway, and higher likelihood of vomiting and aspiration. Neuraxial/regional anesthesia should be considered if possible. Positioning the patient is challenging secondary to breast tissue engorgement, weight gain, and aortocaval compression. The anesthetic must be tailored to both the mother and the fetus.
Operations during pregnancy are generally reserved for urgent and emergent surgeries with elective procedures delayed until after delivery [4]. Ideally, cases are performed in the second trimester, beyond organogenesis yet before a higher chance of preterm labor in the third trimester. Depending on gestational age, there can be increased morbidity due to delays and uncertainty of when to perform a non-obstetrical procedure.
For this case, there were no delays in treatment as all of the procedures performed were emergent, since any delays would have resulted in increased maternal morbidity or mortality. The decision to have fetal monitoring and potential intervention must also be made prior to operating. Continuous fetal monitoring was utilized for each procedure performed for our patient so that appropriate action could be taken to optimize uteroplacental perfusion and fetal oxygenation. There is no data at this time regarding morbidity and mortality for pregnant patients undergoing neuroendovascular procedures, but general surgery appears to be as safe for pregnant women as it is for nonpregnant women [5].
As previously mentioned, a diagnosis of choriocarcinoma is exceedingly rare. It develops in approximately one in every 50,000 otherwise normal deliveries [1]. Molar disease, spontaneous abortion, and ectopic pregnancy can precede choriocarcinoma. Choriocarcinoma can be localized to the placenta or produce highly vascular metastasis. One large systematic review reported that metastatic disease occurred in 52% of identified cases with pulmonary metastasis being most common, followed by uterine, brain, and then vaginal sites [3]. These metastases can produce hematuria, hemoptysis, hematemesis, hematochezia, seizure, stroke, or vaginal bleeding. Other clinical presentations include headache, lethargy, as well as severe and intractable back pain [6, 7]. Given these potential nonspecific presenting symptoms, the differential can be quite long and delay the diagnosis of choriocarcinoma.
Typically, the diagnosis is made based on history, imaging studies, and serum hCG level. In pregnancy serum hCG levels are already elevated. Elevated hCG levels are not pathognomonic for choriocarcinoma. However, a significantly elevated serum hCG along with appropriate history is highly suggestive of choriocarcinoma [8].
Our patient’s first presenting sign was seizure with subsequently diagnosed intracranial bleeding. It was not until 3 weeks after cesarean delivery (4 weeks after her first seizure) that the diagnosis of choriocarcinoma was made from pathology of the placenta and a labial hematoma that was later found to be a metastasis. In addition, she had a seemingly clear cause for her intraparenchymal bleed. AVM and aneurysms are among the most common causes of intracranial hemorrhage in pregnancy [9]. An arteriovenous fistula of the posterior cerebral artery was initially suspected and successfully embolized in our patient, thus leaving the concern for metastatic disease low on the differential.
Learning points
Choriocarcinoma is extremely rare in viable pregnancies, but it should be considered when a parturient presents with intracranial bleeding. A high level of suspicion and serial serum hCG levels may lead to early and potentially life-saving multidrug chemotherapy. Unfortunately, in the case presented, the disease was advanced, and diagnosis delayed. Our patient’s disease resulted in several intracranial bleeds leading to devastating brain injury and ultimately death despite aggressive treatment. With a broader differential, earlier hCG measurement, and earlier treatment our patient may have survived.
Acknowledgments
The authors do not have any additional contributors to acknowledge.
Financial Disclosure
The authors did not receive any specific funding, and the writeup of this article was performed of their own volition while working at Medical University of South Carolina in the department of Anesthesia and Perioperative Medicine.
Conflict of Interest
The authors declare that there is no conflict of interest regarding the publication of this article. The authors declare that they have not received any funding, payments, goods or services that may influence their work on this publication.
Informed Consent
Publication was approved by the patient prior being deceased as well as an ethics committee and privacy officer postmortem. There is no identifiable information.
Author Contributions
Deborah A. Romeo helped coordinate the writeup, collected the data, analyzed the case, and wrote up the case report. David A. Gutman assisted with coordinating the writeup submission, collected the data, analyzed the case, and wrote up the case report. Joel Sirianni performed the clinical case, reviewed the collected the data, analyzed the case, and revised the case report for critically important intellectual content. Michael Marotta assisted with coordinating the writeup submission, collected the data, formatted the images, analyzed the case, and assisted with multiple revisions of the case report.
Data Availability
Any inquiries regarding supporting data availability of this study should be directed to the corresponding author.
Abbreviations
hCG: human chorionic gonadotropin; CT: computed tomography; MRI: magnetic resonance imaging; AVM: arteriovenous malformation: ; ICU: intensive care unit; PEG: percutaneous endoscopic gastric
| References | ▴Top |
- Seckl MJ, Sebire NJ, Berkowitz RS. Gestational trophoblastic disease. Lancet. 2010;376(9742):717-729.
doi - Ngan S, Seckl MJ. Gestational trophoblastic neoplasia management: an update. Curr Opin Oncol. 2007;19(5):486-491.
doi pubmed - Jiao L, Ghorani E, Sebire NJ, Seckl MJ. Intraplacental choriocarcinoma: Systematic review and management guidance. Gynecol Oncol. 2016;141(3):624-631.
doi pubmed - Frohlich MA. Maternal and fetal physiology and anesthesia. In: Butterworth JF, Mackey DC, Wasnick JD, editors. Morgan and Mikhail's clinical anesthesiology, 6th ed. New York: McGraw-Hill Education; 2018; p. 825-843.
- Moore HB, Juarez-Colunga E, Bronsert M, Hammermeister KE, Henderson WG, Moore EE, Meguid RA. Effect of pregnancy on adverse outcomes after general surgery. JAMA Surg. 2015;150(7):637-643.
doi pubmed - Mamelak AN, Withers GJ, Wang X. Choriocarcinoma brain metastasis in a patient with viable intrauterine pregnancy. Case report. J Neurosurg. 2002;97(2):477-481.
doi pubmed - Huang L, Huang SY, Lee AL, Hung TH. Choriocarcinoma in a viable pregnancy with the rare presentation of intractable lower back pain. Taiwan J Obstet Gynecol. 2021;60(6):1098-1102.
doi pubmed - Salani R, Copeland LJ. Malignant diseases and pregnancy. In: Gabbe S, Niebyl J, Simpson J, Landon M, Galan H, Jauniaux E, Driscoll D, et al., editors. Obstetrics: normal and problem pregnancies, 7th ed. Philadelphia: Elsevier. 2016; p. 1057-1074.
- Fairhall JM, Stoodley MA. Intracranial haemorrhage in pregnancy. Obstet Med. 2009;2(4):142-148.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


