| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 13, Number 3, March 2022, pages 125-128
Prolonged Lactobacillus Bacteremia With Abdominal Abscesses Secondary to Traumatic Injuries From Pet Dogs: A Case Report
Wesley Tanga, c , Marco Comianosa, Satish Sarvepallib
aDepartment of Medicine, Kettering Medical Center, Kettering, OH, USA
bDivision of Infectious Disease, South Dayton Acute Care Consultants, Dayton, OH, USA
cCorresponding Author: Wesley Tang, Department of Medical Education, Kettering Medical Center, Dayton, OH 45429, USA
Manuscript submitted November 18, 2021, accepted February 23, 2022, published online March 5, 2022
Short title: Lactobacillus Bacteremia With Abdominal Abscesses
doi: https://doi.org/10.14740/jmc3851
| Abstract | ▴Top |
Lactobacillus casei is a non-spore forming gram-positive rod considered to be normal flora of the oropharynx and gastrointestinal tract. Additionally, Lactobacillus spp. are commonly used as probiotics and other commercial products. Invasive infections are rarely encountered and have been associated with underlying immunosuppression or malignancy. Here, we present a case of prolonged Lactobacillus bacteremia and multiple intra-abdominal abscesses likely as a result of injuries associated with pet dogs.
Keywords: Lactobacillus; Bacteremia; Splenic abscesses; Zoonotic infection
| Introduction | ▴Top |
Lactobacillus are non-spore forming, facultative anaerobic, gram-positive rods, which are considered commensal flora of the oropharynx and gastrointestinal tract [1]. They are used for a variety of commercial products including biological catalysts for the production of organic compounds, used as starter cultures, and probiotics [2]. In the presence of certain risk factors Lactobacilli have been responsible for serious infections such as bacteremia, infective endocarditis, and intra-abdominal abscesses [3-5]. Predisposing factors risk factors for serious Lactobacillus infections have included structural heart disease, leukemia, and immunosuppression in transplant patients [6, 7]. Bacteremia and intra-abdominal abscesses as a result of Lactobacillus is rare, with only 11 cases reported in the literature [8]. We add to this number by reporting a case of persistent bacteremia and splenic abscess caused by Lactobacillus casei.
| Case Report | ▴Top |
Investigations
The patient is a 44-year-old male with a past medical history significant for intravenous (IV) drug use, candidal endocarditis status (post bioprosthetic aortic valve replacement, 9 years prior to presentation), now in remission who presented with generalized abdominal pain, which started 6 days prior, with associated nausea and vomiting. The patient admitted to rough playing with his pet bulldogs and denied immunosuppression, probiotic use, or recreational/illegal drug use since his aortic valve replacement. The patient also complained of intermittent fevers. He was initially seen by his primary care physician (PCP) who started the patient on ciprofloxacin and metronidazole out of concern for diverticulitis. The patient’s PCP also ordered a computed tomography (CT) scan of the abdomen and pelvis (A/P) that revealed multiple abnormalities (imaging unattainable), which prompted the PCP to immediately ask the patient to report to the emergency department (ED) for further evaluation.
Diagnosis
While in ED, repeat CT imaging revealed large fluid collections in the spleen (14 × 10.9 × 2.6 cm), left pelvic region (8.3 × 27.7 × 7.7 cm) and deep pelvic region (13.4 × 6.7 × 4.5 cm) concerning for abscesses vs. hematomas. Initial vitals were stable and pertinent physical exam findings included open abdominal wall ulcers with multiple scratch marks and lower abdominal pain on palpation. Labs were significant for leukocytosis and thrombocytosis. Blood cultures were also obtained. The patient was hospitalized for further management.
While hospitalized general surgery felt there was no surgical intervention needed. They recommended infectious disease (ID) consult and interventional radiology (IR) for drain placement.
The patient underwent drain placement to the left lower quadrant fluid collection with the return of purulent fluid. This would later grow Lactobacillus and identified via matrix-assisted laser desorption ionization-time of flight (MALDI-TOF). The patient had another drain placed in the transgluteal region, which also later grew Lactobacillus. Initial blood cultures grew Lactobacillus casei, with culture data demonstrating sensitivity to ampicillin, penicillin, clindamycin, and erythromycin. Unfortunately, minimum inhibitory concentrations (MICs) were not reported. The patient was then started on ampicillin/sulbactam out of concern that the source of the Lactobacillus infection was zoonotic/exogenous source from the mouth of the patient’s dogs versus trauma induced translocation of endogenous flora in a patient with diverticulosis. On hospital day 2, a transthoracic echocardiogram was performed with no evidence for vegetations. Subsequent blood cultures on day 5 of admission continued to grow Lactobacillus casei, sensitive to ampicillin/sulbactam. A transesophageal echocardiogram was performed 7 days after the first positive culture and was also negative for vegetations.
Treatment
Prior to discharge, blood cultures were negative and repeat CT abdomen/pelvis revealed a decrease in size of the abscesses. The patient was discharged on day 10 of hospitalization with drains in place and plan for continuation of amoxicillin/clavulanic acid, 875/125 mg oral tablet, twice daily, for 6 weeks. He was instructed to follow up with ID and general surgery on an outpatient basis.
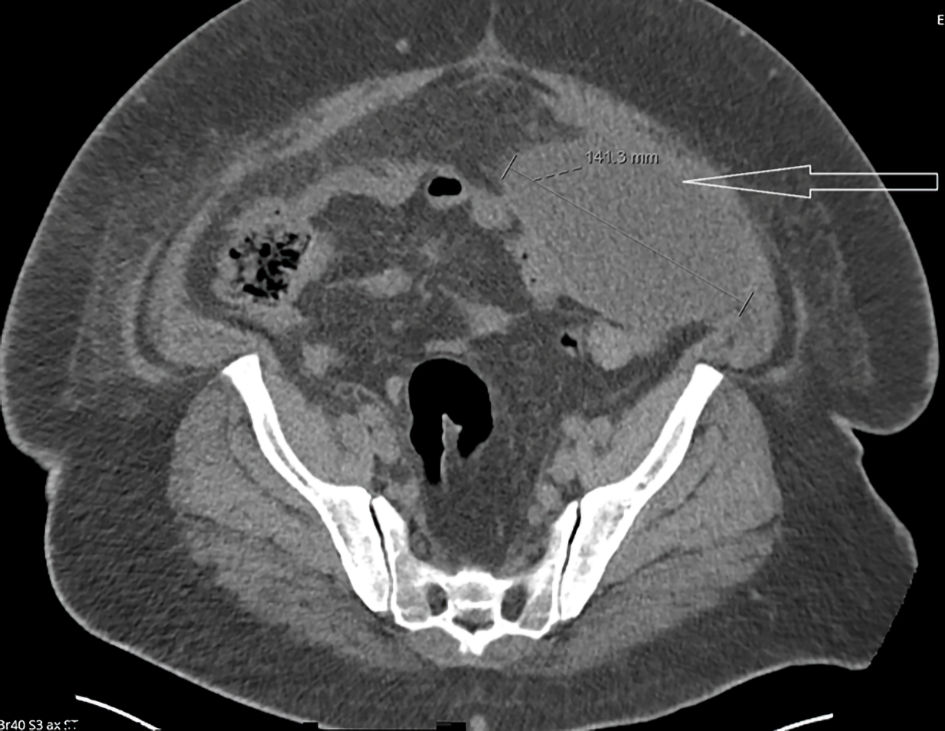
The patient was subsequently rehospitalized a few days later (14 days from first presentation) with worsening fever, altered mental status, and sepsis. He underwent a repeat CT abdomen/pelvis which showed an increase in size of the deep pelvic abscess to 9 × 3 cm, previously 6.6 × 4.6 cm, in which a drain was already in place. It also showed stable splenic and left-sided pelvic abscesses (Figs. 1, 2). A repeat transthoracic echocardiogram 16 days after the first positive culture was also negative for vegetations. The patient was restarted on IV ampicillin/sulbactam 3 g IV every 6 h. Blood cultures remained negative through this hospital stay. Surgery did not recommend surgical intervention and recommended IR drain placement to the splenic abscess which occurred later this hospital admission. This fluid culture again grew Lactobacillus casei as well as light growth of Staphylococcus aureus later revealing methicillin-sensitive Staphylococcus aureus. He was continued on ampicillin/sulbactam. Due to decreased output from the patient’s drains, a repeat CT was ordered which revealed some improvement. The splenic abscess measured 9.8 × 12.7 cm, improved from 12.7 × 15.5 cm. The left-sided pelvic abscess measured 1.9 × 3.7 cm, improved from 2.5 × 10.7 cm. The deep pelvic fluid abscess improved to 2.4 × 5.62 cm, from 3.3 × 9.2 cm. Due to these findings, the patient was discharged on IV antibiotics, with plan to continue ampicillin/sulbactam, 3 g IV every 6 h, for 2 to 3 weeks (23 days from first presentation). Patient was to follow up with general surgery as well as ID for drain management as well as antimicrobial surveillance respectively.
 Click for large image | Figure 1. Computed tomography (CT) scan of the abdomen demonstrating a large fluid density mass within the spleen (arrow). |
 Click for large image | Figure 2. Computed tomography (CT) scan of the abdomen demonstrating oblong collections in the left lower quadrant omentum and within the pelvis containing predominantly indeterminate fluid (arrow). |
Follow-up and outcomes
In the subsequent 2-week post-hospitalization follow-up, the patient continued to have issues with his drain. He would later undergo drain exchange for his intrasplenic abscess (33 days from first presentation). Fluid culture would again reveal Lactobacillus. Plan was then revised to continue the patient on IV antibiotics for another 4 weeks. Repeat CT imaging would reveal improvement in his splenic abscess, now 5.9 × 5.2 cm as well as resolution of other intra-abdominal abscesses (47 days from first presentation). The patient continued to have ongoing drainage, and repeated drain malfunction for the next several months during which time he was maintained on amoxicillin/clavulanic acid, 875/125 mg oral tablet, twice daily. In summary, the patient would receive antibiotics for a total of 19 weeks and has not had recurrence of fever or abdominal pain for the last 5 months. The patient reported no adverse events throughout the treatment course.
| Discussion | ▴Top |
Lactobacillus species are often regarded as commensal organisms and thus, contaminants in the laboratory and of low virulence. At the same time, Salminen et al report that overall mortality from Lactobacillus spp. was found to be 26% at 1 month and 48% at 1 year [9].
Due to the infrequency of Lactobacilli infections, there are currently no clinical guidelines recommending certain antimicrobial regimens nor are there guidelines for the duration of therapy. A retrospective review of over 200 cases found isolates to be most sensitive to erythromycin (94.3%) and clindamycin (90.0%) while 63.6% of isolates demonstrated sensitivity to penicillin [10]. Lactobacillus casei and Lactobacillus rhamnosus have been reported to be resistant to metronidazole, vancomycin, ciprofloxacin, and sulfonamides [11, 12]. The present authors opted to treat the patient with ampicillin/sulbactam based on the repeated sensitivities of the organism. We further highlight the educational value of this case as the persistent bacteremia was almost certainly due to the lack of source control given his multiple abscesses and repeated drain malfunction.
Aside from a significant amount of dog scratches, the patient did not have traditional risk factors for Lactobacilli bacteremia as reported in the literature such as immunosuppression, history of transplantation, uncontrolled diabetes, known malignancy, recent dental procedures, poor dental condition, or IV drug use in the preceding 9 years prior to presentation. He likewise denied the use of probiotic consumption or exposure to recent antibiotics. Despite the presence of a bioprosthetic aortic valve replacement in 2012, infective endocarditis was quickly ruled out and no source of the bacteremia was ever identified. Consequently, the authors speculate that the bacteremia was a result of trauma, injuries, and/or bites while interacting with the patient’s pet pitbulls. The organism could have been introduced exogenously from the dog’s oropharynx via licking/biting, or introduced endogenously whereby trauma whilst playing with his dogs may have caused a translocation event of normal gut flora into the bloodstream.
As our patient was relatively young with few comorbidities, our patient has made a full recovery following prolonged percutaneous drainage and antibiotic course. Because of the unusual circumstances of this infection, further research is needed to further elucidate the pathogenesis and virulence factors associated with Lactobacillus bacteremia in order to better understand prevention and treatment.
Learning points
Lactobacillus species have been described as commensal organisms of low virulence, seldom causing serious infections. In the case of persistent bacteremia, the source of ongoing bacteremia must be identified. Given that there are no current guidelines on the treatment of this organism, this patient was treated with ampicillin/sulbactam, and later amoxicillin/clavulanate.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Informed Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Author Contributions
WT, MC, SS designed and conducted the research. SS provided the data. WT had primary responsibility for the final content. All authors have read and approved the final manuscript.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Goldstein EJ, Tyrrell KL, Citron DM. Lactobacillus species: taxonomic complexity and controversial susceptibilities. Clin Infect Dis. 2015;60(Suppl 2):S98-107.
doi pubmed - Hatti-Kaul R, Chen L, Dishisha T, Enshasy HE. Lactic acid bacteria: from starter cultures to producers of chemicals. FEMS Microbiol Lett. 2018;365(20):fny213
doi pubmed - Sherid M, Samo S, Sulaiman S, Husein H, Sifuentes H, Sridhar S. Liver abscess and bacteremia caused by lactobacillus: role of probiotics? Case report and review of the literature. BMC Gastroenterol. 2016;16(1):138.
doi pubmed - Salvana EM, Frank M. Lactobacillus endocarditis: case report and review of cases reported since 1992. J Infect. 2006;53(1):e5-e10.
doi pubmed - Antoun M, Hattab Y, Akhrass FA, Hamilton LD. Uncommon pathogen, lactobacillus, causing infective endocarditis: case report and review. Case Rep Infect Dis. 2020;2020:8833948.
doi pubmed - Cohen SA, Woodfield MC, Boyle N, Stednick Z, Boeckh M, Pergam SA. Incidence and outcomes of bloodstream infections among hematopoietic cell transplant recipients from species commonly reported to be in over-the-counter probiotic formulations. Transpl Infect Dis. 2016;18(5):699-705.
doi pubmed - Sussman JI, Baron EJ, Goldberg SM, Kaplan MH, Pizzarello RA. Clinical manifestations and therapy of Lactobacillus endocarditis: report of a case and review of the literature. Rev Infect Dis. 1986;8(5):771-776.
doi pubmed - Ramos-Coria D, Canto-Losa J, Carrillo-Vazquez D, Carbajal-Morelos L, Estrada-Leon R, Corona-Rodarte E. Lactobacillus gasseri liver abscess and bacteremia: a case report. BMC Infect Dis. 2021;21(1):518.
doi pubmed - Salminen MK, Rautelin H, Tynkkynen S, Poussa T, Saxelin M, Valtonen V, Jarvinen A. Lactobacillus bacteremia, clinical significance, and patient outcome, with special focus on probiotic L. rhamnosus GG. Clin Infect Dis. 2004;38(1):62-69.
doi pubmed - Cannon JP, Lee TA, Bolanos JT, Danziger LH. Pathogenic relevance of Lactobacillus: a retrospective review of over 200 cases. Eur J Clin Microbiol Infect Dis. 2005;24(1):31-40.
doi pubmed - Salminen MK, Rautelin H, Tynkkynen S, Poussa T, Saxelin M, Valtonen V, Jarvinen A. Lactobacillus bacteremia, species identification, and antimicrobial susceptibility of 85 blood isolates. Clin Infect Dis. 2006;42(5):e35-44.
doi pubmed - Kyriacou A, Tsimpidi E, Kazantzi E, Mitsou E, Kirtzalidou E, Oikonomou Y, Gazis G, et al. Microbial content and antibiotic susceptibility of bacterial isolates from yoghurts. Int J Food Sci Nutr. 2008;59(6):512-525.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


