| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 13, Number 1, January 2022, pages 11-14
Inferior Myocardial Infarction Secondary to Coronary Artery Vasospasm Following Regadenoson Stress Imaging
Benjamin Fogelsona, b, James Livesaya, Jeffrey H. Johnsona
aDepartment of Medicine, University of Tennessee Graduate School of Medicine, Knoxville, TN, USA
bCorresponding Author: Benjamin Fogelson, Department of Internal Medicine, University of Tennessee Medical Center, 1924 Alcoa Highway, U114 Knoxville, TN 37920-6999, USA
Manuscript submitted November 12, 2021, accepted November 26, 2021, published online January 17, 2022
Short title: Inferior MI Secondary to CAV
doi: https://doi.org/10.14740/jmc3850
| Abstract | ▴Top |
Coronary artery vasospasm is a rare condition that is caused by hyperactive arterial smooth muscle vasoconstriction leading to reversible coronary artery occlusion. Patients that suffer from coronary artery vasospasm have the potential to develop life-threatening conditions such as myocardial infarction and fatal arrhythmias. ST-elevations are a rare complication that can occur in people with coronary vasospasm, and to the best of our knowledge there are no documented cases of ST-elevation myocardial infarction occurring in patients undergoing regadenoson stress test. We present a unique case of a patient with known coronary artery disease and catheter-induced coronary artery vasospasm who developed ST-segment elevations and typical angina immediately following the administration of regadenoson during an elective myocardial stress test.
Keywords: Coronary vasospasm; Regadenoson; Myocardial perfusion imaging; Stress test
| Introduction | ▴Top |
Coronary artery vasospasm (CAV), also known as vasospastic angina, is an uncommon condition that involves the partial or complete occlusion of a coronary artery secondary to reversible vasoconstriction [1]. CAV has been found to cause up to 1.5% of all angina hospital admissions [2]. Patients with CAV typically present with symptoms consistent with typical angina; however, they can also present with fatal arrhythmias and/or acute myocardial infarction [1, 3]. Lanza et al found that approximately 17% of patients with ST-segment changes secondary to CAV had evidence of myocardial infarction [2]. Unfortunately, the diagnosis of CAV can be delayed due to unremarkable electrocardiograms (ECGs), negative stress testing, and the absence of significant coronary artery disease (CAD) on coronary angiography [2]. Subsequently, CAV has primarily become a diagnosis of exclusion.
CAV can be observed during coronary angiography secondary to an acute vasoconstriction episode, mechanical stimulation of the artery with engagement of the catheter, or an intra-coronary injection of an arterial vasoconstrictor [2]. In comparison, CAV is rarely captured during cardiac stress testing. There are published case reports that have demonstrated CAV during adenosine stress testing [4]. Despite similar adenosine receptor activation properties, regadenoson has been less commonly associated with CAV during stress testing [5, 6]. There have been very few cases of CAV captured immediately following regadenoson stress testing. To our knowledge, there are no reported cases of ST-segment elevation myocardial infarction (STEMI) secondary to CAV following regadenoson stress testing. We report a unique case of an inferior STEMI secondary to CAV immediately following regadenoson stress myocardial perfusion imaging in a patient with a history of CAD and coronary artery bypass grafting (CABG).
| Case Report | ▴Top |
Investigations
A 60-year-old female presented with recurrent episodes of typical angina. Her history was significant for CAD, hypertension, hyperlipidemia, obesity, and tobacco use. She underwent CABG 12 years prior with a saphenous vein graft to the obtuse marginal branch of the circumflex artery and the left internal mammary artery to the left anterior descending artery. In the setting of known CAD with previous CABG and symptoms suggestive of typical angina we elected to proceed with a regadenoson stress myocardial perfusion scan. As part of our protocol, a baseline ECG was obtained showing normal sinus rhythm and non-specific ST wave changes (Fig. 1). Our patient then received administration of regadenoson (0.4 mg intravenous (IV) over 15 s) and immediately developed severe substernal chest pressure with associated shortness of breath.
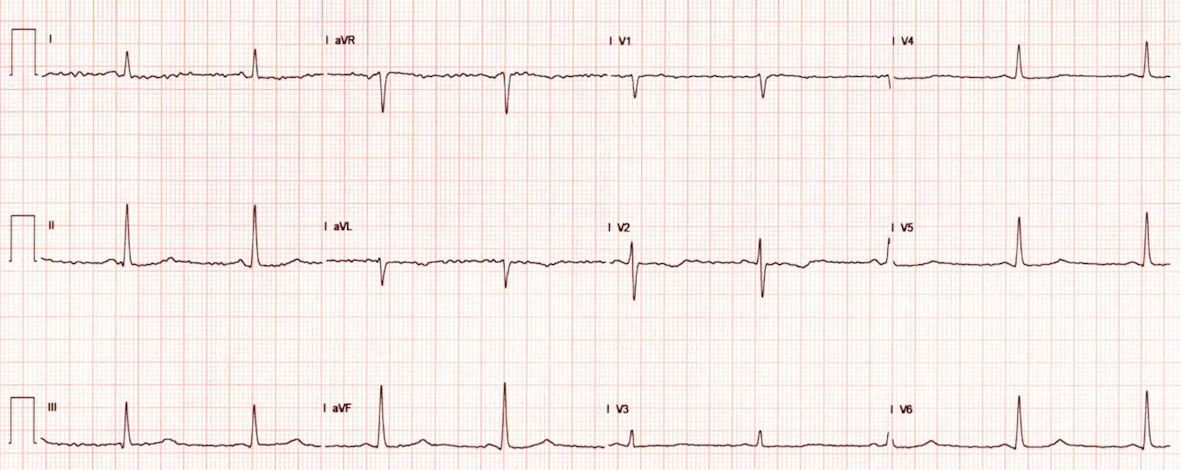 Click for large image | Figure 1. Electrocardiogram prior to regadenoson stress myocardial perfusion imaging demonstrating normal sinus rhythm and nonspecific ST changes. |
Diagnosis
A stat ECG was performed demonstrating ST-segment elevations in the inferior leads (II, III, and aVF) consistent with an acute inferior STEMI (Fig. 2). She was given nitroglycerin and emergently taken to the cardiac catheterization laboratory for left heart catheterization with possible percutaneous intervention. Coronary angiography revealed mild to moderate nonobstructive CAD but no explanation for her sudden onset symptoms or ECG changes (Fig. 3). Follow-up ECGs demonstrated complete resolution of ST-segment elevations. Initial and serial troponins were unremarkable at 0.00 ng/mL, 0.03 ng/mL and 0.01 ng/mL, respectively (reference range: 0.00 - 0.78). In further review of her outpatient records, the patient had a documented history of catheter-induced CAV of the right coronary artery during a previous coronary angiogram. The diagnosis of CAV was made based on her symptomatology, post-stress test ECG findings, rapid resolution of pain with nitroglycerin, unremarkable coronary angiographic findings, and in the setting of prior catheter-induced vasospasm.
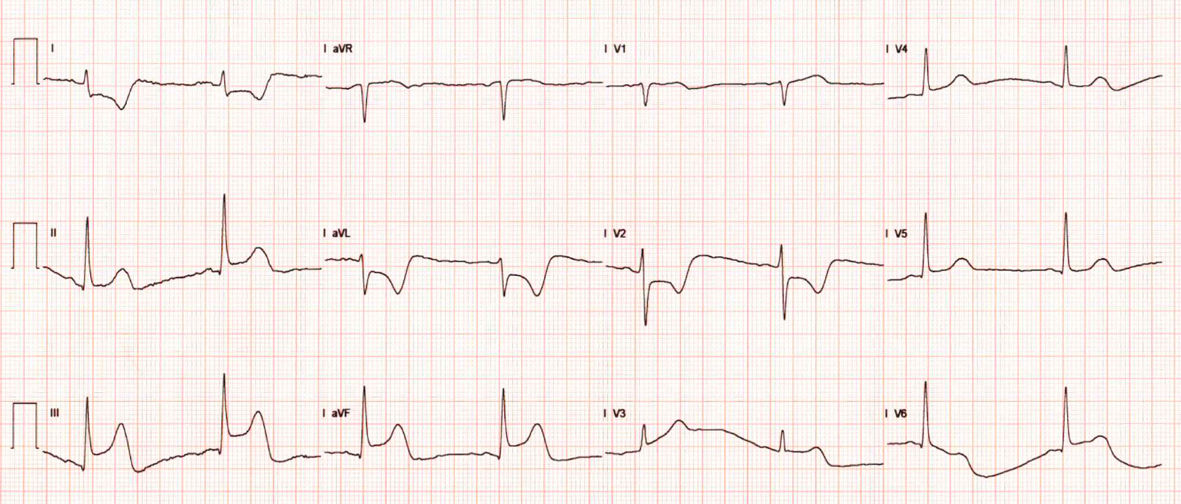 Click for large image | Figure 2. Electrocardiogram demonstrating inferior ST-segment elevation with associated reciprocal changes immediately following regadenoson stress myocardial perfusion imaging. |
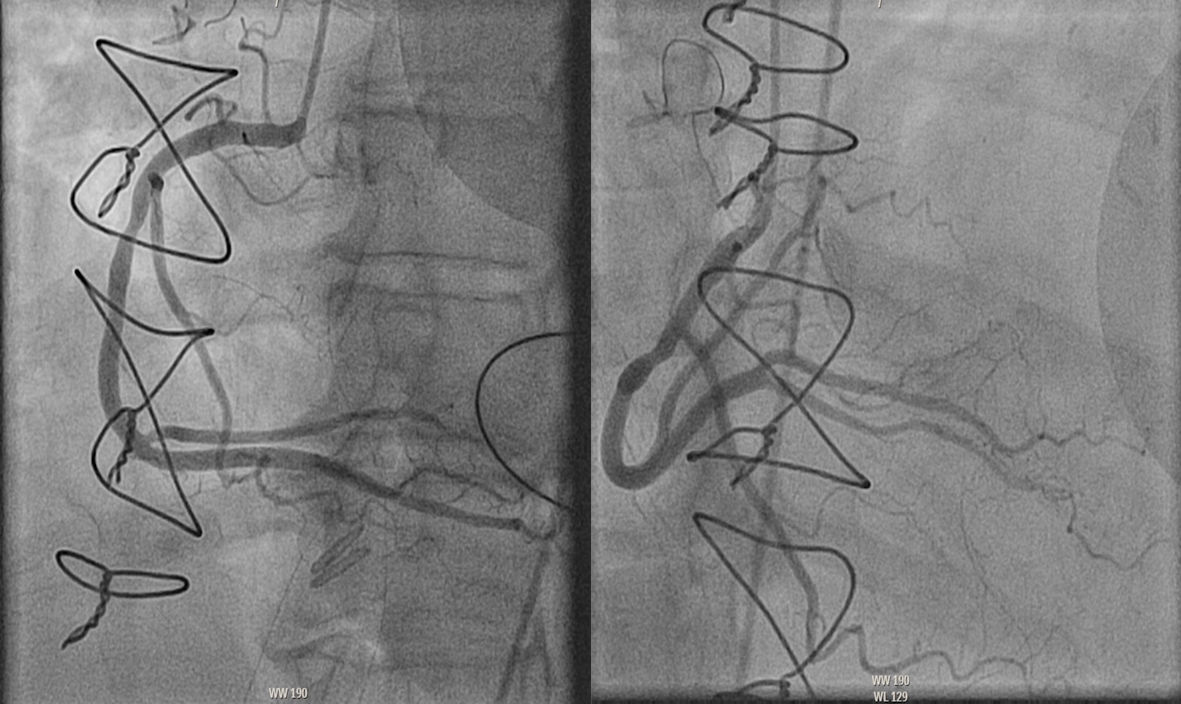 Click for large image | Figure 3. Right coronary artery angiography demonstrating no angiographically significant stenosis to explain the patient’s acute inferior ST-elevation myocardial infarction. |
Treatment
Medical management with amlodipine and isosorbide was initiated.
Follow-up and outcomes
After starting medical therapy, she had no recurrence of her symptoms. She had no complications following her procedure and was therefore safely discharged home in stable condition. She is regularly seen in our clinic and has not reported any new concerns or adverse events.
| Discussion | ▴Top |
CAV is a rare condition that is caused by reversible subtotal or total occlusion of a coronary artery branch [1]. Physiologically, CAV is the result of local coronary smooth muscle hyperactivity leading to coronary artery occlusion [7]. Prompt diagnosis of CAV is crucial to prevent many serious life-threatening conditions such as myocardial infarction and fatal arrhythmias [2]. According to Lanza et al, patients with STEMI secondary to CAV have been shown to have an increased risk of major cardiac events [2]. STEMI secondary to CAV is usually a diagnosis of exclusion; however, it can be captured on a stat ECG or during emergent coronary angiography immediately following an acute chest pain presentation [8, 9]. In comparison, the diagnosis of CAV without ST-elevation or other ischemic changes on ECG is frequently delayed given that most diagnostic testing is unremarkable [2]. Previously, the administration of IV ergonovine or acetylcholine was used to provoke CAV; however, they have since fallen out of favor due to severe side effects.
Although approximately 40% of patients with STEMI secondary to CAV are found to have > 50% coronary stenosis on cardiac catheterization, CAD and CAV do not share identical risk factors [2, 10]. According to Hung et al, older age, smoking, and elevated C-reactive protein levels were found to be the main risk factors for CAV [10]. Patients with prior coronary stenting have also been known to develop CAV involving the coronary smooth muscle just distal to the stent. Our patient was found to have mild to moderate nonobstructive CAD in the setting of an acute STEMI secondary to CAV, despite her history of CAD. This case demonstrates that regardless of cardiac history, CAV should be a differential diagnosis in patients presenting with symptoms consistent with angina or acute coronary syndrome (ACS).
Prior reports of patients who presented as a STEMI secondary to CAV during pharmacologic cardiac stress imaging are limited. The pharmacologic agent, regadenoson, has been found to cause coronary vasoconstriction during stress testing due to its adenosine receptor activation properties. To the best of our knowledge, prior cases of regadenoson associated CAV have demonstrated either no ECG changes or non-specific ischemic ECG changes [5, 6]. Our case is unique in that our patient demonstrated classic findings of an inferior STEMI secondary to CAV immediately following regadenoson stress testing. We were able to capture active CAV causing an inferior STEMI during stress myocardial perfusion imaging. This case stresses the importance of acknowledging CAV as a cause of STEMI during pharmacologic stress testing when using an adenosine receptor agonist.
Prompt diagnosis and treatment of CAV is crucial to prevent life-threatening conditions such as STEMI and fatal arrhythmias [2]. The diagnosis of CAV is challenging and typically requires a process of elimination that utilizes both symptoms and diagnostic testing such as ECG, cardiac catheterization, and/or stress testing. Given the vasoconstrictive pathophysiology of CAV, the primary treatment is coronary vasodilation with nitrates [9]. Commonly, patients presenting with STEMI secondary to CAV with an obvious vasospastic lesion receive intra-coronary nitrate injections during emergent coronary angiography [8]. Our patient’s symptoms resolved completely after the administration of sublingual nitroglycerin. This emphasizes the importance of immediate administration of nitrates to patients with suspected or known CAV that present with symptoms consistent with angina or ACS.
Conclusions
CAV is an uncommon condition of reversible coronary artery occlusion that is rarely captured during pharmacologic stress myocardial perfusion imaging. Few case reports have reported CAV during regadenoson stress testing. We report a very unusual case of an inferior STEMI secondary to CAV immediately following a regadenoson stress test in a patient with only mild to moderate nonobstructive CAD on angiogram. Our case highlights the importance of considering CAV as the cause of STEMI during pharmacologic stress testing, especially with the use of adenosine receptor agonists. It also emphasizes the importance of nitrates in the treatment of CAV to prevent life-threatening cardiac events.
Learning points
CAV can cause symptoms and ECG findings consistent with acute ST-elevation myocardial infarction. ST-elevation myocardial infarction secondary to CAV can occur during regadenoson stress myocardial perfusion imaging and should be considered in all patients that develop angina during pharmacologic stress testing. Regardless of cardiac history, CAV should be a differential diagnosis in patients presenting with angina. Lastly, prompt diagnosis and treatment of CAV is crucial to prevent major cardiac events.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Informed consent was obtained.
Author Contributions
All authors reviewed the literature and helped write the manuscript. Benjamin Fogelson, DO, James Livesay, DO, and Jeffrey H. Johnson, MD performed critical revisions of article and approved the final version of manuscript.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
Abbreviations
CAV: coronary artery vasospasm; ECG: electrocardiogram; CAD: coronary artery disease; STEMI: ST-segment elevation myocardial infarction; CABG: coronary artery bypass grafting; ACS: acute coronary syndrome
| References | ▴Top |
- Kaski JC, Maseri A, Vejar M, Crea F, Hackett D. Spontaneous coronary artery spasm in variant angina is caused by a local hyperreactivity to a generalized constrictor stimulus. J Am Coll Cardiol. 1989;14(6):1456-1463.
doi - Lanza GA, Sestito A, Sgueglia GA, Infusino F, Manolfi M, Crea F, Maseri A. Current clinical features, diagnostic assessment and prognostic determinants of patients with variant angina. Int J Cardiol. 2007;118(1):41-47.
doi pubmed - Crea F, Lanza GA. New light on a forgotten disease: vasospastic angina. J Am Coll Cardiol. 2011;58(12):1238-1240.
doi pubmed - Shah S, Parra D, Rosenstein RS. Acute myocardial infarction during regadenoson myocardial perfusion imaging. Pharmacotherapy. 2013;33(6):e90-95.
doi pubmed - Nam JG, Choi SH, Kang BS, Bang MS, Kwon WJ. Development of coronary vasospasm during adenosine-stress myocardial perfusion CT imaging. Korean J Radiol. 2015;16(3):673-677.
doi pubmed - Bagley SJ, Lilly SM, Litwack AJ. Coronary vasospasm during a regadenoson stress test. Cardiol J. 2012;19(1):92-94.
doi pubmed - Platsman Z, Auerbach A, Lee A, Jauhar R, Makaryus JN. Regadenoson-induced coronary vasospasm resulting in severe reversible perfusion defects and transient ischemic dilation on SPECT stress myocardial perfusion imaging. J Nucl Cardiol. 2016;23(4):843-845.
doi pubmed - Kaya C, Altay S. An extreme case of vasospastic angina mimicking acute STEMI: Severe threevessel disease with critical stenoses. Anatol J Cardiol. 2019;21(6):347-349.
doi - Pendela VS, Kudaravalli P, Chhabria M, Balmer-Swain M. ST segment elevation in an adult chest pain patient: A case of coronary artery vasospasm. Am J Emerg Med. 2020;38(8):1699.e1-e3.
doi pubmed - Hung MJ, Hu P, Hung MY. Coronary artery spasm: review and update. Int J Med Sci. 2014;11(11):1161-1171.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


