| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 11, Number 6, June 2020, pages 185-188
Spontaneous Coronary Artery Dissection in a Young Man
Stella Paka, d, Edinen Asukab, Anastasia Postoevc
aDepartment of Medicine, Orange Regional Medical Center, Middletown, NY, USA
bAll Saints University School of Medicine, Roseau, Dominica
cDepartment of Medicine, Caribbean Medical University, 5600 N River Rd, Rosemont, IL 60018, USA
dCorresponding Author: Stella Pak, Department of Medicine, Orange Regional Medical Center, 707 East Main Street, Middletown, NY 10940, USA
Manuscript submitted May 8, 2020, accepted May 15, 2020, published online May 28, 2020
Short title: SCAD in a Young Man
doi: https://doi.org/10.14740/jmc3490
| Abstract | ▴Top |
Spontaneous coronary artery dissection (SCAD) is an idiosyncratic phenomenon by which a spontaneous separation of the intimal and medial layer in the coronary artery occurs with intramural hemorrhage in the absence of trauma. This intramural hematoma, in turn, leads to compression and occlusion of the arterial lumen. Unlike traumatic dissection of coronary arteries, more than half of SCAD heals spontaneously over time. SCAD is known to occur predominantly in women under the age of 50, particularly during pregnancy or peripartum period. Herein, we present a case of a 32-year-old man with an SCAD on the left anterior descending coronary artery. The discordance between clinical presentation and angiographic finding posed a unique challenge in therapeutic decision making. This case reminds clinicians that SCAD should be kept in mind as a differential diagnosis even for young men presenting with acute chest pain.
Keywords: Spontaneous coronary artery dissection; Coronary artery bypass grafting; Percutaneous coronary intervention; Coronary angiography; Optical coherence tomography; Intravascular ultrasound; Thrombolysis in myocardial infarction; Dual antiplatelet therapy
| Introduction | ▴Top |
Spontaneous coronary artery dissection (SCAD) is a rare anomaly that involves the abrupt separation of the intimal and medial layer in the coronary artery leading to the formation of intramural hemorrhage within the false lumen. This intramural hematoma, in turn, leads to compression and occlusion of the arterial lumen [1]. SCAD has a broad spectrum of clinical presentation, ranging from asymptomatic state to myocardial infarction, cardiogenic shock, and sudden cardiac death [2]. It is estimated that approximately 1.7-4% of acute coronary syndrome (ACS) is attributed to SCAD. More than 90% of SCAD occurs in women due to higher level of progesterone compared to men. Progesterone disrupts delicate vascular structure by impairing synthesis of collagen and damaging mucopolysaccharides and elastic fibers. During pregnancy and peripartum period, women are exposed to persistently elevated level of progesterone. Due to this progesterone exposure in addition to physiological stress on cardiovascular system, women who are pregnant or within the peripartum period are at increased risk for development of SCAD [3]. In addition to female gender, the potential precipitating causes for SCAD include fibromuscular dysplasia, connective tissue disorder, systemic inflammatory disease, intense physical exertion, intense hormonal therapy with estrogen, progesterone, testosterone, or beta-human chorionic gonadotropin (HCG), and the use of steroids, cocaine, amphetamine, or metamphetamines [4]. Presently, there are no consensual recommendations available for the management of SCAD [1, 4]. Therefore, clinicians must exercise careful judgment to develop individualized treatment plan based on the clinical presentation and extent of the dissection [5]. Herein, we report a case of a 32-year-old man with an SCAD on left anterior descending artery. The discordance between clinical presentation and angiographic finding posed a unique challenge in therapeutic decision making. This case is unusual in that a young man presented with ACS due to SCAD in the absence of precipitating factors for SCAD.
| Case Report | ▴Top |
A 32-year-old man with obesity with body mass index (BMI) of 38.5, chronic migraine disorder, and mild intermittent asthma, presented with acute onset of a pressure-like sensation in the substernal area of his chest. This pain was constant, exertional, and non-radiating. Accompanying symptoms included exertional dyspnea, nausea, and non-bloody, non-biliary vomiting. Obesity and history of smoking (total 25 cigarettes in lifetime) were his only risk factors for coronary artery disease, as he was non-diabetic, non-hypertensive, and did not have family history of coronary artery disease. Only medication he was on at the time of admission was topiramate 50 mg twice daily for chronic migraine. His blood pressure was 138/80 mm Hg, heart rate was 90/min, respiration rate was 18/min, and oxygen saturation rate was 99% in room air. Electrocardiogram (ECG) revealed sinus rhythm with a PR elevation in the lead aVR, a PR depression in the lead II, as well as diffuse ST elevation. His serial troponin I over 4-h interval since admission was as the following: 1.97 ng/mL, 9.70 ng/mL, 14.39 ng/mL, 17.86 ng/mL, 21.33 ng/mL, 21.33 ng/mL, and 23.58 ng/mL. Urgent coronary angiogram showed a spontaneous dissection of the proximal left anterior descending artery with an intramural hematoma, causing a tubular stenosis of 80% (Fig. 1). Thrombolysis in myocardial infarction (TIMI) grade flow of the left anterior descending (LAD) was 3. Intraoperative ventriculogram demonstrated left ventricular ejection fraction (LVEF) of 45% with a diffuse hypokinesis. He was subsequently started on metoprolol 25 mg daily, lisinopril 2.5 mg daily, and dual antiplatelet therapy (DAPT) with aspirin 81 mg and clopidogrel 75 mg daily. He remained completely asymptomatic and hemodynamically stable. On the fourth day of hospitalization, he was discharged with arrangement for close monitoring on outpatient basis. About 1 week after the episode of SCAD, he returned with 3-h duration of “stabbing” pain in the epigastric area, associated with nausea and vomiting. Serial troponin I level with 2-h interval was slightly elevated as the following: 0.19 ng/L and 0.21 ng/L. ECG revealed sinus rhythm with ST elevation less than 1 mm in the anterolateral leads. Subsequently, the patient underwent a repeat cardiac catheterization, which revealed a reduction of the LAD stenosis from 80% to 20%. Intraoperative ventriculogram also showed an improvement of LVEF from 45% to 55%. Without any intervention, his chest pain resolved over a few hours.
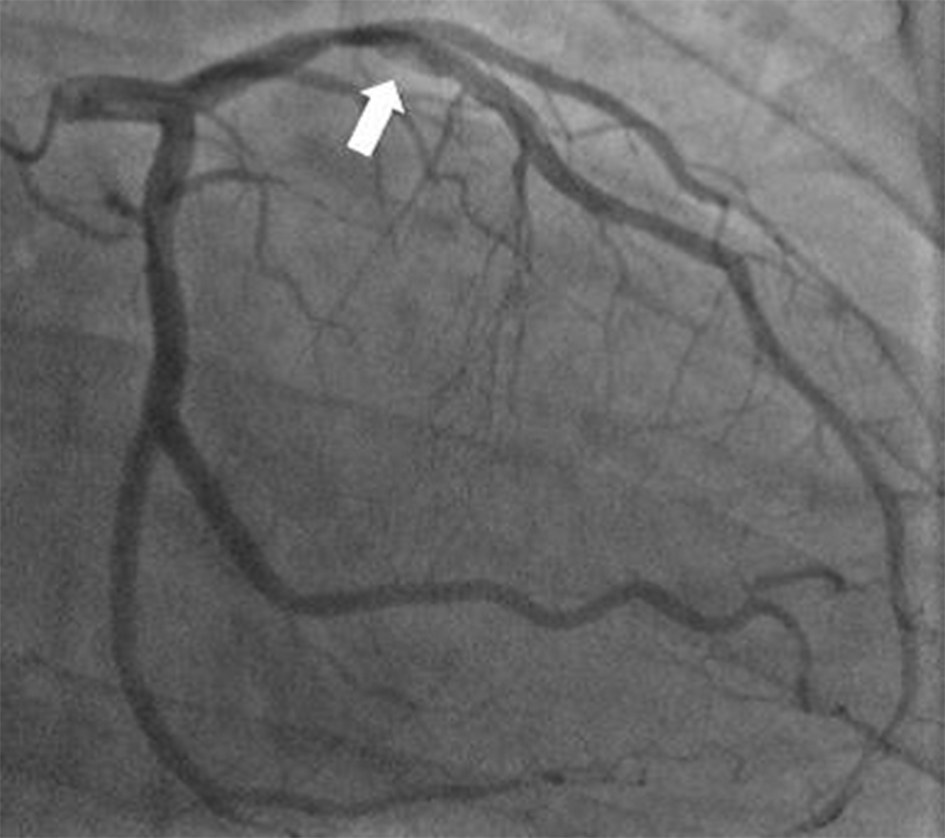 Click for large image | Figure 1. Coronary angiogram demonstrating a spontaneous dissection (arrow) of the proximal left anterior descending artery with an intramural hematoma, causing a tubular stenosis of 80%. |
At 6-month follow-up, the patient denied chest pain, shortness of breath, or palpitations. Computed tomography (CT) coronary angiography did not show any stenosis or vascular abnormality. CT visualized moderate left ventricular hypertrophy with LVEF of 50.9%.
| Discussion | ▴Top |
The present case of ACS due to SCAD in the absence of precipitating factors for SCAD posed a diagnostic challenge. In our patient, the coronary angiography provided excellent visualization of the dissected artery. However, in more than 70% of SCAD cases, the pathognomonic sign of multiple radiolucent lumens with contrast wall staining is absent [6]. Alternative imaging modalities, such as intravascular ultrasound (IVUS) and optical coherence tomography (OCT), can be used to confirm the diagnosis of SCAD. Due to its tremendous spatial resolution, OCT may be to visualize intramural hematoma, double lumen, and intimal flap on the arterial wall [7]. Furthermore, comprehensive visualization of coronary anatomy and pathology by OCT can guide therapeutic decision making process as it can measure the magnitude of luminal compromise and distribution of dissection flap. In patients with contraindication for iodinated contrast media, live CT imaging can be used to track the guidewires in angioplasty or IVUS can be utilized [7]. The discordance between clinical presentation and angiographic finding posed a unique challenge in therapeutic decision making. Unlike traumatic dissection of coronary arteries, more than half of SCAD heals spontaneously over time [2, 7]. Due to this substantial rate of spontaneous healing, conservative medical management is recommended for patients who are hemodynamically stable with a minor dissection. There is no consensual recommendation for medical therapy, but the following medications were reported to be effective in SCAD management: beta-blocker, aspirin, and clopidogrel [7]. Percutaneous coronary intervention (PCI) or coronary artery bypass graft (CABG) is reserved for hemodynamically unstable patients with SCAD in left main, circumflex, proximal left anterior descending artery, or right coronary artery [8]. Our patient presented with mild chest pain which resolved within 48 h from onset. He remained asymptomatic and hemodynamically stable. However, he had SCAD, resulting in an 80% stenosis of the LAD. His mild clinical presentation and TIMI grade flow 3 of the left anterior descending artery favored conservative management, but angiographic finding of severe stenosis appeared to warrant PCI. After careful consideration of individual risks and benefits, close observation with follow-up CT coronary angiography was chosen for this patient. Without dissection propagation, he remained without development of clinical symptoms. This case illustrates a rapid and complete healing of SCAD with medical intervention only. The intimal tear in SCAD establishes the pro-thrombotic milieu within the false lumen. The role of DAPT is to prevent thrombus formation in the false lumen and subsequent compression of true lumen. DAPT is typically continued until the angiographic evidence of healing is demonstrated or resolution of ischemic chest pain [9]. With empirical DAPT patient did not develop any thrombotic complication from SCAD. Recurrence rate of SCAD is reported as 10-30% [4, 9]. The median time for SCAD recurrence is 2.8 years with an interval of 3 days to 12 years [9]. Hypertension and the use of calcium channel blockers are notable risk factors for SCAD recurrence [2, 9]. Reported protective factor against SCAD recurrence was beta-blocker therapy [4, 9]. To prevent the recurrence of SCAD, our patient was promptly started on beta-blocker at the time of diagnosis. In light of a high frequency of recurrent SCAD events, the patients who have experienced SCAD should be closely followed for a potential recurrence. The etiology of coronary dissection in our patient is most likely coronary spasm, given his age and the history of smoking. The prevalence of coronary vasospasm in the patients withstand is known to be 0.9%. This unusual etiology makes our case to be exceedingly rare [10].
Conclusions
From this case, it is evident that the underlying pathological process in SCAD can be more severe when compared to its clinical presentation. So it is advisable for physicians to take caution when treating these patients. Risk stratification with TIMI score and utilization of initial diagnostic workups like ECG, cardiac enzymes (troponin) and adjunct studies like coronary angiography can help guide management and decision making. Other imaging modalities that can be employed in the case of existing contraindications to iodine contrast include IVUS. OCT can be used in the case of inconclusive coronary angiography. With regards to management, medical therapy with dual antiplatelet medications (aspirin and clopidogrel) can be used to prevent thrombus formation within the false lumen, which can further worsen the situation by decreasing or completely occluding blood delivery to the myocardial tissue. Beta-blockers have also been reported to be cardioprotective against SCAD recurrence. The patient’s blood pressure should be adequately controlled to avert further recurrence or worsening of current symptoms. However, teratogenic antihypertensive such as lisinopril should be avoided in patients affected during pregnancy. In recalcitrant cases or cases with severe hemodynamic instability, and severe occlusion of major coronary vessels, PCI with stent placement or CABG can be used to stop further damage to the myocardial tissue and regain cardiac function. It is pertinent to note that some young patients with minimal to no cardiovascular risk factors may present with SCAD as in this case.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
We obtained consent from the patient for this case study.
Author Contributions
SP wrote the initial manuscript. EA and AP revised the manuscript. All authors fulfilled the requirements to be listed as authors and approve of the submission of this manuscript for publication.
Data Availability
The authors declare that data supporting the findings of this study are available within the article. For further inquiries, you may reach out to the corresponding author.
Abbreviations
SCAD: spontaneous coronary artery dissection; ECG: electrocardiogram; DAPT: dual antiplatelet therapy; IVUS: intravascular ultrasound; OCT: optical coherence tomography; CABG: coronary artery bypass graft; TIMI: thrombolysis in myocardial infarction; ACS: acute coronary syndrome; HCG: human chorionic gonadotropin; BMI: body mass index; LAD: left anterior descending; LVEF: ventricular ejection fraction; CT: computed tomography; PCI: percutaneous coronary intervention
| References | ▴Top |
- Tweet MS, Eleid MF, Best PJ, Lennon RJ, Lerman A, Rihal CS, Holmes DR, Jr., et al. Spontaneous coronary artery dissection: revascularization versus conservative therapy. Circ Cardiovasc Interv. 2014;7(6):777-786.
doi pubmed - Al Emam AR, Almomani A, Gilani SA, Khalife WI. Spontaneous coronary artery dissection: one disease, variable presentations, and different management approaches. Int J Angiol. 2016;25(3):139-147.
doi pubmed - Papireddy MR, Nandish S, Mishkel GJ. Recurrent spontaneous coronary artery dissection: First case report in men with three episodes of spontaneous coronary dissection in separate vascular territories. Catheter Cardiovasc Interv. 2016;87(5):E192-196.
doi pubmed - Saw J, Mancini GBJ, Humphries KH. Contemporary review on spontaneous coronary artery dissection. J Am Coll Cardiol. 2016;68(3):297-312.
doi pubmed - Dakik HA, Nader GA, Arja WA, Sawaya J, Gharzuddine W. Asymptomatic spontaneous coronary artery dissection. Clin Cardiol. 2010;33(7):E40-42.
doi pubmed - Saw J, Aymong E, Sedlak T, Buller CE, Starovoytov A, Ricci D, Robinson S, et al. Spontaneous coronary artery dissection: association with predisposing arteriopathies and precipitating stressors and cardiovascular outcomes. Circ Cardiovasc Interv. 2014;7(5):645-655.
doi pubmed - Lim C, Banning A, Channon K. Optical coherence tomography in the diagnosis and treatment of spontaneous coronary artery dissection. J Invasive Cardiol. 2010;22(11):559-560.
- Saw J. Spontaneous coronary artery dissection. Can J Cardiol. 2013;29(9):1027-1033.
doi pubmed - Gilhofer TS, Saw J. Spontaneous coronary artery dissection: a review of complications and management strategies. Expert Rev Cardiovasc Ther. 2019;17(4):275-291.
doi pubmed - White Solaru K, Heupler F, Cho L, Kim ESH. Prevalence of coronary vasospasm using coronary reactivity testing in patients with spontaneous coronary artery dissection. Am J Cardiol. 2019;123(11):1812-1815.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


