| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 10, Number 7, July 2019, pages 203-205
An Uncommon Silent Strategic Left Middle Cerebral Artery Infarction
Permphan Dharmasaroja
Department of Anatomy, Faculty of Science, Mahidol University, Rama VI Road, Ratchathewi, Bangkok 10400, Thailand
Manuscript submitted July 1, 2019, accepted July 15, 2019
Short title: An Uncommon Silent Strategic Infarction
doi: https://doi.org/10.14740/jmc3328
| Abstract | ▴Top |
Impairment of memory retrieval is not the major presenting symptoms of vascular cognitive impairment (VCI), which can result from silent strokes occurring in uncommon vascular territories, and can be detected only on neuroimaging or neuropathology. The neuroanatomical substrate for VCI remains unclear. This report presents an uncommon location of silent strategic infarction resulting in an insidious onset and gradual progression of the cognitive decline without overt sensorimotor deficits.
Keywords: Vascular cognitive impairment; Stroke; Middle cerebral artery; Magnetic resonance imaging
| Introduction | ▴Top |
Evidence has shown that the cognitive impairment by subcortical lacunes and white matter lesions is most apparent in the dorsolateral frontal cortex (DFC) [1], and impairment of memory retrieval is usually associated with defects of the hippocampal-parieto-frontal network. Vascular cognitive impairment (VCI) can occur without recent stroke in which cognitive impairment is the result of covert vascular brain injury detected only on neuroimaging or neuropathology [2]. The silent strategic infarction in the territory of the inferior M2 branch of the left middle cerebral artery (MCA) is uncommon, which can result in isolated cognitive impairment without apparent sensorimotor symptoms.
| Case Report | ▴Top |
A 73-year-old priest presented with a rapid onset of difficulty in recalling of chanting lyrics. Two weeks prior, during a religious ceremony he became aware that he could not recall the chanting lyrics. Progressively, he had difficulty in recalling recent conversations. When reading, he found it hard to read the words in the sentences. However, he could remember the names of his colleagues, was able to use the phone, and could adequately perform his personal daily activities. He had a history of diabetes mellitus, hyperlipidemia, and essential hypertension.
At examination, he was afebrile, and his blood pressure was 111/58 mm Hg, with a pulse rate of 58 beats per minute (bpm). He was oriented with fluent speech. His cranial nerve functions were normal. There were nosensory and motor deficits; however, his Babinski sign was positive on the right. The Montreal Cognitive Assessment (MoCA) revealed prominent impairment in attention (digit span and serial seven subtractions), language (sentence repetition and letter fluency), and delayed recall. Alexia, agraphia, and apraxia were absent. Laboratory tests revealed high blood sugar of 242 mg/dL. Blood cell counts and other blood chemistry were normal, including thyroidfunction test and syphilitic screening.
Brain magnetic resonance imaging (MRI), performed 2 weeks after onset, revealed a hyperintense fluid-attenuated inversion recovery (FLAIR) lesion without restricted diffusion on diffusion weighted image (DWI) in the deep white matter of the left parietal and temporal lobes and left external capsule, suggestive of gliotic changes from an old insult, especially old infarction in the left MCA territory (Fig. 1). Brain magnetic resonance angiography (MRA) showed occlusion or very severe stenosis at the inferior M2 branch of the left MCA, with loss of its distal flow related enhancement (Fig. 2). Irregularity of the M2 segment of the right MCA and bilateral posterior cerebral arteries was noted, while the remaining of the intracranial arteries was unremarkable.
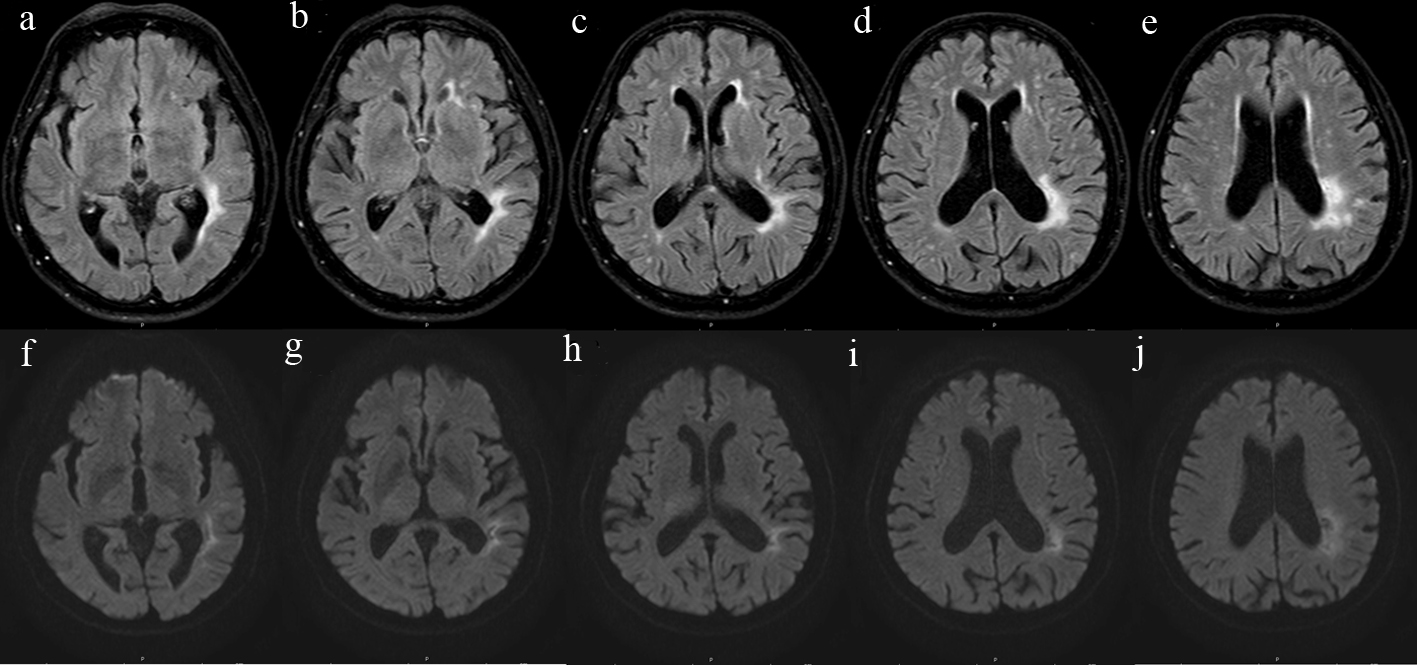 Click for large image | Figure 1. Brain MRI showing a hyperintense FLAIR lesion (a-e) without restricted diffusion on DWI (f-j) in the white matter of the left parietal and temporal lobes, and left external capsule, which could damage the left IFOF and ILF. FLAIR: fluid-attenuated inversion recovery; IFOF: inferior fronto-occipital fasciculus; ILF: inferior longitudinal fasciculus. |
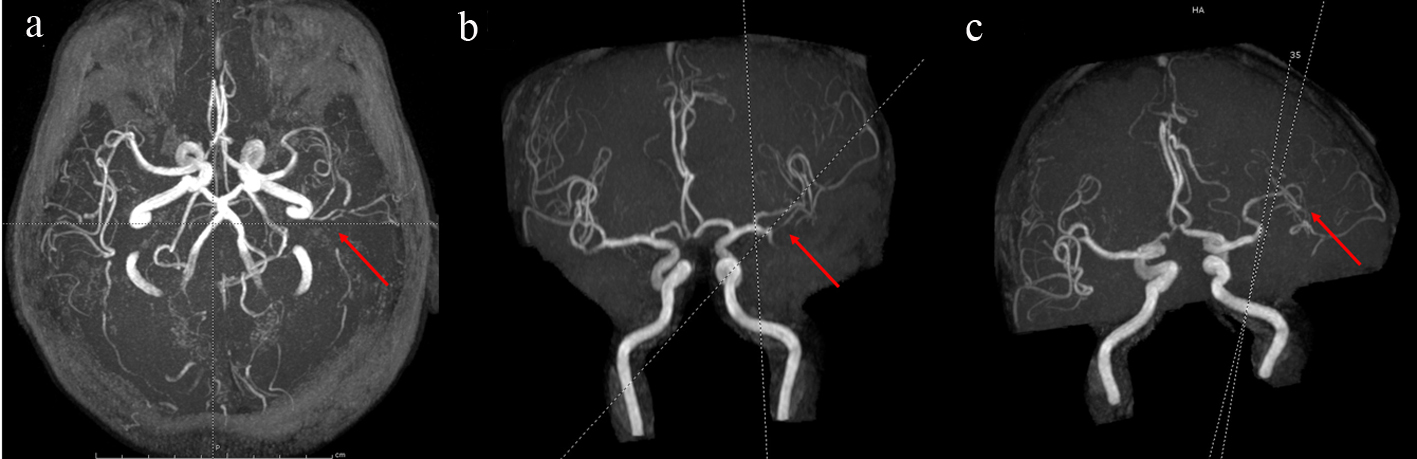 Click for large image | Figure 2. Brain MRA showing occlusion or very severe stenosis at the inferior M2 branch of the left MCA (a-c). MCA: middle cerebral artery. |
The patient was diagnosed with vascular cognitive impairment or VCI and was prescribed 325 mg aspirin. Hyperglycemia was initially managed with subcutaneous insulin injection for 48 h to maintain the blood glucose at about 160 - 180 mg/dL. The patient was then given metformin, and was discharged on the fifth day after admission. The cognitive examination result remained the same as at admission. A follow-up at 4 weeks after discharge did not show progression of the cognitive functions and sensorimotor deficits.
| Discussion | ▴Top |
Impairment of memory retrieval is usually associated with defects of the hippocampal-parieto-frontal network, but it is not the major presenting symptom in patients with VCI. Typically, patients are diagnosed with VCI after single or multiple clinical strokes. VCI consists of two main clinical syndromes: post-stroke VCI in which cognitive impairment is the immediate consequence of a recent stroke, and VCI without recent stroke in which cognitive impairment is the result of covert vascular brain injury detected only on neuroimaging or neuropathology. The latter, which developed without recent clinical symptoms of stroke, was relevant to this patient.
Brain CT and MRI in VCI patients usually reveal evidence of large multiple infarcts, infarcts in specific vascular territories including the angular gyrus, basal forebrain, anterior cerebral artery or posterior cerebral artery, multiple basal ganglia lacunes, or white matter lacunes, and extensive periventricular white matter lesions [3]. Evidence has shown that the cognitive impairment by subcortical lacunes and white matter lesions is most apparent in the DFC [2]; however, the neuroanatomical substrate for cognitive dysfunction is complex and remains unclear. Excluding large multiple infarcts and extensive periventricular white matter lesions, lesions causing cognitive and memory impairments in VCI typically involve infarcts in specific vascular distributions. These include a single strategically placed infarct in the angular gyrus, basal forebrain, multiple basal ganglia lacunes, or white matter lacunes, as well as territories of anterior and posterior cerebral arteries [2]. In this patient, the major lesion is located deep in the subcortical area of the left temporo-parietal lobe, with sparing the angular gyrus. The lesion in the patient could mostly affect the inferior fronto-occipital fasciculus (IFOF) and inferior longitudinal fasciculus (ILF) [4]. The IFOF connects the occipital cortex, temporo-basal areas, and superior parietal lobe to the frontal lobe. The fiber bundle of the ILF was defined as a direct connection from the occipital lobe to the anterior part of the temporal lobe, running laterally and inferiorly above the optic radiation fibers, while the IFOF runs medially and above the optic pathways and spatially overlaps with the ILF along some pathway lengths [5-7]. However, a detailed anatomical definition of the IFOF and ILF, and their exact functional roles are still under debate.
The lesion is correspondent to the territory of the inferior M2 branch of the left MCA (Fig. 2). This location is uncommon for silent strategic infarction [8]. The present case report indicates that damages in the left deep parietotemporal white matter could result in an insidious onset and gradual progression of the cognitive functions without overt sensorimotor deficits, but can be detected only on neuroimaging. Careful neurological examination may assist in locating lateralizing signs such as the unilateral Babinski sign, and involvement of the IFOF and ILF can be confirmed by tractography.
Epidemiological studies have shown that patients with silent brain infarction have a higher risk of future stroke. Although the effectiveness of aspirin to prevent stroke has not been studied in this setting [9], a recent prospectively multicenter clinical trial has shown that silent cerebral infarction seems to be a negative prognostic factor and low-dose aspirin treatment might improve the prognosis [10]. Therefore, it seems appropriate to apply secondary stroke prevention strategies to silent stroke patients with modifiable risk factors for atherosclerosis.
Acknowledgments
The patient has been treated at Phyathai 1 Hospital, Bangkok, Thailand.
Financial Disclosure
None to declare.
Conflict of Interest
The author declares no conflict of interest.
Informed Consent
Not applicable.
Author Contributions
PD was involved in patient care and writing the manuscript.
| References | ▴Top |
- Reed BR, Eberling JL, Mungas D, Weiner M, Kramer JH, Jagust WJ. Effects of white matter lesions and lacunes on cortical function. Arch Neurol. 2004;61(10):1545-1550.
doi pubmed - Roman GC, Tatemichi TK, Erkinjuntti T, Cummings JL, Masdeu JC, Garcia JH, Amaducci L, et al. Vascular dementia: diagnostic criteria for research studies. Report of the NINDS-AIREN International Workshop. Neurology. 1993;43(2):250-260.
doi pubmed - Lopez OL, Kuller LH, Becker JT, Jagust WJ, DeKosky ST, Fitzpatrick A, Breitner J, et al. Classification of vascular dementia in the Cardiovascular Health Study Cognition Study. Neurology. 2005;64(9):1539-1547.
doi pubmed - Wakana S, Jiang H, Nagae-Poetscher LM, van Zijl PC, Mori S. Fiber tract-based atlas of human white matter anatomy. Radiology. 2004;230(1):77-87.
doi pubmed - Catani M, Thiebaut de Schotten M. A diffusion tensor imaging tractography atlas for virtual in vivo dissections. Cortex. 2008;44(8):1105-1132.
doi pubmed - Wahl M, Li YO, Ng J, Lahue SC, Cooper SR, Sherr EH, Mukherjee P. Microstructural correlations of white matter tracts in the human brain. Neuroimage. 2010;51(2):531-541.
doi pubmed - Ortibus E, Verhoeven J, Sunaert S, Casteels I, de Cock P, Lagae L. Integrity of the inferior longitudinal fasciculus and impaired object recognition in children: a diffusion tensor imaging study. Dev Med Child Neurol. 2012;54(1):38-43.
doi pubmed - Min WK, Park KK, Kim YS, Park HC, Kim JY, Park SP, Suh CK. Atherothrombotic middle cerebral artery territory infarction: topographic diversity with common occurrence of concomitant small cortical and subcortical infarcts. Stroke. 2000;31(9):2055-2061.
doi pubmed - Smith EE, Saposnik G, Biessels GJ, Doubal FN, Fornage M, Gorelick PB, Greenberg SM, et al. Prevention of stroke in patients with silent cerebrovascular disease: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2017;48(2):e44-e71.
doi - Maestrini I, Altieri M, Di Clemente L, Vicenzini E, Pantano P, Raz E, Silvestrini M, et al. Longitudinal study on low-dose aspirin versus placebo administration in silent brain infarcts: the silence study. Stroke Res Treat. 2018;2018:7532403.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


