| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 10, Number 3, March 2019, pages 67-71
Epidermoid Intramedullary Cyst: A Rare Case Report
Antigona Kabashia, Ilir Ahmetgjekaja, Kreshnike Dedushia, b, Serbeze Kabashia, b, c, Jeton Shatria, b
aClinic of Radiology, Diagnostic Centre, UCCK, Prishtina 10000, Kosovo
bFaculty of Medicine, University of Prishtina, Prishtina 10000, Kosovo
cCorresponding Author: Serbeze Kabashi, Faculty of Medicine, University of Prishtina, Prishtina 10000, Kosovo
Manuscript submitted November 30, 2018, accepted January 25, 2019
Short title: Epidermoid Intramedullary Cyst
doi: https://doi.org/10.14740/jmc3224
| Abstract | ▴Top |
Epidermoid cysts are tumors that ocur in most parts of the body and are often treated by neurosurgeons, but intramedullary localizations of epidermoid cysts are very rare. The incidence in adults is lower than 1% and in children lower than 3%.We report a case of a 27-year-old patient presenting with thoracic spinal cord compression syndrome (T11-12). The magnetic resonance imaging (MRI) showed an intramedullary cystic mass. It demonstrated low signal intensity on T1-weighted sequence and high signal intensity on T2-weighted sequences, with minimal peripheral enhancement following intravenous administration of gadoteric acid. After surgical removal of the tumor, the pathology confirmed the radiological diagnosis of spinal epidermoid cyst. MRI reduces the delay in diagnosis of spinal cord tumors but should be guided by clinical judgment.
Keywords: Epidermoid cyst; Spinal cord cyst; Spinal cord; Magnetic resonance imaging
| Inroduction | ▴Top |
Epidermoid cysts are a frequently occurring subgroup of congenital tumors. In a series of adult patients, cranial site involvement outweighed the spinal sites by 14:1. Intraspinal epidermoid cysts represent less than 1% of all intraspinal tumors in adults [1].
In children, the incidence is higher. However, most intraspinal epidermoid cysts are subdural and extramedullary, and they are rarely found within the spinal cord. We review the literature regarding intramedullary epidermoid cysts and present the case of a child with an intramedullary epidermoid cyst in the thoracic region that was evaluated by magnetic resonance imaging (MRI).
The vast majority of spinal epidermoid cysts are localized at subdural and extramedullary spaces. Thoracic region is the favorite site of the intramedullary epidermoid cysts and the lumbar region is the next common area [2].
The differential diagnosis depends on the signal intensity of cyst content and the enhancement pattern of cyst wall. However, because of the similar imaging features, it is not easy to distinguish this pathology among other entities that are usually encountered in differential diagnosis during MRI examinations (epidermoid cyst, dermoid cyst, ventriculus terminalis and arachnoid cyst).
In conclusion, epidermoid cysts should be included in the differential diagnosis when an intramedullary cystic mass with the abovementioned MRI features is detected within the spinal canal.
| Case Report | ▴Top |
A 27-year-old woman developed progressive difficulty in walking associated with stiffness and paresthesia during 3 months. There was no history of trauma or any mediacal procedure on the spine. Clinical (neurological) examination revealed spastic paraparesis with the grade 1 muscle power (Medical Research Council grading scale) on both lower limbs. Sensory examination revealed loss of all sensation below T11-L1 segments. Sacral dermatomal sensations were preserved. Deep tendon reflexes decreased in both lower limbs. MRI study of the thoracic and lumbar spine was performed. An intramedullary cystic mass measuring 16 mm (transverse plane) and 66 mm (cranio-caudal diameter) at the T11-L1 levels was found. The lesion was hypointense on T1-weighted sequence (Fig. 1a) and hyperintense on T2-weighted sequence. Turbo inversion recovery magnitude (TIRM) sequence, T2 fat sat and T1 fat sat (Fig. 1b-d and Fig. 2a-c) show minimal peripheral enhancement following intravenous administration of gadoteric acid (Fig. 3). The patient underwent T11-L1 laminectomy with removal of the tumor. The slices obtained during histopathology examination showed a fibrous wall lined with stratified cerotic epithelium surrounding a cyst, consistent with an intramedullary epidermoid cyst (Fig. 4). After surgical removal of the tumor, the pathology diagnosis confirmed the MRI diagnosis of spinal epidermoid cyst. Figure 5 shows T2-weighted sagital sequence (segments T11-L1) after surgical removal of the tumor (Fig. 5a), T1 fat sat sagital sequence (segments T11-L1) after surgical removal of the tumor (Fig. 5b), T1 fat sat coronal sequence (segments T11-L1) (Fig. 5c), and T1 fat sat transversal sequence after administration of intravenous contrast (segments T11-L1) and after surgical removal of the tumor (Fig. 5d).
 Click for large image | Figure 1. (a) T1-weighted sagital sequence (T11-L1 segments show hypointense, heterogeneous signal). (b) T2-weighted sagital sequence. (c) T2 TIRM sagital sequence. (d) T1/fat sat sagital sequence (T11-L1 segments show hyper intense signal). |
 Click for large image | Figure 2. (a) T2-weighted axial sequence (segment T11). (b) T2-weighted axial sequence (segment T12). (c) T2- weighted axial sequence (segment T12/L1). |
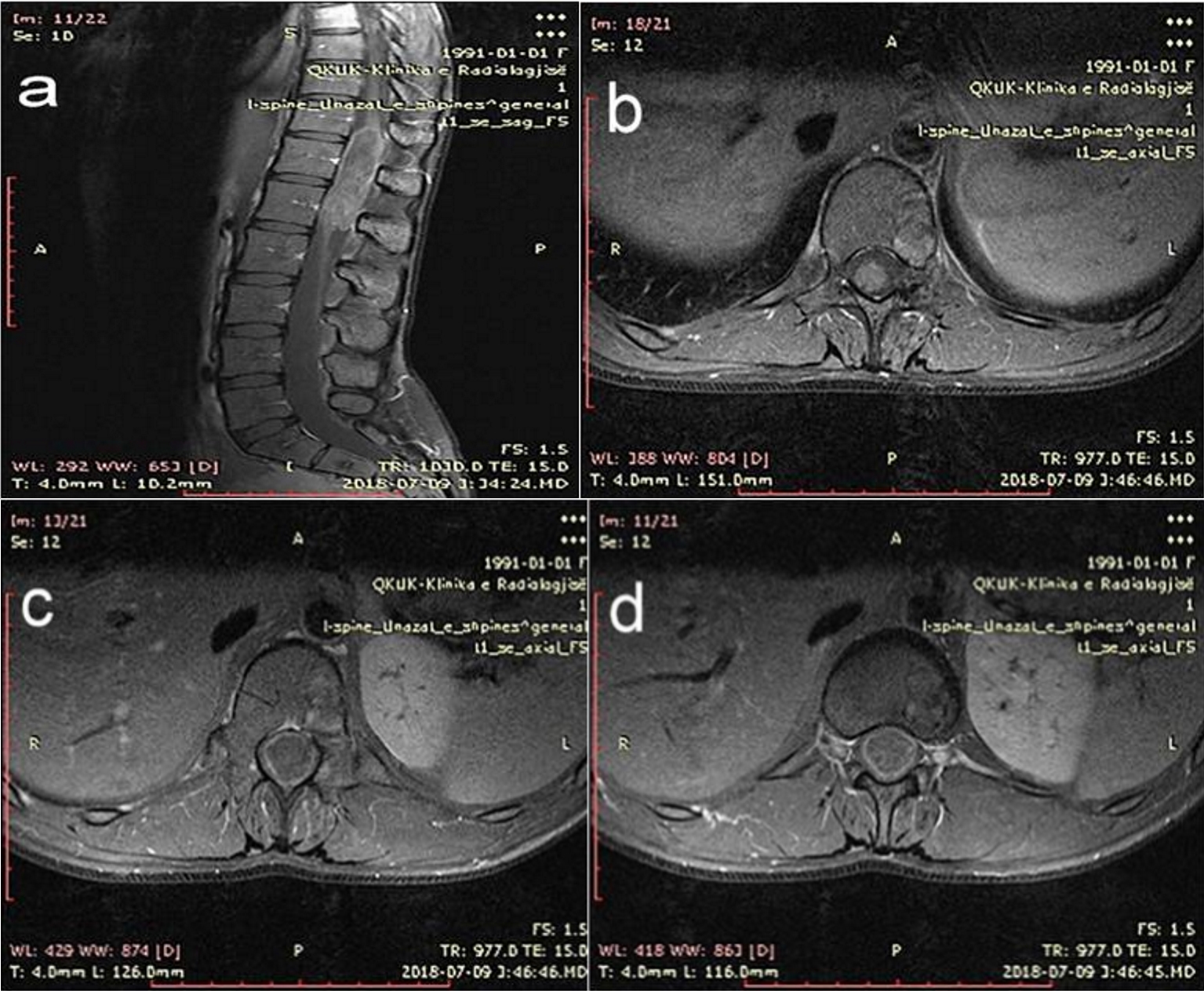 Click for large image | Figure 3. (a) T1 fat sat sagital sequence. (b-d) T1 fat sat axial sequence (after administration of intravenous contrast gadoteric acid). The lesion shows minimal peripheral enhancement. |
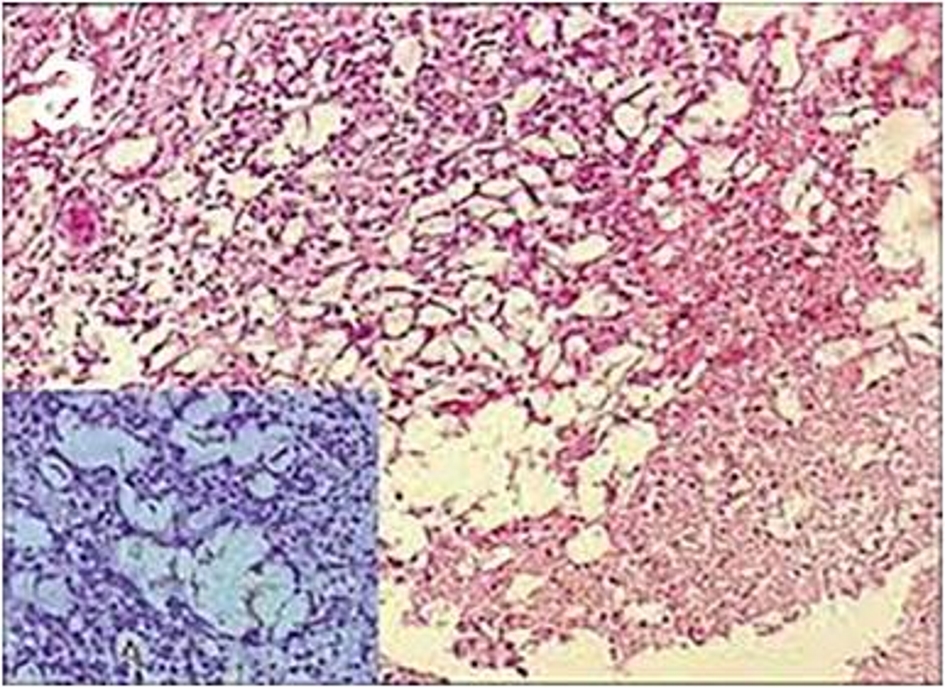 Click for large image | Figure 4. Histopathology image analysis shows keratin material characteristic for epidermoid cyst. |
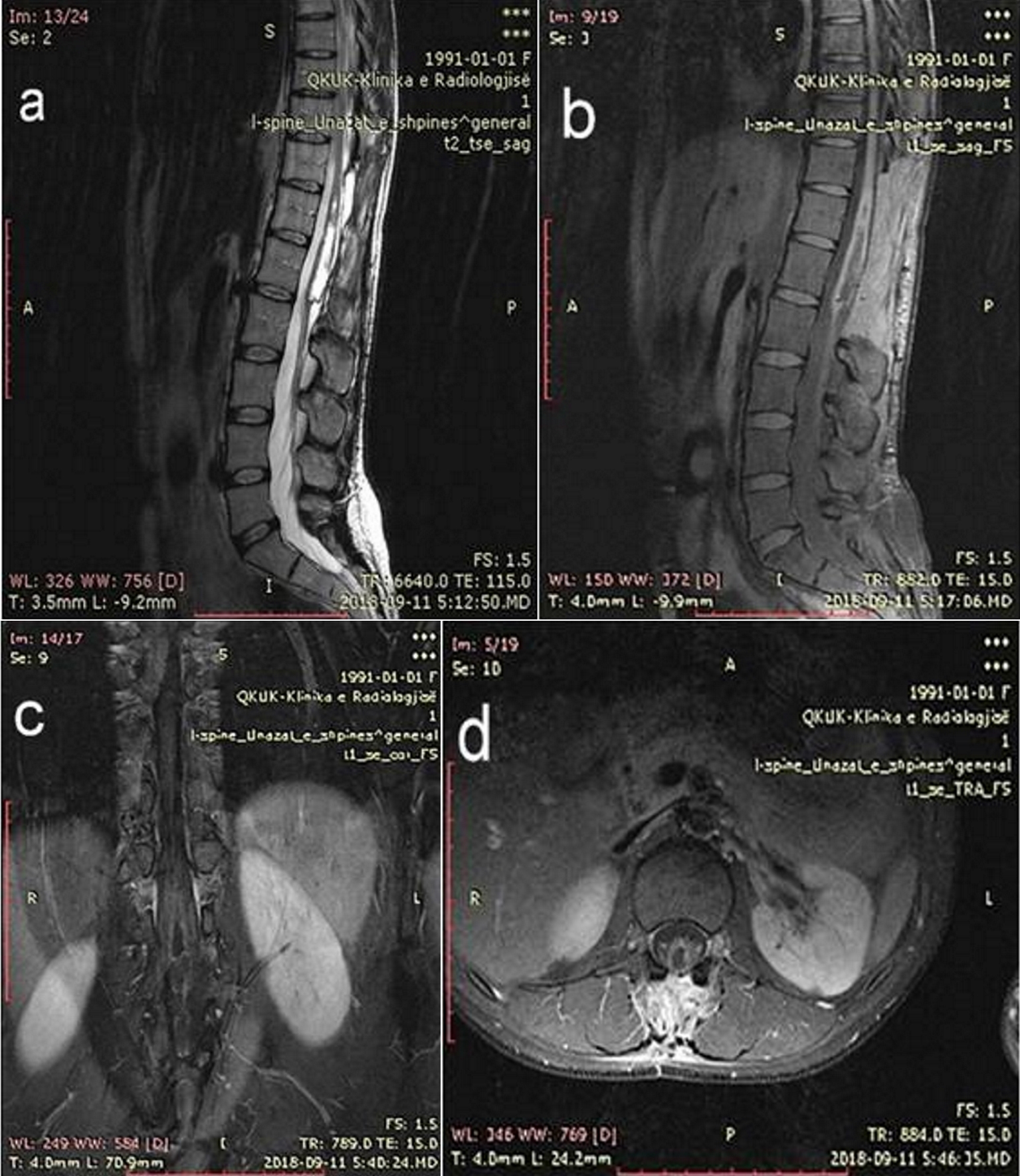 Click for large image | Figure 5. (a) T2-weighted sagital sequence. (b) T1- Fat Sat sagital sequence. (c) T1 fat sat coronal sequence. (d)T1 fat sat transversal sequence after administration of intravenous contrast (segments T11-L1). The MRI examination was undertaken after surgical removal of the tumor. |
| Discussion | ▴Top |
Intramedullary epidermoid cysts with localization in the spinal cord are rare. They are slow-growing benign tumors, and represent less than 1% of all intraspinal tumors. Epidermoid cysts most commonly occur in the third to fourth decade, and predominantly in men [1].
The vast majority of epidermoid cysts are localized at subdural and extramedullary spaces. Thoracic region is the most favorite site of intramedullary epidermoid cysts and the lumbar region is the next common area of occurence [2].
Histologically, epidermoid cysts have a fibrous wall lined with stratified squamous epithelium surrounding a cyst containing waxy squames [3]. It can be either congenital or acquired.
As for the epidemiology, the incidence of the epiderrnoid cysts among other intracranial tumors in most of the large series of cases is estimated to be from 0.2% to 1%; in the spinal canal, the incidence is even lower [4].
Halcrow et al reported a series of 90 intraspinal epidermoid cysts collected from the literature, with 39 being acquired and 51 being congenital. Acquired epidermoid cysts have been found years after single or multiple lumbar spinal punctures and are thought to result from iatrogenic penetration of skin fragments [5, 6]. It is generally believed that congenital epidermoid cysts originate from displaced ectoderm inclusions arising in early fetal life and may be associated with defective closure of the dural tube [7, 8]. In our case, the patient denied the history of trauma or puncture. Also, it is unreasonable to puncture at so high level during usual medical procedures. The old age of symptom onset is less possible for a congenital lesion, except for a very slow-growing lesion. Finally, we have supposed that our case was caused either by a congenital lesion with an extraordinary slow-growing pattern or by subtle trauma event with unaware puncture of the cord. Intramedullary epidermoid cysts showed hypointensity on T1-weighted sequence and hyperintensity on T2-weighted sequence. The margins of the lesions had an irregular or a shaggy appearance possibly because of chronic inflammatory response to the squamous tissue leak through the capsule and variable gliosis along the margin [2]. The inner structure of the intramedullary epidermoid cyst was heterogenous with a high-intensity portion on T2-weighted images. Intravenous injection of gadoteric acid demonstrated peripheral enhancement on T1-weighted images. The acquired cauda equina epidermoid cyst, which is isointense on T1-weighted images and hyperintense on T2-weighted images, reveales faint peripheral enhancement in the post-contrast images [9]. Generally, on MRI examination, the epidermoid cysts have heterogeneous hypointense signal on T1-weighted images and hyperintense signal intensity on T2-weighted images with no contrast enhancement or minimal peripheral enhancement following intravenous gadolinium administration (in our case, the periferal enhancement was stronger than usual). The differential diagnosis depends on the signal intensity of the content of the cyst and the enhancement pattern of cyst’s wall. However, because of the similar imaging features, it is not easy to make differential diagnosis between epidermoid cyst, dermoid cyst, ventriculus terminalis and arachnoid cyst on MRI examnination. Dermoid cysts contain mature tissues of ectoderm with predominance of fatty components, characterized by heterogeneous hyperintensity on all sequences [10]. The high signal intensity on T1-weighted images makes the diagnosis easier as a result of the fatty content of the tumor [11]. The ventriculus terminalis, also known as the fifth ventricle [12], is a small ependyma-lined cavity in the conus medullaris, and it is usually in continuity with the central canal of the rostral spinal cord [13]. The ventriculus terminalis is ovoid, smooth-walled and has no internal septum. The intracystic fluid follows the signals of cerebrospinal fluid (CSF), characterized by low signal on T1-weighted and high signal on T2-weighted sequences. In the eight (72.7%) of 11 cases the contrast gadoteric acid was administered intravanously.
Epidermoid cysts are generally characterized on MRI images by an important variability of signal intensity among different cases and, sometimes, between the different parts of the same cyst; other features include the absence of edema in surrounding tissue, well-defined limits, and the presence of calcifications [14].
Conclusions
Epidermoid cysts should be included in the differential diagnosis when encountering an intramedullary cystic mass with the abovementioned MRI features.
Complete microsurgical excision is the treatment of choice and complete excision or near total excision of this benign tumor can cure the patient with the expectation of normal life.
Conflict of Interest
The authors have no conflict of interest to declare.
| References | ▴Top |
- Penisson-Besnier I, Guy G, Gandon Y. Intramedullary epidermoid cyst evaluated by computed tomographic scan and magnetic resonance imaging: case report. Neurosurgery. 1989;25(6):955-959.
doi pubmed - Chandra PS, Manjari T, Devi BI, Chandramouli BA, Srikanth SG, Shankar SK. Intramedullary spinal epidermoid cyst. Neurol India. 2000;48(1):75-77.
pubmed - Sternberg SS. Epidermoid cyst. In: Antonioli DA, Carter D, Mills SE, Oberman HA, ed. Diagnostic surgical pathology 2nd edition. New York Hong Kong: Raven Press 1994: p. 473-474.
- Hakyemez B, Aksoy U, Yildiz H, Ergin N. Intracranial epidermoid cysts: diffusion-weighted, FLAIR and conventional MR findings. Eur J Radiol. 2005;54(2):214-220.
doi pubmed - Halcrow SJ, Crawford PJ, Craft AW. Epidermoid spinal cord tumour after lumbar puncture. Arch Dis Child. 1985;60(10):978-979.
doi pubmed - Shaywitz BA. Epidermoid spinal cord tumors and previous lumbar punctures. J Pediatr. 1972;80(4):638-640.
doi - Netsky MG. Epidermoid tumors. Review of the literature. Surg Neurol. 1988;29(6):477-483.
doi - Roux A, Mercier C, Larbrisseau A, Dube LJ, Dupuis C, Del Carpio R. Intramedullary epidermoid cysts of the spinal cord. Case report. J Neurosurg. 1992;76(3):528-533.
doi pubmed - Kachhara R, Unnikrishnan M. Acquired cauda equina epidermoid cyst. Neurol India. 1999;47(3):250.
pubmed - Gupta S, Gupta RK, Gujral RB, Mittal P, Kuriyal M, Krishnani N. Signal intensity patterns in intraspinal dermoids and epidermoids on MR imaging. Clin Radiol. 1993;48(6):405-413.
doi - Newton DR, Larson TC III, Dillon WP, Newton TH. Magnetic resonance characteristics of cranial epidermoid and teratomatous tumors. AJNR. 1987;8:945-945.
- Kernohan JW. The ventriculus terminalis: its growth and development. J Comp Neurol. 1924;38:10-125.
doi - Vion-Dury J, Vincentelli F, Jiddane M, Van Bunnen Y, Rumeau C, Grisoli F, Salamon G. MR imaging of epidermoid cysts. Neuroradiology. 1987;29(4):333-338.
doi pubmed - Robert IG, David MY. Congenital disorders of the brain and spine. Neuroradiology: the requisites, 2nd edition. USA: Mosby. 2003: p. 413-416.
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


