| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 9, Number 12, December 2018, pages 386-389
An Unusual Trigger for Stress Cardiomyopathy
Sowjanya Yenigallaa, b, Navneet Kaura
aDepartment of Medicine, University of Pittsburgh Medical Center Mercy Hospital, Pittsburgh, PA, USA
bCorresponding Author: Sowjanya Yenigalla, Department of Medicine, UPMC Mercy, 1400 Locust Street, Pittsburgh, PA 15219, USA
Manuscript submitted September 18, 2018, accepted November 6, 2018
Short title: An Unusual Trigger for Stress Cardiomyopathy
doi: https://doi.org/10.14740/jmc3132w
| Abstract | ▴Top |
Our patient is a 65-year-old male with a history of hypertension, hyperlipidemia, diabetes mellitus, alcohol abuse and paroxysmal atrial fibrillation, who presented to the emergency department with epigastric pain. On laboratory examination, his sodium level was found to be 127 meq/L (normal range: 136 - 145 meq/L). During his hospital course, he developed retrosternal chest pain. His electrocardiogram (ECG) during this episode showed deep symmetrical T wave inversions in the anterior, septal and apical leads. His symptoms of chest pain and ECG changes prompted a cardiac catheterization, which revealed, non-obstructive coronary disease with left ventriculogram significant for apical near akinesis and preserved basal wall motion, characteristic findings of Takotsubo cardiomyopathy, with an estimated left ventricle ejection fraction of 35-40%.
Keywords: Takotsubo cardiomyopathy; Hyponatremia; Sodium correction; Alcohol withdrawal
| Introduction | ▴Top |
Takotsubo syndrome, also known as stress cardiomyopathy or apical ballooning syndrome, is a transient decrease in left ventricular function, reported in 1-2% of patients presenting with symptoms similar to acute coronary syndrome [1]. Risk factors can include emotional or physical stressors, such as asthma exacerbations, major surgery, stroke and more rarely, electrolyte disturbances leading to an increase in catecholamine production.
| Case Report | ▴Top |
A 65-year-old male with a history of hypertension, hyperlipidemia, diabetes mellitus, alcohol abuse and paroxysmal atrial fibrillation presented to the emergency room with complaints of epigastric pain, nausea, vomiting and decrease in appetite for 5 days. He was initially placed in the clinical decision unit (CDU) overnight for rehydration with intravenous fluids. He reported drinking one pint of vodka daily with his last drink being about 2 days prior to his emergency department visit. On initial presentation, he was found to be in sinus tachycardia. While overnight in the CDU, his cardiac telemetry monitor had an episode of rapid paroxysmal atrial fibrillation. This prompted an admission to the general medicine floor for further management of his rapid atrial fibrillation, as well as epigastric pain.
His vital signs on arrival to the emergency department were significant for sinus tachycardia to 112 beats/min, blood pressure of 175/105 mm Hg, respiratory rate of 18 breaths/min and oxygen saturation of 96% on ambient air.
Physical examination on arriving to the medical floor showed an anxious appearing Caucasian male with poor physical hygiene. His cardiovascular examination showed an irregular rhythm without any murmurs. His breathing was non-labored with normal vesicular breath sounds in all lung fields. His abdomen was tender in the epigastric region without distension, guarding or rigidity. He had normal bowel sounds on auscultation. His alcohol withdrawal assessment score ranged from 0 to 12.
Investigations
His laboratory examinations were pertinent for hyponatremia to 127 meq/L, elevated alanine aminotransferase (ALT) and aspartate aminotransferase (AST) to 124 and 127 U/L, respectively. Lipase level was within normal limits. Troponin level on the day of presentation was within normal limits. After his episode of chest pain on day 5, troponin level was found to be elevated and peaked at 0.11. Computed tomography (CT) of abdomen and pelvis with contrast showed no abnormalities. As mentioned earlier, his electrocardiogram (ECG) on admission showed sinus tachycardia with ventricular rate of 112 beats/min. A few hours after being in the CDU, his cardiac telemetry had alarmed for atrial fibrillation with rapid ventricular rates. An echocardiogram was performed on day 2 for evaluation of his atrial fibrillation with rapid ventricular rates, and showed a normal left ventricular size and function with ejection fraction of 60-65%. The right ventricular size and function were normal. Systolic pressure of pulmonary artery was estimated to 42 mm Hg and diastolic function could not be assessed. On day 5 of his hospital course, he developed retrosternal chest pain overnight and his ECG now revealed a normal sinus rhythm with deep symmetrical T wave inversions in the anterior septal and apical leads, presenting as Wellen’s syndrome (Fig. 1).
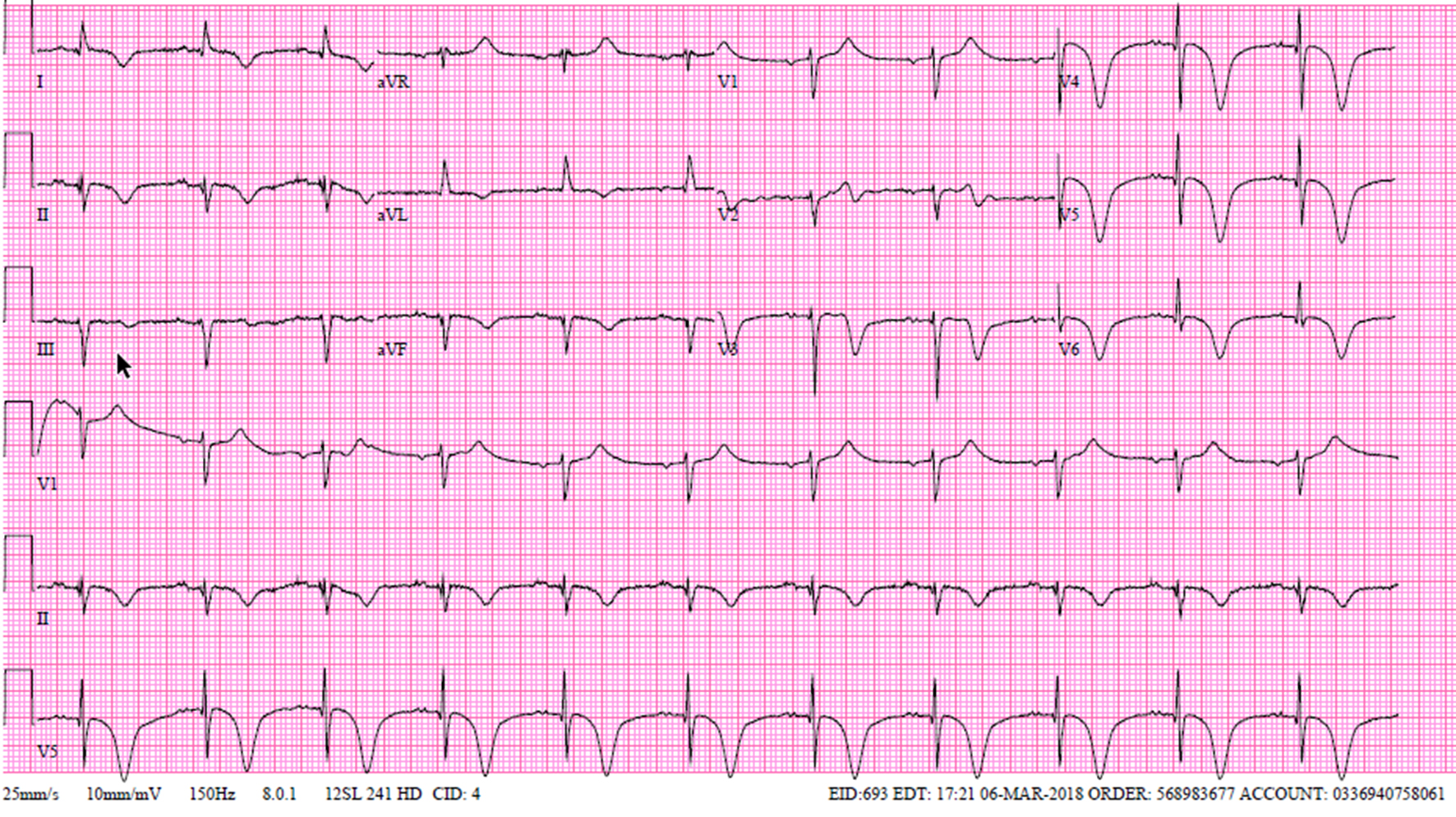 Click for large image | Figure 1. ECG with deep T wave inversions in precordial leads, presenting as Wellens syndrome. |
Hospital course
Once he was admitted to the general medicine floor, the patient was being worked up for his abdominal pain. On day 5, he developed new retrosternal chest pain, relieved by nitroglycerin sublingual tablets. Based on his chest pain, dynamic ECG changes and mild elevation in troponin, a cardiac catheterization was warranted. On day 6, cardiac catheterization via right radial approach demonstrated moderate non-obstructive diffuse disease of left anterior descending artery, left circumflex artery and a dominant right coronary artery. Left ventricle end diastolic pressure (LVEDP) was 20 mm Hg. Left ventriculogram (Fig. 2) showed apical near akinesis and preserved basal wall motion, characteristic of Takotsubo cardiomyopathy (TCM). The estimated left ventricle ejection fraction was 35-40%. He was managed medically and remainder of his hospital course was uneventful. He was discharged home on day 7 with prescriptions for metoprolol of 50 mg, aspirin of 81 mg, atorvastatin of 80 mg and lisinopril of 20 mg. He was provided outpatient follow-up with cardiology. It was believed that correction of his metabolic disarray in conjunction with his alcohol withdrawal may have triggered this event. On his outpatient follow-up, his repeat echocardiogram showed an improvement in his ejection fraction to 60-65% with normal systolic function.
 Click for large image | Figure 2. Left ventriculogram showing apical ballooning, hypokinesis and basal hyperkinesis. |
| Discussion | ▴Top |
TCM was first described in 1990 by Sato et al from Japan [2]. Since the initial description, there have been many case reports of this condition in medical literature. In majority of cases, TCM is triggered by an emotionally or physically stressful event. Physical stressors in the form of acute asthma exacerbation, major surgery, chemotherapy or stroke were linked to 36% of cases, followed by emotional triggers seen in 28% of cases in the International Takotsubo Registry Study [3, 4] and 29% had no evident trigger. There are few case reports of TCM in hyponatremia. In majority of these case reports, it was severe hyponatremia that was linked to TCM. Table 1 shows the compilation of case reports that reported TCM with isolated hyponatremia without seizures [5-13].
 Click to view | Table 1. Case Reports of Takotsubo Cardiomyopathy with Hyponatremia |
In case report 5, patient presented with severe hyponatremia of 118 meq/L and was subsequently treated with an intravenous infusion of 3% saline at a rate of 50 cc/h and with improvement in the sodium level to 131 meq/L at 36 h from initial presentation. Patient was noted to have T wave inversions on day 2 of admission, at which time the sodium level was noted to be 131 meq/L. The patient in our case presented with a sodium level of 127 meq/L, which was corrected to 137 meq/L conservatively with normal saline. The exact reason for his hyponatremia is unknown and is thought to be secondary to poor oral intake or chronic alcoholism. On day 5 of presentation, his laboratory examination showed a sodium level of 137 meq/L and the symptoms of retrosternal chest with ECG findings of symmetric T wave inversions with a mild troponin leak. Our patient also has a history of chronic alcohol abuse and was unable to definitively report when he had his last alcoholic drink. He received lorazepam on the first day of his admission as there was a concern for withdrawal. His withdrawal assessment scores were < 12 for the most part. No other triggers or stressful events can be identified after detailed review of his hospital course. It is unclear if correction of hyponatremia can be a physiological trigger for TCM. The exact cause of TCM is unknown; however, various etiologies were presumed that include coronary vasospasm, plaque rupture, microcirculatory dysfunction, metabolic disturbances and catecholamine hypothesis, although no consensus with respect to pathophysiology has yet been reached [14].
Catecholamine-mediated stunning of the myocardium is believed to be the leading mechanism of underlying TCM, but again evidence is limited [15]. Excessive adrenergic stimulation may shift the beta-receptor from its stimulatory G protein-mediated pathway to an inhibitory G protein pathway, thereby decreasing cyclic adenosine monophosphate (cAMP) levels and leading to transient myocardial dysfunction.
The exact pathogenesis of hyponatremia or correction of hyponatremia in TCM may not be catecholamine-mediated. Goldenberg and colleagues [16] mentioned in their case report about a patient with hyponatremia (sodium level of 123 meq/L), who had repeated episodes of CK-MB elevation. The mechanism by which serum levels of sodium affect myocardium is independent of catecholamines. It could be due to damage of subclinical myocyte through intracellular movement of water and swelling of cells, induced by hyponatremia. Santos et al [7] speculated that hyponatremia could interfere with myocardial inotropism by modulation of cardiomyocyte Na+/Ca2+ exchange and also result in hypotonicity-induced myocardial swelling.
Conclusions
Our case illustrates TCM precipitated by isolated mild hyponatremia. It is unclear if correction of hyponatremia precipitated the event. Unfortunately, there is limited evidence in this regard. After diagnosis, it is important to triage TCM patients and stratify their risk factors in order to select appropriate treatment. No evidence currently exists to guide treatment choices in complex patients. Future research should be focused on randomized control trials to guide treatment as medical treatment in TCM remains entirely empirical [17]. Although reversibility, morbidity and mortality of TCM remain high during the acute and subacute phases of the disease, patients are prone to severe complications, including heart failure, cardiogenic shock and life-threatening arrhythmias. The large International Takotsubo Registry included 1,750 patients and it reported 5.9% mortality after 30 days and death rate during long-term follow-up was 5.6% per patient year [4]. Our patient had uneventful hospital course after having catheterization and was discharged home, and his repeat echocardiogram in 5 months showed improved ejection fraction.
Conflict of Interest
The authors declare that they have no conflict of interest.
| References | ▴Top |
- Kurowski V, Kaiser A, von Hof K, Killermann DP, Mayer B, Hartmann F, Schunkert H, et al. Apical and midventricular transient left ventricular dysfunction syndrome (tako-tsubo cardiomyopathy): frequency, mechanisms, and prognosis. Chest. 2007;132(3):809-816.
doi pubmed - Sato H, Tateishi H, Uchida T, et al. Takotsubo type cardiomyopathy due to multivessel spasm. In: Kodama K, Haze K, Hon M (eds). Clinical aspect of myocardial injury: from ischemia to heart failure. Kagaku Hyoronsha, Tokyo. 1990; p. 55-64.
- Siddique M, et al. Tako Tsubo registry. Takotsubo International Registry. University Hospital Zurich. 2011.
- Templin C, Ghadri JR, Diekmann J, Napp LC, Bataiosu DR, Jaguszewski M, Cammann VL, et al. Clinical features and outcomes of Takotsubo (Stress) cardiomyopathy. N Engl J Med. 2015;373(10):929-938.
doi pubmed - AbouEzzeddine O, Prasad A. Apical ballooning syndrome precipitated by hyponatremia. Int J Cardiol. 2010;145(1):e26-29.
doi pubmed - Kawano H, Matsumoto Y, Arakawa S, Hayano M, Fijisawa H. Takotsubo cardiomyopathy in a patient with severe hyponatremia associated with syndrome of inappropriate antidiuretic hormone. Intern Med. 2011;50(7):727-732.
doi pubmed - Santos M, Dias V, Meireles A, Gomes C, Luz A, Mendes D, Caiado L, et al. Hyponatremia - an unusual trigger of Takotsubo cardiomyopathy. Rev Port Cardiol. 2011;30(11):845-848.
doi pubmed - Sagiv O, Vukelic S, Czak S, Messineo F, Coplan NL. Apical ballooning syndrome associated with isolated severe hyponatremia: case report and suggested pathophysiology. Rev Cardiovasc Med. 2012;13(4):e198-202.
pubmed - Chikata A, Omi W, Saeki T, Nagai H, Sakagami S. Repeated pacemaker dysfunction in a patient with recurrent Takotsubo cardiomyopathy precipitated by hyponatremia. Int J Cardiol. 2014;170(3):443-444.
doi pubmed - Cecconi A, Franco E, de Agustin JA, Vilchez JP, Palacios-Rubio J, Sanchez-Enrique C, Fernandez-Ortiz A, et al. Hyponatremia-induced stress cardiomyopathy due to psychogenic polydipsia. Int J Cardiol. 2016;202:618-620.
doi pubmed - Jha KK, Kumar M, Jha U, Desar S. Takotsubo cardiomyopathy in a patient with SIADH. Int J Cardiol. 2016;225:342-344.
doi pubmed - Purdy A, Ren B. A broken heart: a rare complication of hyponatremia. Journal of Medical Cases. 2018;9(5):147-150.
doi - Patnaik S, Punjabi C, Nathan R, Khurram I, Witzke C, Lai YK. Bland and broken hearted: A case of hyponatremia induced Tako-tsubo cardiomyopathy. Int J Cardiol. 2015;187:267-271.
doi pubmed - Watanabe M, Izumo M, Akashi YJ. Novel understanding of Takotsubo syndrome. Int Heart J. 2018;59(2):250-255.
doi pubmed - Wittstein IS, Thiemann DR, Lima JA, Baughman KL, Schulman SP, Gerstenblith G, Wu KC, et al. Neurohumoral features of myocardial stunning due to sudden emotional stress. N Engl J Med. 2005;352(6):539-548.
doi pubmed - Goldenberg I, Jonas M, Thaler M, Grossman E. Elevated levels of serum creatine kinase induced by hyponatraemia. Postgrad Med J. 1997;73(862):511-512.
doi pubmed - Singh Kuljit, Akashi Yoshihiro, Horowitz John. Takotsubo syndrome therapy: current status and future directions. International Cardiovascular Forum Journal. 2016;5. 10.17987/icfj.v5i0.223.
doi
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


