| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 9, Number 8, August 2018, pages 260-263
Managing Embolized Vertebral Artery Stent – A Drag-Back Approach
Noor Dastgira, Arslan Masooda, b, Ahmed Muqeeta, Zubair Akrama
aDepartment of Cardiology, Allama Iqbal Medical College, Jinnah Hospital, Lahore, Pakistan
bCorresponding Author: Arslan Masood, House # 229, Tariq Block, New Gardentown, Lahore, Pakistan
Manuscript submitted June 3, 2018, accepted June 22, 2018
Short title: Managing Embolized VAS
doi: https://doi.org/10.14740/jmc3104w
| Abstract | ▴Top |
Ischemia involving the posterior cerebral circulation carries high morbidity and mortality. Endovascular access to the vertebral artery is a relatively safe and straightforward management option. The feasibility and safety of angioplasty and stenting is well demonstrated in multiple centers. Periprocedural risks include stent embolization, malposition, stent fracture, vessel rupture, dissection and thrombosis. We present a case of vertebral artery stenting that was complicated by distal embolization of the stent. The anatomical difficulties while managing the complication were challenging. A novel drag-back technique was successfully tried and is described here along with discussion of other management options described in literature.
Keywords: Vertebral artery; Vertebrobasilar insufficiency/therapy; Endovascular; Cerebral revascularization
| Introduction | ▴Top |
Ischemia involving the posterior cerebral circulation is less common compared to anterior circulation; however, it is associated with more morbidity and mortality and a higher risk of stroke or death in cases of medically refractory vertebral artery stenosis [1]. Mortality as high as 80-100% and stroke up to 5-11% have been observed [2]. Symptomatic vertebrobasilar insufficiency should be considered for revascularization in patients with bilateral vertebral artery stenosis of more than 60%, or a similar unilateral stenosis in the setting of a hypoplastic or occluded contralateral vertebral artery [3].
Endovascular access to the vertebral artery is relatively safe and straightforward. The feasibility and safety of angioplasty and stenting is well demonstrated in a single-center retrospective case series [2]. Periprocedural risks include stent embolization, malposition, stent fracture, vessel rupture, dissection and thrombosis. We present a case of vertebral artery stenting (VAS) that was complicated by distal embolization of the stent. The anatomical difficulties while managing the complication were challenging. A novel drag-back technique was successfully tried and is described here along with discussion of other management options described in literature.
| Case Report | ▴Top |
A 63-year-old male who already had weakness of left half of the body for 1 year presented with exertional pain and numbness in the right arm for 3 months. It was accompanied by dizziness that would typically occur during right arm exertion. On examination, all pulses of the right upper limb and right carotid were weak, while all pulses on the left were normal. A probable diagnosis of subclavian steal syndrome was made based on the Doppler examination that revealed post-stenotic low velocity signals in right arm arteries and retrograde (caudal) flow in right vertebral artery.
Subsequently, angiography of neck vessels was carried out which showed occluded innominate artery with arterial supply to right subclavian and common carotid through retrograde right vertebral flow. There was, however, also a severe ostial stenosis of left vertebral artery (Fig. 1). It was followed by an unsuccessful attempt at recanalization of innominate artery and the patient was referred for surgical consultation. While the patient was being scheduled for the surgical revascularization, he had recurrent and worsening vertigo, nausea and vomiting - attributed to ongoing vertebrobasilar insufficiency. Considering his symptoms and expected simplicity of the procedure, he was advised ostial stenting of left vertebral artery as a bridge to improve the posterior circulation while he awaited surgery.
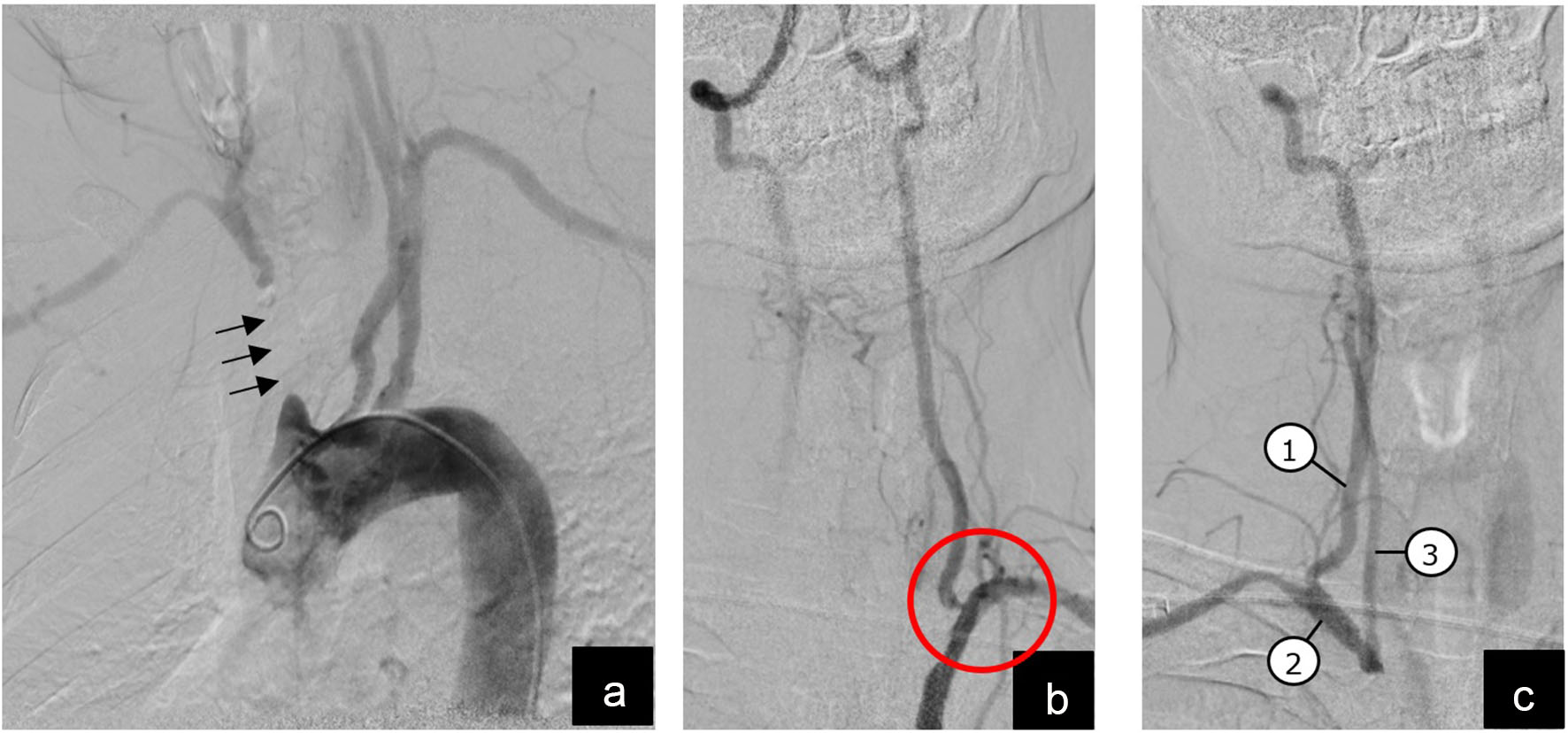 Click for large image | Figure 1. Diagnostic angiography with digital subtraction imaging. (a) Arch aortogram showing blocked segment of innominate artery (arrows); (b) magnified view of left vertebral artery arising from left subclavian artery with a severe stenosis at vertebral origin (red circle); (c) magnified view of right vertebral artery (1) that has a retrograde/caudal flow and fills right subclavian (2) and right common carotid (3) arteries. |
A left radial approach was used and a 6 French Judkin’s - right guiding catheter was placed in the left subclavian artery near the origin of left vertebral branch. The ostial lesion was predilated with a semi-compliant balloon followed by stenting with a 4 × 12 mm coronary drug eluting stent. The stent was under-expanded at the inlet and while trying to track a non-compliant balloon to optimize it, the stent got embolized distally into the vertebral artery nearly at the level of base of skull (Fig. 2)
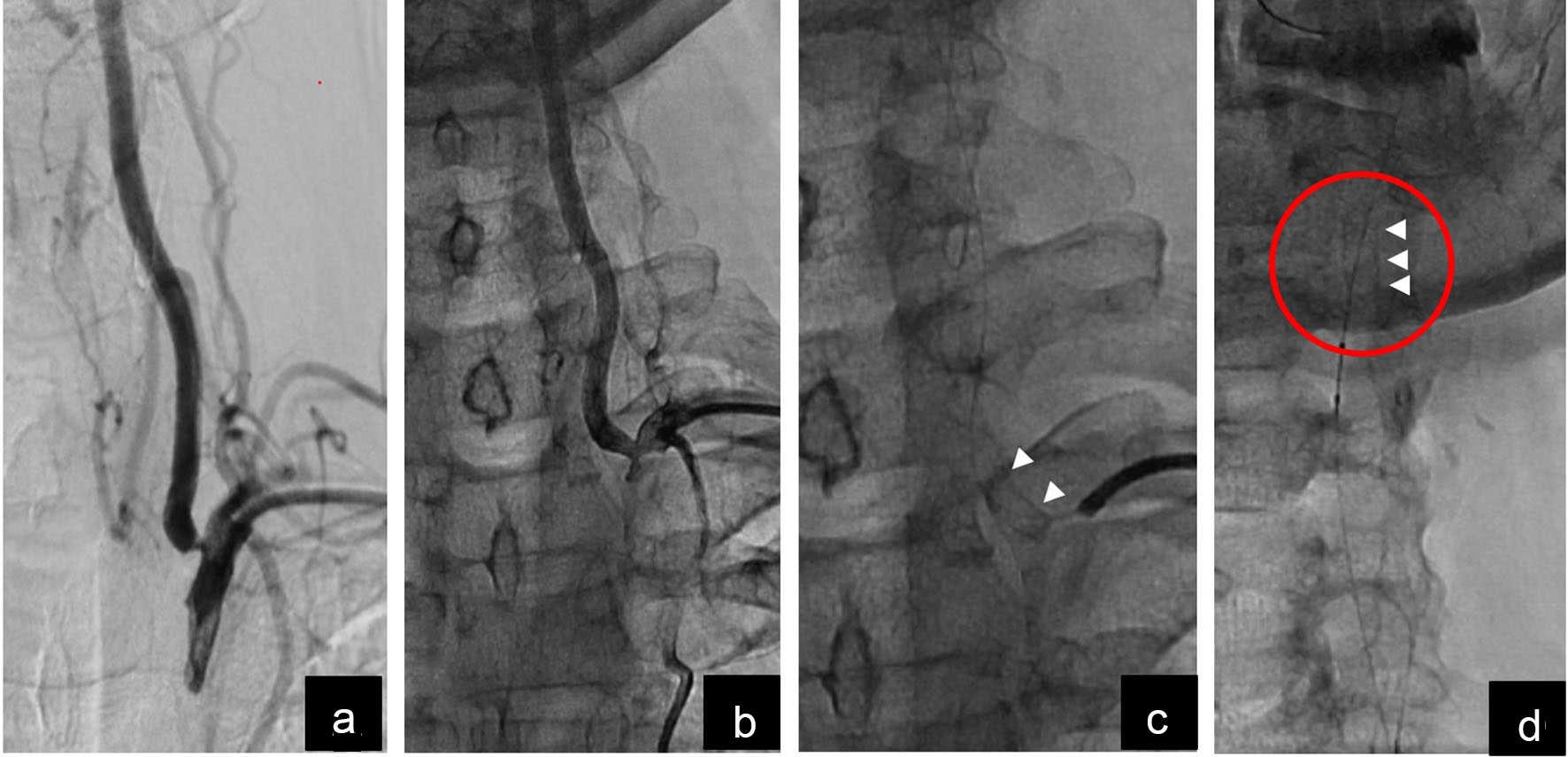 Click for large image | Figure 2. Magnified pictures of left vertebral artery ostial intervention and stent embolization. (a) Vertebral ostium before intervention; (b) partially improved stenosis after ballooning and stenting; (c) short stent visible at vertebral ostium (white arrow heads); (d) embolized stent visualized in distal left vertebral artery above the mandibular line (white arrowheads). |
A drag-back approach was used to fix this embolized stent where a 4.5 mm non-compliant balloon was carefully passed beyond the stent over the same wire, inflated at a very low pressure of 4 atmospheres and slowly pulled back to drag down the embolized stent with it. The manoeuvre was carried out in a stepwise fashion with test injections repeatedly to check for vessel trauma. The stent was finally brought down to the proximal most segment of vertebral artery and was dilated with the same balloon at a higher pressure to anchor it against the arterial wall. Another 4 × 28 mm drug eluting coronary stent was placed, starting from the vertebral ostium and overlapping the distal (initially embolized) stent and post-dilated at higher pressures with 4.5 mm non-compliant balloon (Fig. 3).
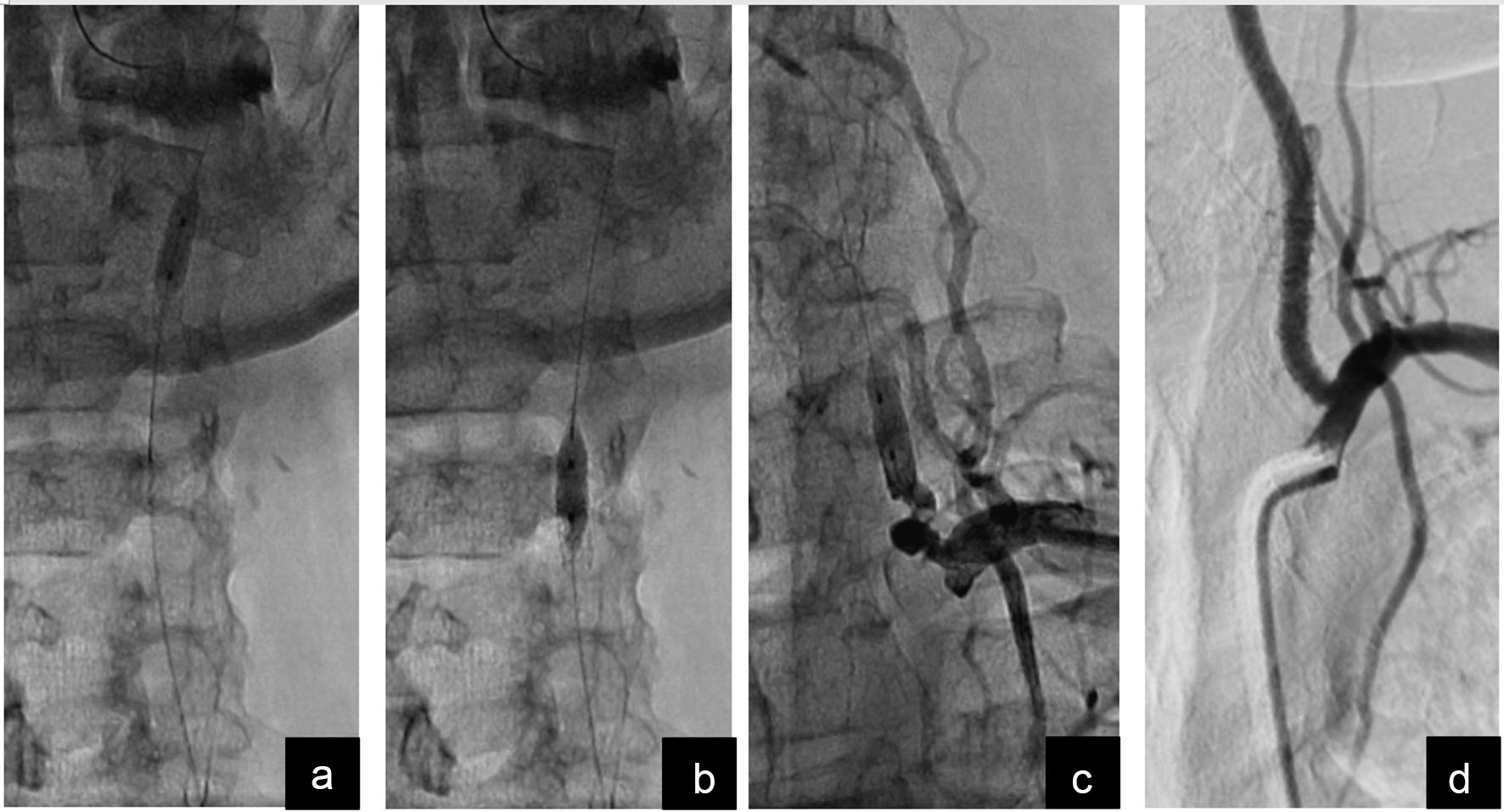 Click for large image | Figure 3. Drag-back technique to manage the embolized stent. (a) Balloon tracked beyond the stent and inflated at low pressure; (b) embolized stent being dragged back by gentle traction on the balloon; (c) embolized stent successfully dragged back to the proximal-most segment of left vertebral artery and anchored against the vessel wall by inflating the same balloon at higher pressure; (d) final result after deploying another stent starting from vertebral artery ostium and overlapping the first stent. |
The patient remained stable throughout the procedure, right arm arterial pressure improved considerably and his symptoms significantly improved after the procedure. He was subsequently referred for surgical revascularization of the blocked innominate artery.
| Discussion | ▴Top |
The safety and efficacy of endoluminal stenting in treating atherosclerotic vertebral artery disease was evaluated in a trial. Success (< 20% residual diameter stenosis, without stroke or death) was achieved in all patients (100%). At follow-up (mean: 10.6 months), all patients (100%) were alive and 97% were asymptomatic [4]. Another study done by Lin et al evaluated the safety and feasibility of stent implantation for vertebral artery ostial stenosis and reached the conclusion that it was relatively safe to treat symptomatic ostial vertebral artery stenosis using coronary techniques and equipment [5]. Unlike cerebral angioplasty and carotid artery stenting, which have a low risk of restenosis, VAS has a significantly higher restenosis rate [6, 7]. Little information is available regarding the use of drug-eluting stents, although initial reports indicate a lower restenosis rate [8]. Endoluminal stenting of vertebral artery lesions is safe, effective and durable as evidenced by the low recurrence rate. Primary stent placement is an attractive option for atherosclerotic vertebral artery stenotic lesions.
Many methods have been reported previously to tackle dislodged or embolized coronary stents. The potential techniques range from leaving the embolized stents at embolized site to their surgical removal. Other methods include snaring and post-dilation to anchor them at the embolized site. In this case, the embolized stent could had been left at the embolized site and anchored by further dilations; however, there was a risk of stent kinking, fracture and disfigurement due to torsion and flexion forces of head and neck movements. This could lead to vessel trauma, rupture or stent thrombosis - all with potential catastrophic outcomes. The option of snaring was also considered but turned down due to expected stent disfigurement, which would have made it impossible to pass through the stenosed ostium of vertebral artery. The successfully executed novel technique described here is not free of risks. It could end up in stent disfigurement, arterial dissection or rupture and distal balloon entrapment. Despite potential risks, the technique offers an effective way of fixing a dislodged stent particularly in large lumen vessels without acute bends or tortuosity, partially inflated dislodged stents and where the inflated stent diameter is adequately smaller than that of the vessel lumen.
In conclusion, VAS is a relatively straightforward procedure; however, an interventional approach should be carefully planned.
For ostial stenting, adequate sized and properly expanded stent may prevent embolization.
Conflict of Interest
All the authors hereby disclose that they do not have any potential conflict of interest to mention.
Financial Support
No grant or financial assistance received in this regard.
| References | ▴Top |
- Stayman AN, Nogueira RG, Gupta R. A systematic review of stenting and angioplasty of symptomatic extracranial vertebral artery stenosis. Stroke. 2011;42(8):2212-2216.
doi pubmed - Jenkins JS, Patel SN, White CJ, Collins TJ, Reilly JP, McMullan PW, Grise MA, et al. Endovascular stenting for vertebral artery stenosis. J Am Coll Cardiol. 2010;55(6):538-542.
doi pubmed - Lee CJ, Morasch MD. Endovascular management of vertebral artery disease. Expert Rev Cardiovasc Ther. 2011;9(5):575-578.
doi pubmed - Younis GA, Gupta K, Mortazavi A, Strickman NE, Krajcer Z, Perin E, Achari A. Predictors of carotid stent restenosis. Catheter Cardiovasc Interv. 2007;69(5):673-682.
doi pubmed - Dabus G, Gerstle RJ, Derdeyn CP, Cross DT, 3rd, Moran CJ. Endovascular treatment of the vertebral artery origin in patients with symptoms of vertebrobasilar ischemia. Neuroradiology. 2006;48(12):917-923.
doi pubmed - Gupta R, Al-Ali F, Thomas AJ, Horowitz MB, Barrow T, Vora NA, Uchino K, et al. Safety, feasibility, and short-term follow-up of drug-eluting stent placement in the intracranial and extracranial circulation. Stroke. 2006;37(10):2562-2566.
doi pubmed - Jenkins JS, White CJ, Ramee SR, Collins TJ, Chilakamarri VK, McKinley KL, Jain SP. Vertebral artery stenting. Catheter Cardiovasc Interv. 2001;54(1):1-5.
doi pubmed - Lin YH, Juang JM, Jeng JS, Yip PK, Kao HL. Symptomatic ostial vertebral artery stenosis treated with tubular coronary stents: clinical results and restenosis analysis. J Endovasc Ther. 2004;11(6):719-726.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


