| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 8, Number 12, December 2017, pages 396-399
Norepinephrine Type Pheochromocytoma With Concomitant Aortic Aneurysms: A Distinctive Association
Ayman R. Fatha, c, Anthony H. Kashoua, c, Bashaer Gheyatha, Hisham E. Kashoub, d
aCardiology Department at Cleveland Clinic, Cleveland, OH, USA
bDepartment of Cardiology, United Health Services Hospitals, Wilson Regional Medical Center, Johnson City, NY, USA
cThese authors contributed equally to this work
dCorresponding Author: Hisham E. Kashou, United Health Services Hospitals, Wilson Regional Medical Center, 30 Harrison St #250, Johnson City, NY 13790, USA
Manuscript submitted September 17, 2017, accepted October 17, 2017
Short title: Pheochromocytoma and Aortic Aneurysms
doi: https://doi.org/10.14740/jmc2922w
| Abstract | ▴Top |
Pheochromocytoma is a rare catecholamine secreting tumor. It has two types based on plasma catecholamines levels: 1) norepinephrine type and 2) mixed epinephrine-norepinephrine type. Few reports in the literature have documented the coexistence of pheochromocytoma with abdominal aortic aneurysm and proposed an association between them. In this report, we support these reports and present a case of norepinephrine type pheochromocytoma with concomitant aortic aneurysms. These aneurysms were found in the abdominal aorta, ascending, and descending thoracic aorta. That is unlike previous reports that had the aneurysms confined to the abdominal aorta. Uniquely, we suggest that this type of pheochromocytoma (the norepinephrine type) is associated with a more aggressive and extensive damage to the aortic walls. We also support that the etiology may be associated with the persistent elevation of catecholamines levels secreted from the tumor. Consequently, the aortic walls are damaged and become weak, predisposing them to aneurysm formation.
Keywords: Pheochromocytoma; Aortic aneurysm; Abdominal aortic aneurysm
| Introduction | ▴Top |
Pheochromocytoma is a rare chromaffin cell tumor that secretes catecholamines which can precipitate life-threatening hypertension [1]. It is usually benign in nature, but a few malignant tumors have also been reported. The diagnosis is made by measuring plasma metanephrines or a 24-h urinary collection for catecholamines and metanephrines [2]. Approximately 10% are discovered incidentally [3]. Computed tomography (CT) and magnetic resonance imaging (MRI) are often used for localization, with the latter being the modality of choice. Surgical resection of the tumor is the treatment of choice and often cures the associated hypertension. Careful preoperative treatment with alpha blockade and, if required, beta blockers are important in the prevention of intraoperative hypertensive crises [4].
An aortic aneurysm (AA) is defined as a localized or diffuse dilation of the aorta with a diameter increase of more than 50% of its normal limits. It can be localized above the diaphragm (thoracic AA) or below it (abdominal aortic aneurysm (AAA)). It can also present on either sides of the diaphragm (thoracoabdominal aneurysm). The etiology encompasses infections, arteritis, trauma, and inherited connective tissue disorders. Smoking is the strongest risk factor associated with AAs. Hypertension, atherosclerosis, increasing age, male sex, and increased body mass index have also been thought to be associated. There has been an inverse association noted with females, African Americans, and diabetics [5, 6]. Although the majority are asymptomatic and are often detected incidentally on imaging, they can be potentially life-threatening. Surgical repair is still the definitive treatment.
There are few reports in the literature that propose an association between pheochromocytoma and AAA [7, 8]. Herein, we support those few and, uniquely, report the first norepinephrine type (NE-type) pheochromocytoma coexisting in association with diffuse AAs.
| Case Report | ▴Top |
A 60-year-old African American male with a history of refractory hypertension, type 2 diabetes, tobacco use, heart failure, bilateral renal artery stenosis, and chronic kidney disease presented to the hospital with a 1-week history of diarrhea, altered mental status, weakness, and nausea. At presentation, he was bradycardic and disoriented to time. Otherwise, his physical exam was unremarkable. He was hyperkalemic as a result of acute on chronic kidney injury with elevated liver enzymes and bilirubin levels.
An abdominal ultrasound was performed to evaluate his hyperbilirubinemia, which revealed an incidental AAA and a mass atop the left kidney. Contrast-enhanced CT scan of abdomen and pelvis demonstrated an AAA with involvement of the mesenteric vessels. The AAA showed maximum diameter of 5.3 cm at the level of celiac artery (Fig. 1). Additionally, a retroperitoneal mass was detected between the superior pole of the left kidney and abdominal aorta. This measured 5.3 × 4.7 cm with irregular peripheral enhancement concerning for an adrenal tumor (Fig. 2). For verification, an abdominal and pelvic MRI was done and confirmed the CT findings.
 Click for large image | Figure 1. Abdominal CT with contrast revealing an AAA with a maximum diameter of 5.3 cm at the level of the celiac artery. |
 Click for large image | Figure 2. Abdominal CT with contrast showing a left suprarenal mass 5.3 × 4.7 cm in size. |
In light of the patient’s refractory hypertension, the presence of pheochromocytoma was suspected. Further serum and urine biochemical studies yielded a greater than seven-fold increase in total plasma metanephrines (10-fold increase in free plasma normetanephrine with low free plasma metanephrines) and a six-fold increase in 24-h urine total metanephrines (seven-fold increase in 24-h urine normetanephrine with normal 24-h fractionated metanephrines). Plasma cortisol, aldosterone, and supine renin activity levels were found to be low (Table 1). Thus, a diagnosis of adrenal pheochromocytoma was made. I-MIBG scintigraphy was not done due to the high risk of interaction with some of the patient’s medications that could not be discontinued.
 Click to view | Table 1. Serum and Urine Biochemical Studies |
In order to assess the integrity of the thoracic aorta, a chest CT without contrast was done and detected an ascending AA with diameter of 4.3 cm at the level of the right pulmonary artery as well as a descending thoracic AA with diameter of 4.7 cm at the level of the diaphragm. A surgical approach was deferred at this time after expert consultation with vascular surgery as the patient was asymptomatic. The patient’s CKD status placed him at higher risk for dialysis-dependence and this outweighed the benefits of a surgical approach. Thus, the case was managed medically and the initial plan of pheochromocytoma resection was discussed with endocrine surgery and deferred to a point of time when his renal function is optimal.
| Discussion | ▴Top |
Although aneurysms can occur anywhere in the aorta, the abdomen is the most common site. The majority of AAAs occur below the level of the renal arteries with a size greater than 4.0 cm. Thoracic AAs are subdivided depending on the location: ascending aorta, aortic arch, and descending aorta. Prognosis is based on size, growth rate, and severity of coexisting vascular diseases. The greater the size and the faster the growth rate of the aneurysm, the greater the risk for rupture and the worse the prognosis.
Pheochromocytoma has been classified into two types based on plasma catecholamine levels: 1) NE-type and 2) mixed epinephrine-norepinephrine type (E-type). The NE-type has been reported to have an association with a deficiency in the phenylethanolamine N-methyltransferase (PNMT) [9]. Deficiency in PNMT would result in a buildup of normetanephrine and a relative deficiency in metanephrine (Fig. 3). No genetic testing was done on our patient to prove that he had a PNMT deficiency. However, his lab values showing very high normetanephrine and low metanephrine levels coincide with the NE-type pheochromocytoma.
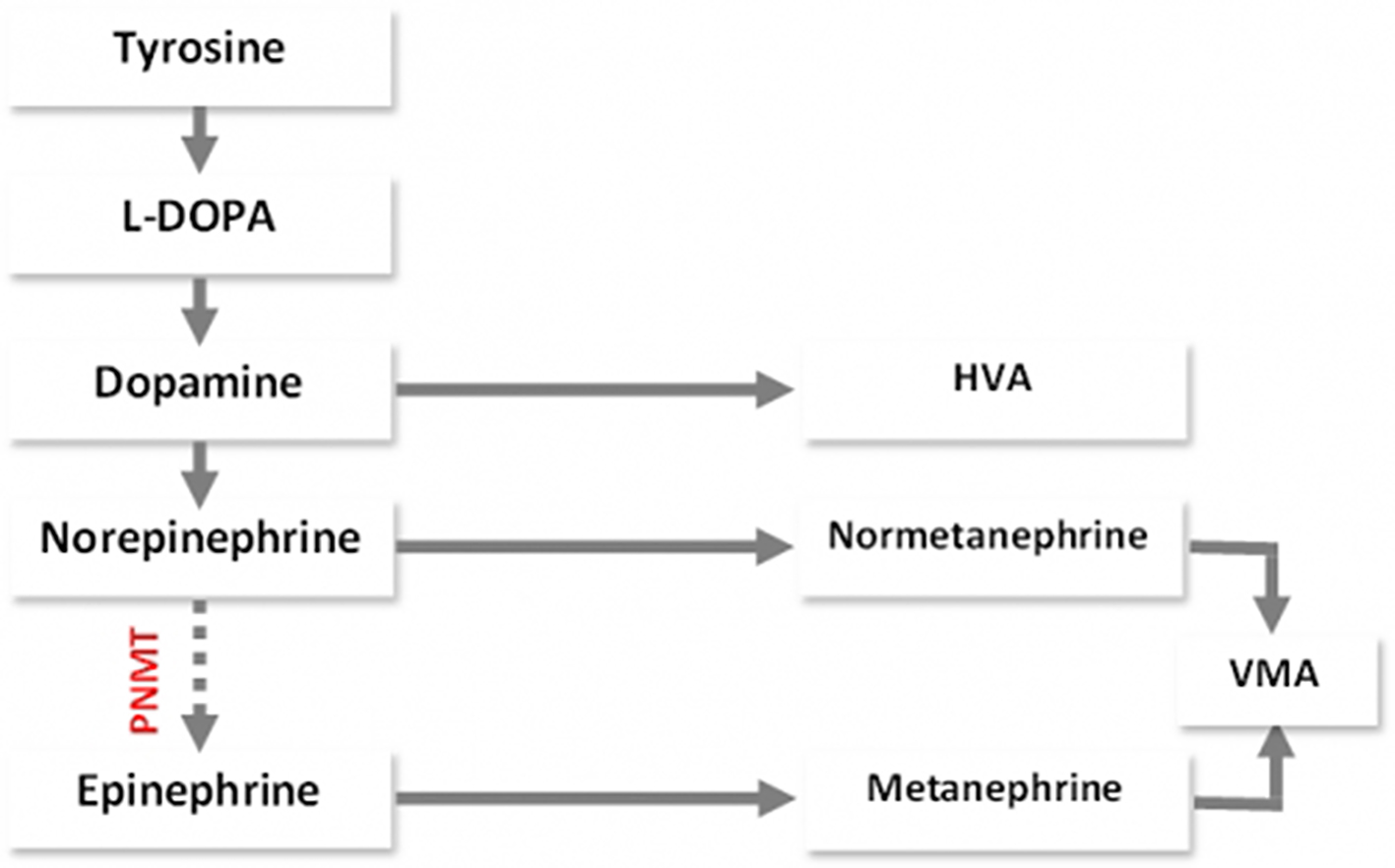 Click for large image | Figure 3. Catabolism of catecholamines - normetanephrine and metanephrine. |
The coexistence of pheochromocytoma and AAA has been reported previously in the literature [7, 8]. Our article reaffirms such association and substantiates the authors’ claim. Persistently high catecholamines in the blood damage and weaken the vascular endothelium of the aorta. With more than seven-fold rise in total catecholamine levels in our patient, it is plausible that this played a role in developing his AAs. Additionally, we propose a distinctive association between the NE-type pheochromocytoma and AAs. We believe that the NE-type may have a greater propensity and aggressive nature that can cause more destructive damage throughout the aorta compared to the E-type. This was manifested in our patient with multiple aortic aneurysmal lesions at the ascending, descending thoracic, and abdominal aorta.
Management of patients with coexisting pheochromocytoma and AA remains an evolving field. The rarity of this coexistence leaves ideal management unclear with no specific guidelines. It is suggested that concomitant surgical removal of the pheochromocytoma and AA repair be attempted if the patient’s condition allows. Regarding AAA, surgical repair is recommended if the aneurysm is ≥ 5.5 cm and/or symptomatic. For patients that are surgical candidates, pre-operative medical optimization is crucial. Alpha and possibly beta-adrenergic blockade decrease the perioperative and cardiovascular morbidity and mortality related to the catecholamine surge [4]. Unfortunately, our asymptomatic patient was not a surgical candidate at the time due to his acutely worsened kidney function. Therefore, he was medically managed with blood pressure control and close follow-up until his clinical status improved, upon which a surgical option would be reconsidered.
In conclusion, pheochromocytoma is associated with high levels of circulating catecholamines that damage and weaken aortic walls. Consequently, this can result in the development of AAs. The NE-type pheochromocytoma demonstrated in our case appears to have a more diffuse and aggressive effect on the aortic walls compared to the E-type that is usually confined to one area. We encourage all clinicians to report similar cases with coexisting pheochromocytoma and AAs as well as, to note the type of pheochromocytoma (NE- versus E-type) in order to further evaluate for a possible association.
Acknowledgments
We thank Dr. Douglas Nachand, MD, an abdominal imaging fellow from the Radiology Department at Cleveland Clinic, for reading and confirming the images used in this report.
Conflict of Interest
Authors have no conflict of interest.
Funding Support
The work was not supported or funded by any drug company.
| References | ▴Top |
- Liao WB, Liu CF, Chiang CW, Kung CT, Lee CW. Cardiovascular manifestations of pheochromocytoma. Am J Emerg Med. 2000;18(5):622-625.
doi pubmed - Lenders JW, Pacak K, Walther MM, Linehan WM, Mannelli M, Friberg P, Keiser HR, et al. Biochemical diagnosis of pheochromocytoma: which test is best? JAMA. 2002;287(11):1427-1434.
doi pubmed - Copeland PM. The incidentally discovered adrenal mass. Ann Surg. 1984;199(1):116-122.
doi pubmed - Elenkova A, Matrozova J, Zacharieva S, Kirilov G, Kalinov K. Adiponectin - A possible factor in the pathogenesis of carbohydrate metabolism disturbances in patients with pheochromocytoma. Cytokine. 2010;50(3):306-310.
doi pubmed - Blanchard JF, Armenian HK, Friesen PP. Risk factors for abdominal aortic aneurysm: results of a case-control study. Am J Epidemiol. 2000;151(6):575-583.
doi pubmed - Lederle FA, Johnson GR, Wilson SE, Chute EP, Littooy FN, Bandyk D, Krupski WC, et al. Prevalence and associations of abdominal aortic aneurysm detected through screening. Aneurysm Detection and Management (ADAM) Veterans Affairs Cooperative Study Group. Ann Intern Med. 1997;126(6):441-449.
doi pubmed - Kota S, Kota S, Meher L, Jammula S, Mohapatra S, Modi K. Coexistence of pheochromocytoma with abdominal aortic aneurysm: an untold association. Ann Med Health Sci Res. 2013;3(2):258-261.
doi pubmed - Spanos C, Moros I, Spanos G, Drakotou I, Mavromanolis H, Spanos P. Elective resection of pheochromocytoma with concomitant abdominal aortic aneurysm repair: report of a case. Surg Today. 2006;36(8):741-743.
doi pubmed - Kimura N, Togo A, Sugimoto T, Nata K, Okamoto H, Nagatsu I, Nagura H. Deficiency of phenylethanolamine N-methyltransferase in norepinephrine-producing pheochromocytoma. Endocr Pathol. 1996;7(2):131-136.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


