| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 7, Number 12, December 2016, pages 550-553
A Case of Peripartum Cardiomyopathy Affected by Left Ventricle Thrombus
Nobuhiro Takeuchia, e, Kazumasa Emoria, Junichi Sonedab, Kaori Mohric, Masanori Takadad
aDepartment of Internal Medicine, Kobe Tokushukai Hospital, 1-3-10 Kamitakamaru, Tarumi-ku, Kobe-shi, Hyogo 655-0017, Japan
bDepartment of Cardiovascular Surgery, Kobe Tokushukai Hospital, 1-3-10 Kamitakamaru, Tarumi-ku, Kobe-shi, Hyogo 655-0017, Japan
cDepartment of Laboratory Medicine, Kobe Tokushukai Hospital, 1-3-10 Kamitakamaru, Tarumi-ku, Kobe-shi, Hyogo 655-0017, Japan
dDivision of Cardiology, Department of Internal Medicine, Kawasaki Hospital, 3-3-1 Higashiyama-cho, Hyogo-ku, Kobe-shi, Hyogo 652-0042, Japan
eCorresponding Author: Nobuhiro Takeuchi, Department of Internal Medicine, Kobe Tokushukai Hospital, 1-3-10 Kamitakamaru, Tarumi-Ku, Kobe-shi, Hyogo 655-0017, Japan
Manuscript accepted for publication November 18, 2016
Short title: Peripartum Cardiomyopathy
doi: https://doi.org/10.14740/jmc2698w
| Abstract | ▴Top |
Peripartum cardiomyopathy (PPCM) mimicking dilated cardiomyopathy is defined as an idiopathic cardiomyopathy affecting perinatal or postnatal women with no cardiac history. It occurs in 1 in 20,000 births in Japan. A 25-year-old female without cardiology diseases presented to our hospital’s emergency department with upper abdominal pain, exertional dyspnea, and leg edema. One month prior, she gave birth to her first child via vaginal delivery. At 36 weeks of gestation, she was diagnosed with pregnancy hypertension by an obstetrician. Ultrasonography and non-contrast computed tomography were performed and revealed an edematous gallbladder as well as dilated hepatic and inferior jugular veins. Chest X-ray revealed cardiomegaly, lung edema, and pleural effusion. She was diagnosed with congestive heart failure. Transthoracic echocardiogram (TTE) revealed a dilated left ventricle with a reduced ejection fraction (EF) of 17%. Immediately after admission, diuretic agents, including furosemide and carperitide, were administered. Although her heart failure improved with sufficient diuretic treatment, thromboses measuring 16 × 8 and 29 × 11 mm in her left ventricle were revealed by TTE on day 10. Heparin sodium and warfarin potassium were initiated, which reduced the thromboses. Her symptoms improved, although EF was not restored to normal function. She was discharged on day 40 and an outpatient clinic follow-up was scheduled. Long-term prognosis of PPCM is currently unknown, and meticulous follow-up of the patient is required. Here we present a case of PPCM that was affected by a left ventricular thrombus.
Keywords: Peripartum cardiomyopathy; Ventricle thrombus
| Introduction | ▴Top |
Peripartum cardiomyopathy (PPCM) is a cardiac condition which affects perinatal or postnatal women without any cardiology history of cardiac condition and mimics dilated cardiomyopathy. It is characterized by a reduced ejection fraction (EF). Although its frequency is not high, clinicians have to keep in mind this condition because of high mortality rate in its severe cases. PPCM, even with a normal heart beat, may sometimes develop ventricular thrombus due to reduced EF and hypercoagulable status during the perinatal period. We here present a case of PPCM that was affected by a left ventricular (LV) thrombus.
| Case Report | ▴Top |
A 25-year-old female without any medical history visited our emergency department with upper abdominal pain. She recollected suffering from a leg edema at 36 weeks of gestation due to pregnancy hypertension as diagnosed by an obstetrician. A month after she gave birth to her first child, she presented with worsening leg edema and exertional dyspnea. Simultaneously, she also had mild upper abdominal pain. She denied any use of tobacco or alcohol.
On admission, her blood pressure was 127/99 mm Hg, heart rate was 130 beats/min, body temperature was 36.4 °C, and oxygen saturation was 97% on room air. Initial clinical examination revealed a weight of 55 kg, and height of 165 cm. Inspection of the palpebral conjunctiva revealed no evidence of anemia. Auscultation of the heart revealed diastolic and systolic heart murmurs (third and fourth heart sounds) in the cardiac apex. Auscultation of the lungs revealed no rale or other lung sounds. Physical examination of the patient revealed pitting edema in both legs but no cyanosis.
Blood chemistry analyses revealed the following: mildly elevated white blood cell counts (9,220 cells/μL), mild anemia (red blood cell count, 431 × 104 cells/μL; hemoglobin, 11.2 g/dL), mild hypoproteinemia (5.5 g/dL), mild hypoalbuminemia (3.4 g/dL), mildly elevated lactate dehydrogenase (245 IU/L), slightly elevated serum creatinine levels (0.84 mg/dL), and remarkably elevated brain natriuretic peptide levels (2,000 pg/mL). There was no evidence of coagulation dysfunction (prothrombin time, 71%; activated partial thromboplastin time, 26.2 s).
Ultrasonography and non-contrast computed tomography were performed and revealed an edematous gall bladder and dilated hepatic and inferior jugular veins (Fig. 1a, b). Chest X-ray revealed cardiomegaly with a cardio-thoracic ratio of 58%; moreover, there was evidence of pulmonary congestion and pleural effusion (Fig. 1c). Electrocardiogram revealed a normal sinus rhythm, heart rate of 130 beats/min, poor R progression in leads V1-V3, and inverted T wave in leads V4-V6. Transthoracic echocardiogram (TTE) revealed a dilated left ventricle of 63 mm in diastolic phase and 58 mm in systolic phase with a reduced EF of 17% (Fig. 2a, b). Color Doppler revealed moderate mitral regurgitation. At this time, she was diagnosed with congestive heart failure resulting from dilated cardiomyopathy, which was consistent with PPCM.
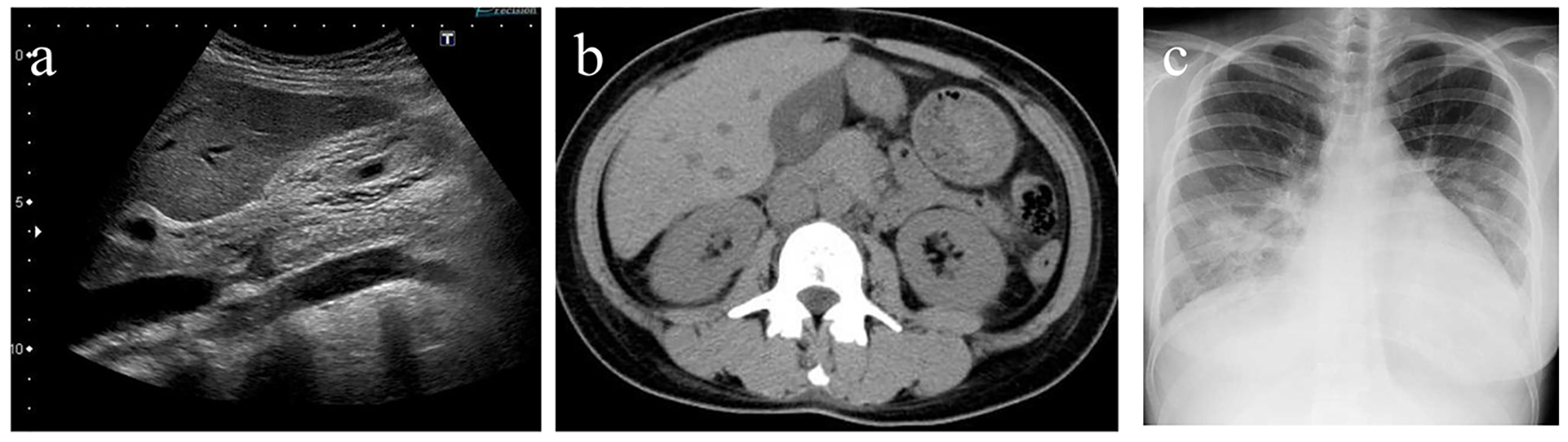 Click for large image | Figure 1. (a) Ultrasonography revealed an edematous gallbladder. (b) Non-contrast computed tomography revealed an edematous gallbladder, dilated hepatic and inferior jugular veins. (c) Chest X-ray revealed cardiomegaly with a cardio-thoracic ratio of 58%, pulmonary congestion, and pleural effusion. |
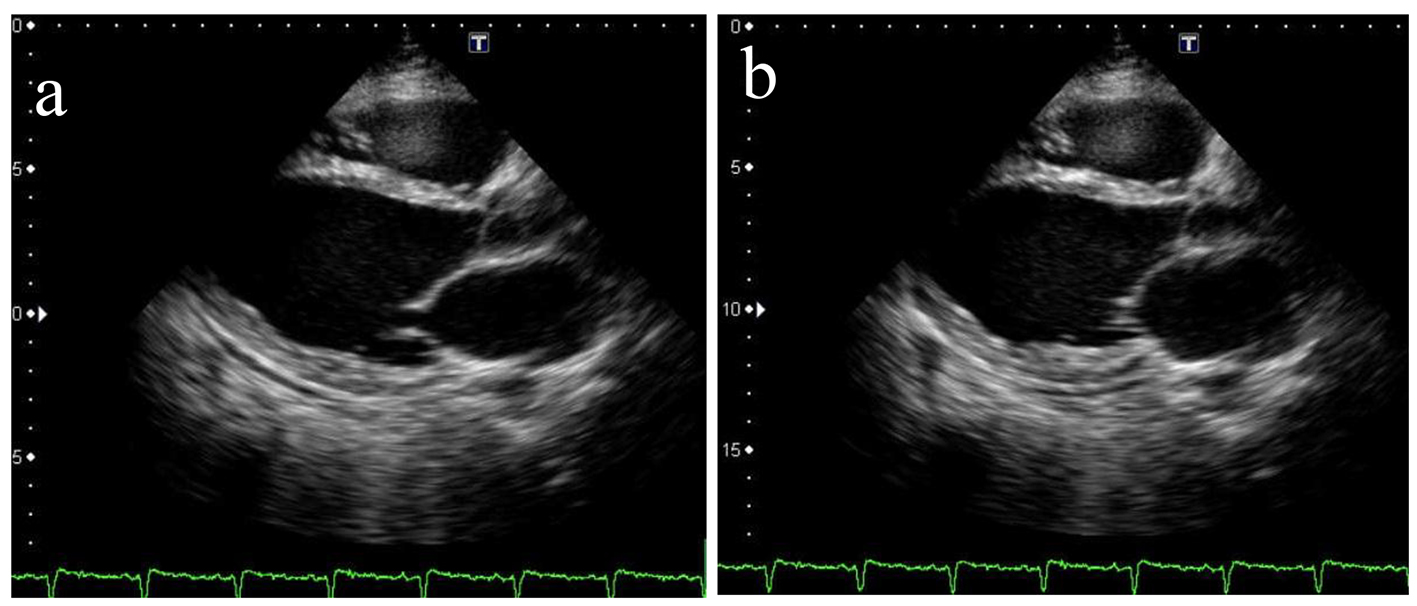 Click for large image | Figure 2. Transthoracic echocardiogram revealed a dilated left ventricle of 63 mm in diastolic phase (a) and 58 mm in systolic phase (b) with a reduced EF of 17%. |
Immediately after admission, diuretic agents, including furosemide and carperitide, were administered. These improved her heart failure with sufficient diuretic effects. On day 6, X-ray revealed disappearance of heart congestion and cardiomegaly (Fig. 3). However, thromboses of 16 × 8 and 29 × 11 mm in her left ventricle were revealed via TTE on day 10 (Fig. 4a, b). Heparin sodium and warfarin potassium were initiated, reducing the thromboses. While her symptoms improved, EF was not restored to normal function. She was discharged on day 40 and an outpatient clinic follow-up was planned.
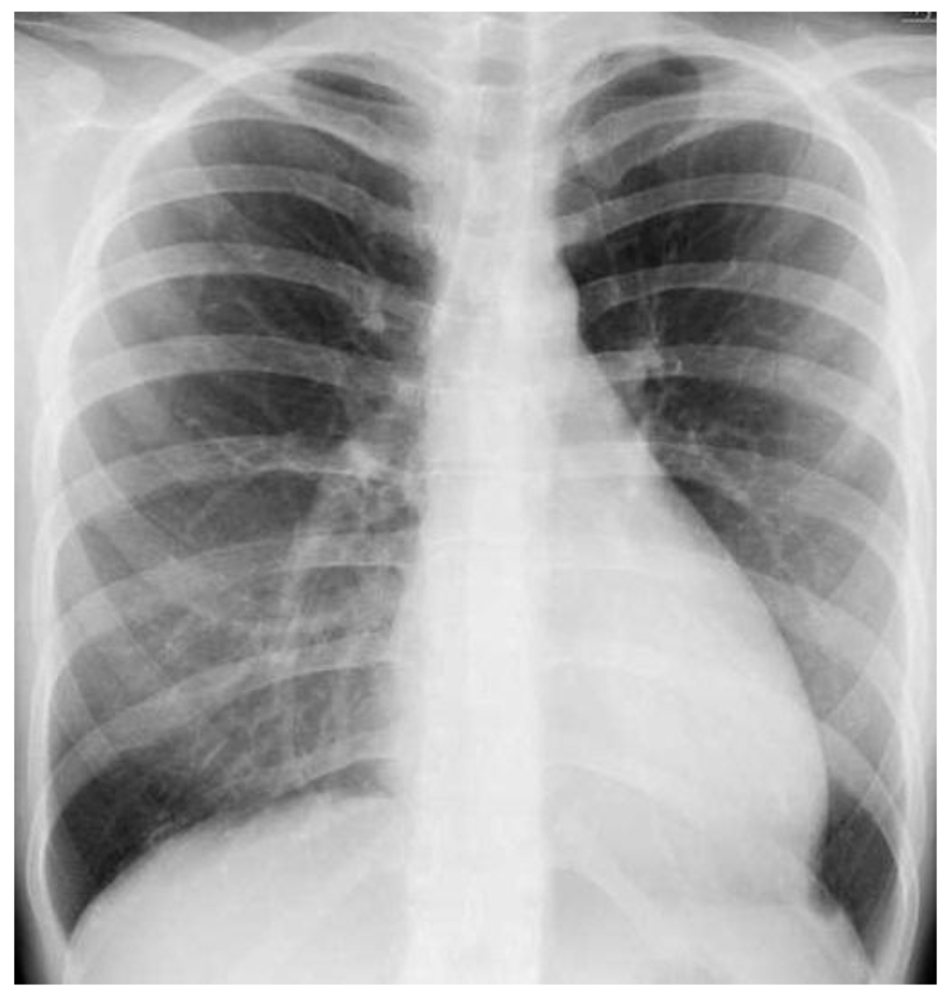 Click for large image | Figure 3. Chest X-ray revealed disappearance of heart congestion and cardiomegaly on day 6. |
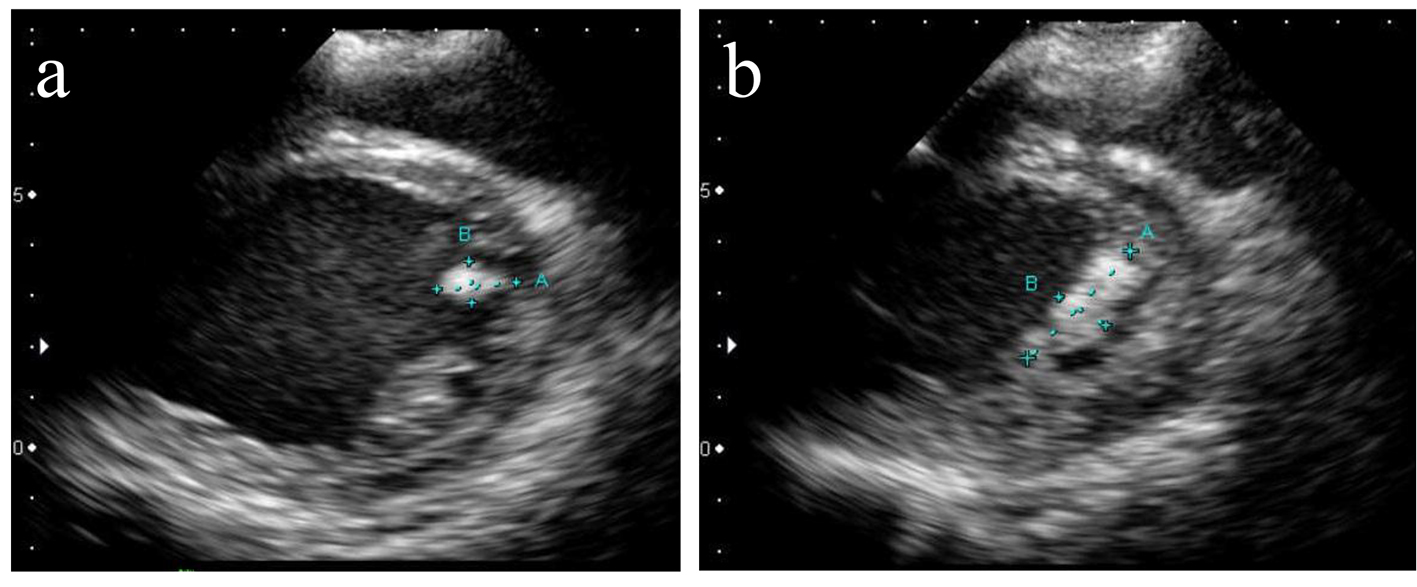 Click for large image | Figure 4. Transthoracic echocardiogram revealed thromboses of 16 × 8 (a) mm and 29 × 11 mm (b) in the patient’s left ventricle on day 10. |
| Discussion | ▴Top |
PPCM is a relatively uncommon cardiology condition which affects perinatal or postnatal women without any cardiac condition. In a US survey conducted between 2004 and 2011, the incidence of PPCM was 1 in 968 births [1], more than the Japanese rate of 1 in 20,000 births [2]. The definition of PPCM includes the following criteria [3]: 1) onset of new congestive heart failure between 1 month before and up to 5 months after; 2) history of cardiac condition, 3) no other causes of heart failure; and 4) LVEF < 45-50%, LV fractional shortening of < 30%, and LV end-diastolic dimension/body mass index of > 27 mm/m2.
Etiology of PPCM is generally unrecognized; however, there are several presumable causes for PPCM, including viral infection, abnormal reactions in the immunology system, circulatory overload accompanied by pregnancy, and endocrine disorders. Considering the difference of incidence between the US and Japan, etiology of PPCM may chiefly depend on ethnicity. With the growing awareness of this disease, the number of cases diagnosed as PPCM is expected to increase. PPCM is also associated with the occurrence of myocarditis or potential dilated cardiomyopathy caused by cardiac overload in prenatal and postnatal period. Recent animal experiments focused on the association with prolactin or angiogenic growth factor [4].
The risk factors of PPCM include a multiple pregnancy, advanced age pregnancy, prolific childbirth, people of African descent, gestational hypertension, history of hypertension, smoking, obesity, and use of tocolytic agents [5]. Among these factors, pregnancy hypertension is the biggest risk factor; approximately 57% of patients with PPCM are reported to have associated pregnancy hypertension, with no difference between races [6]. In 50% of patients with PPCM, cardiac function is restored, whereas 50% of patients have reduced cardiac function. In our case, the patient’s cardiac function did not improve, as observed on the 6-month follow-up. A small number of patients deteriorate and require heart transplant or risk death.
Treatment for PPCM in its acute phase is a standardized strategy for heart failure, including diuretic drugs, beta blockers, catecholamine, and mechanical circulatory support devices (intra-aortic balloon pumping and percutaneous cardiopulmonary support). In its chronic phase, oral drugs, including angiotensin converting enzyme inhibitors, beta blockers, and diuretic drugs, are generally used. In patients with severe and refractory heart failure, heart transplant is required. In some patients with PPCM, immunosuppressive agents and anti-prolactin drugs are attempted. There is no established consensus or guideline on the cessation of medical treatment in the chronic phase.
Seventeen percent of PPCM cases are reported to have associated ventricle thrombus. This may be caused by the hypercoagulable status during the perinatal period or congestive blood flow with reduced cardiac function [3]. Immediate anti-coagulant therapy is effective in reducing the ventricle thrombus [7, 8]. It is unclear whether anti-coagulant therapy is necessary in congestive heart failure patients with a normal sinus rhythm because of hemorrhagic risks; anti-coagulant therapy is recommended for congestive heart failure patients in atrial fibrillation [9]. In patients with PPCM, administration of anti-coagulant agents should be considered to prevent thromboembolic complications due to the hypercoagulable status.
In our case, coagulation test was studied on day 10 when the left ventricle thromboses were evident, revealing elevated levels of plasmin-α2 plasmin inhibitor complex 1.9 μg/mL (normal levels < 0.8 μg/mL) and thrombin-antithrombin complex 3.6 μg/mL (normal levels < 3.0 μg/mL). This result might suggest that the overexpression of plasminogen activator inhibitor-1. Hence, reduction in thromboses in this patient was expected.
In our patient, upper abdominal pain at admission was due to congestive cholestasis. The mechanism of upper abdominal pain in patients with congestive heart failure is to occur mainly from the expansion of hepatic cells by elevated sinusoidal pressure caused by cholestasis [10]. An additional mechanism of congestive heart failure due to gallbladder edema and infection may cause decreased blood flow in cystic artery, leading to acalculous cholecystitis [10]. Not only with imaging modalities but also with clinical symptoms and manifestation, it was crucial to recognize the presence of congestive heart failure in this patient.
Conclusion
PPCM is one of the differential diagnoses in cardiomyopathy that occurs in perinatal or postnatal women. Clinicians should remember that PPCM may be associated with ventricle thrombus caused by the hypercoagulable state in the perinatal period or vascular congestion in reduced cardiac function. They should also remember that PPCM may present gastrointestinal symptoms due to liver congestion.
Conflicts of Interest
The authors declare that there are no conflicts of interest regarding the publication of this paper.
| References | ▴Top |
- Kolte D, Khera S, Aronow WS, Palaniswamy C, Mujib M, Ahn C, Jain D, et al. Temporal trends in incidence and outcomes of peripartum cardiomyopathy in the United States: a nationwide population-based study. J Am Heart Assoc. 2014;3(3):e001056.
doi pubmed - Kamiya CA, Kitakaze M, Ishibashi-Ueda H, Nakatani S, Murohara T, Tomoike H, Ikeda T. Different characteristics of peripartum cardiomyopathy between patients complicated with and without hypertensive disorders. Results from the Japanese Nationwide survey of peripartum cardiomyopathy. Circ J. 2011;75(8):1975-1981.
doi pubmed - Demakis JG, Rahimtoola SH. Peripartum cardiomyopathy. Circulation. 1971;44(5):964-968.
doi - Hilfiker-Kleiner D, Kaminski K, Podewski E, Bonda T, Schaefer A, Sliwa K, Forster O, et al. A cathepsin D-cleaved 16 kDa form of prolactin mediates postpartum cardiomyopathy. Cell. 2007;128(3):589-600.
doi pubmed - Amos AM, Jaber WA, Russell SD. Improved outcomes in peripartum cardiomyopathy with contemporary. Am Heart J. 2006;152(3):509-513.
doi pubmed - Bello N, Rendon IS, Arany Z. The relationship between pre-eclampsia and peripartum cardiomyopathy: a systematic review and meta-analysis. J Am Coll Cardiol. 2013;62(18):1715-1723.
doi pubmed - Kim DY, Islam S, Mondal NT, Mussell F, Rauchholz M. Biventricular thrombi associated with peripartum cardiomyopathy. J Health Popul Nutr. 2011;29(2):178-180.
doi pubmed - Nishi I, Ishimitsu T, Ishizu T, Ueno Y, Suzuki A, Seo Y, Ohtsuka S, et al. Peripartum cardiomyopathy and biventricular thrombi. Circ J. 2002;66(9):863-865.
doi pubmed - Cleland JG, Findlay I, Jafri S, Sutton G, Falk R, Bulpitt C, Prentice C, et al. The Warfarin/Aspirin Study in Heart failure (WASH): a randomized trial comparing antithrombotic strategies for patients with heart failure. Am Heart J. 2004;148(1):157-164.
doi pubmed - Laurila J, Syrjala H, Laurila PA, Saarnio J, Ala-Kokko TI. Acute acalculous cholecystitis in critically ill patients. Acta Anaesthesiol Scand. 2004;48(8):986-991.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


