| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 7, Number 11, November 2016, pages 506-507
Not a Routine Case of Recurrent Cellulitis: Well’s Syndrome
Jeffrey J. Wargo
Department of Internal Medicine, University of Michigan Medical School, 1500 East Medical Center Drive, Ann Arbor, MI 48109, USA
Manuscript accepted for publication October 26, 2016
Short title: Well’s Syndrome
doi: http://dx.doi.org/10.14740/jmc2680w
| Abstract | ▴Top |
When a 28-year-old man with suspected recurrent right forearm cellulitis did not respond to anti-microbial therapy, a dermatological consultation with cutaneous biopsy was obtained. Histopathology along with correlation of his clinical course confirmed a diagnosis of Well’s syndrome (eosinophilic cellulitis) and he was successfully treated with oral anti-histamines and topical corticosteroids. This case emphasizes the importance of consideration for non-infectious etiologies of recurrent cellulitic lesions that do not respond to typical anti-microbial therapy.
Keywords: Well’s syndrome; Eosinophilic cellulitis; Recurrent cellulitis
| Introduction | ▴Top |
Eosinophilic cellulitis, also known as Wells’ syndrome, is a recurrent granulomatous dermatitis associated with peripheral eosinophila [1]. This rare cutaneous condition appears cellulitic, lacks systemic involvement, does not respond to antibiotics, requires a high degree of clinical suspicion to diagnose, and is managed most effectively with oral corticosteroids. With the increasing threat of antibiotic resistance and importance of anti-microbial stewardship, it is imperative to correctly differentiate cellulitis from non-infectious cutaneous conditions, employ a comprehensive differential diagnosis for erythematous plaques, and understand when to perform a skin biopsy to aid with diagnosis. We present a case of Well’s syndrome in a patient admitted to our observation unit for “recurrent cellulitis”.
| Case Report | ▴Top |
Presentation
A 28-year-old man presented with suspected recurrent right forearm cellulitis. The patient had had four episodes of pruritic, edematous, erythematous plaques on the arms and neck over the past 3 months. Each episode lasted for 7 - 10 days and was in a different location. He was treated successfully with antibiotics, but this episode developed while on clindamycin. He had a history of HIV managed with daily emtricitabine, tenofovir, and rilpivirine. His recent CD4 count was 1,204 cells/mm3 with an undetectable viral load. He was started on IV cefazolin in the emergency department and admitted to the observation unit.
Assessment and diagnosis
On admission, he had a temperature of 36.8 °C, blood pressure of 134/77 mm Hg, heart rate of 96 beats per minute, respiratory rate of 15 breaths per minute, and an oxygen saturation of 96% on room air. On his right forearm and inner upper arm, there were several warm erythematous slightly edematous plaques (Fig. 1a). Laboratory analysis was significant for a white blood cell count of 15,200/uL with 80.4% neutrophils and 5% eosinophils. As the patient’s rash did not improve on antibiotics, dermatology was consulted and a biopsy was performed. Histopathology revealed perivascular and interstitial infiltrate with numerous eosinophils and neutrophils, and prominent superficial papillary dermal edema suggesting a diagnosis of Well’s syndrome (eosinophilic cellulitis) (Fig. 1b). The patient was successfully treated with anti-histamines and topical corticosteroids.
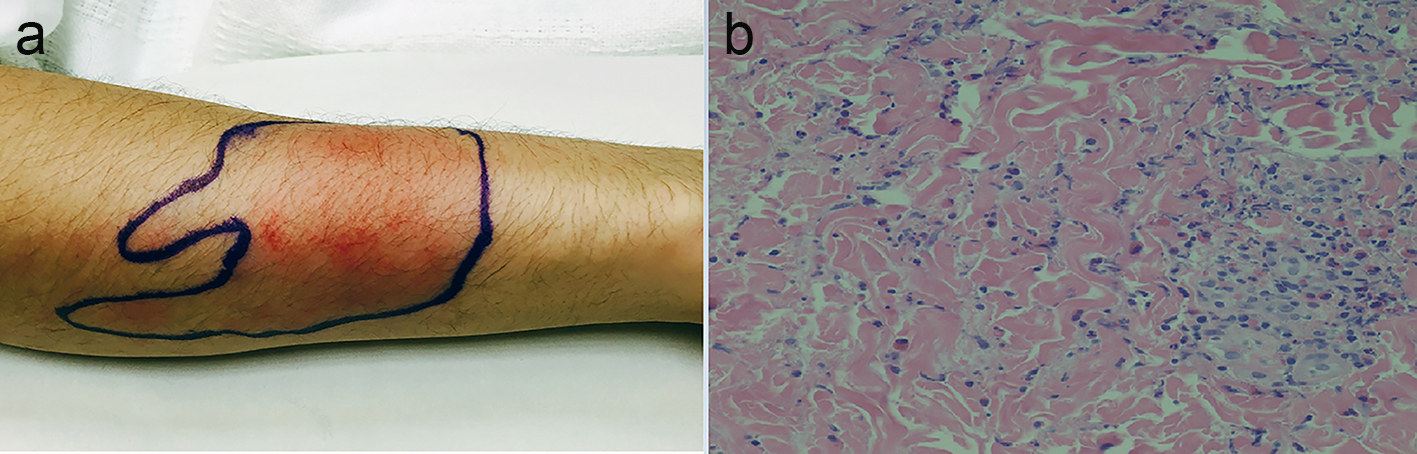 Click for large image | Figure 1. (a) A warm erythematous slightly edematous plaque on the right forearm. (b) Perivascular and interstitial infiltrate with numerous eosinophils, neutrophils, and prominent superficial papillary dermal edema. |
| Discussion | ▴Top |
When a physician is challenged with a case of cellulitis that does not respond to conventional antibiotic therapy, non-infectious etiologies must be considered. After a thorough history, physical, and diagnostic workup has been completed, skin biopsy with histopathology, culture, and direct immunofluorescence may be the only diagnostic option left to secure a diagnosis. In our case, we considered arthropod assault, acute febrile neutrophilic dermatosis, contact dermatitis, Wells’ syndrome, dermal hypersensitivity reaction, urticaria, erythema migrans, toxin-mediated erythema, cellulitis, and drug reactions. Thrombophlebitis, gouty arthritis, familial Mediterranean fever, panniculitis, toxic erythema of chemotherapy, angioedema, and foreign-body reactions represent diseases that commonly masquerade as infectious cellulitis as well [2].
Eosinophilic cellulitis, also known as Wells’ syndrome, was first described in 1971 by Dr. Wells as a recurrent granulomatous dermatitis with eosinophilia [1]. This rare cutaneous condition lacks systemic involvement, does not respond to antibiotics, requires a high degree of clinical suspicion to diagnose, and presents with peripheral eosinophilia in only about 50% of cases [3]. Cutaneous findings appear cellulitic and most typically present with erythematous plaques preceded by pruritis, but blisters, bullae, or nodules may also be seen. Resolution of the lesions occurs in 2 - 8 weeks and may result in hyperpigmentation and skin atrophy resembling morphea [4]. Acute histology reveals tissue edema and a dermal eosinophilic infiltration in a perivascular pattern, while subacute to chronic histology reveals the classic “flame figures” composed of bundles of collagen coated with eosinophils [5]. As flame figures have been associated with other conditions such as Churg-Strauss, spider bites, parasitic infections, follicular mucinosis, and herpes gestationis, a clinical-pathologic approach is required to confirm the diagnosis. Well’s syndrome may be associated with infectious diseases, arthropod assault, malignancy, immunologic disorders, thimerosal-containing vaccines, or medications, but a specific etiology and pathogenesis has not been determined. A literature review of 32 cases of idiopathic eosinophilic cellulitis in 2012 concluded that oral steroids achieved the highest rate of resolution and were 92% effective. In these patients, oral prednisone was typically given 2 mg/kg for 1 week and then tapered over 2 - 3 weeks. Topical steroids and oral anti-histamines were less effective. As recurrence occurs in up to half of cases, treatment of the underlying associated condition (if determined) is imperative, and alternate day low dose prednisone may be indicated.
Conflicts of Interest
There are no conflicts of interest to report.
Funding
None.
| References | ▴Top |
- Wells GC. Recurrent granulomatous dermatitis with eosinophilia. Trans St Johns Hosp Dermatol Soc. 1971;57(1):46-56.
pubmed - Falagas ME, Vergidis PI. Narrative review: diseases that masquerade as infectious cellulitis. Ann Intern Med. 2005;142(1):47-55.
doi - Caputo R, Marzano AV, Vezzoli P, Lunardon L. Wells syndrome in adults and children: a report of 19 cases. Arch Dermatol. 2006;142(9):1157-1161.
doi pubmed - Sinno H, Lacroix JP, Lee J, Izadpanah A, Borsuk R, Watters K, Gilardino M. Diagnosis and management of eosinophilic cellulitis (Wells' syndrome): A case series and literature review. Can J Plast Surg. 2012;20(2):91-97.
doi pubmed - Beer TW, Langtry JA, Phillips WG, Wojnarowska F. Flame figures in bullous pemphigoid. Dermatology. 1994;188(4):310-312.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


