| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 2, Number 3, June 2011, pages 107-109
An Orient Triad With Hepatitis B Related Cirrhosis, Hydatid Cyst and Brucellosis: A Case Report
Ahmet Cumhur Dulgera, Ozgur Kemikb, Huseyin Begenikc, d, Habib Emrec, Fatih Mehmet Erdurc, Rafet Metea
aYuzuncu Yil University School of Medicine, Gastroenterology, Van, Turkey
bYuzuncu Yil University School of Medicine, General Surgery, Van, Turkey
cYuzuncu Yil University School of Medicine, Internal Medicine, Van, Turkey
dCorresponding author: Huseyin Begenik, Yuzuncu Yil University Medical Faculty, Internal Medicine, Van, Turkey
Manuscript accepted for publication March 15, 2011
Short title: Cirrhosis, Hydatid Cyst and Brucellosis
doi: https://doi.org/10.4021/jmc169w
| Abstract | ▴Top |
In many ways, diagnostic problems of the liver are different in Asian patients from those in western patients. Hepatitis B virus infection plays a major role for chronic liver disease worldwide as well as Turkey. One of the most feared complications of chronic hepatitis B is liver cirrhosis. Hydatid disease of the liver is one of the most common clinical problems in developing countries. Usually, the diagnosis is made by serology with ultrasonography. As a zoonotic disease, brucellosis can be coexisted with any of a number of clinical pictures and may mimic a variety of diseases. All of these different diseases may rarely present in the same patient. So, we report an unusual case of hydatide disease with hepatitis B-related cirrhosis and brucellosis. Thus, we reviewed many critical issues on this case report on the role of diagnostic approaches and management.
Keywords: Hepatitis B related cirrhosis; Hydatid cyst; Brucellosis
| Introduction | ▴Top |
Approximately 350 million people are chronically infected with Hepatitis B virus (HBV) worldwide [1]. As the hepatitis B patients increase in number, more people are at risk for developing cirrhosis. The hallmarks of cirrhosis are splenomegaly, thrombocytopenia and prolonged prothrombine time. A liver biopsy is usually required for determining the evidence of fibrosis as well as cirrhosis in patients with either increased alanine aminotransferase (ALT) or HBV DNA levels [2].
Ingestion of the dog tapeworm Echinococcus granulosus may cause hydatide disease and is frequently diagnosed as a liver mass. Man is located as intermediate hosts for the cycle of Echinococcus granulosus infection. Hydatid disease remains endemic in northern hemisphere as well as eastern part of Turkey [3].
Brucellosis is a zoonosis and is caused by small, gram negative and oxidase- and urease-positive coccobacilli. It can affect any human organ or system and can cause severe human disease [4]. This disease is widely seen in the world. Turkey is also an endemic area for brucellosis. The number of annual cases of human brucellosis in Turkey is approximately 15,000 [5].
Hepatitis B-related liver cirrhosis, hydatid disease and brucellosis are endemic diseases for Mediterranean basin. They may share same environmental routes of transmission. Herein, we report a Turkish patient who co-infected by hepatitis B, echinococcus multilocularis and brucella melitensis. Therapeutic strategies are also discussed.
| Case Report | ▴Top |
A 50-year-old man was admitted to this hospital because of abdominal pain, nocturnal fever and vertigo. The patient was born in eastern part of Turkey and had been working in a village as a farmer. There was no family history of liver disease. The patient was taking paracetamol and had no known allergies.
On examination, the blood pressure was 159/94 mm Hg; the pulse rate was 65 per minute; his temperature was 38.1 °C. Tenar atrophy and palmary erythema were evident. The abdomen was soft, with mild, diffuse tenderness on palpation in the right upper quadrant, and there was mild splenomegaly. The lungs were clear to auscultation. The remainder of the physical examination was normal.
Laboratory examinations showed the following results: hemoglobin 15.4 g/dl, white cell count 3.3 × 109/L, platelet count 80.0 × 109/L, sedimentation rate 35/hour, C-reactive protein level 24 (normal 0 to 5), ALT 91 IU/L (normal 5 to 38), aspartate aminotransferase (AST) 73 IU/L (normal 9 to 44), alkaline phosphatase 202 IU/L (normal 90 to 279), gamma glutamyl transpeptidase 101 IU/L (normal 0 to 48), albumin 4.3 mg/dl, globulin 3.3 mg/dl, prothrombin time (PT) 15 s (control 12 s) and alpha fetoprotein 6.93 ng/dl (normal 0 to 9).
The enzyme immunoassay for testing for antibodies to E. granulosus was positive at a value of 1.146 (96% sensitivity and 75% specificity at values greater than 0.5). The patient’s hepatitis B surface antigen was positive and hepatitis e antigen was negative and his HBV-DNA level was 1,340,000 IU/ml. Test results for hepatitis delta virus and for other hepatotrophic viruses were negative. Wright agglutination test for brucellosis was also positive.
An abdomen ultrasonography revealed parancyhmal heterogeneity of the liver associated with cystic mass which was 12 × 10 × 7 cm in diameter. Computerized tomography (CT) of abdomen demonstrated a 12 × 10 × 7 cm multiple loculated cyst with daughter cysts in the right lobe of the liver (Fig. 1). There was associated caudate lobe hypertrophy, splenomegaly and enlarged portal vein. On the day of admission, an upper gastrointestinal system endoscopy demonstrated second-degree esophageal varices. Percutanous biopsy of the liver following correction of coagulopathy and thrombocytopenia was consistent with the diagnosis of advanced liver fibrosis as well as cirrhosis.
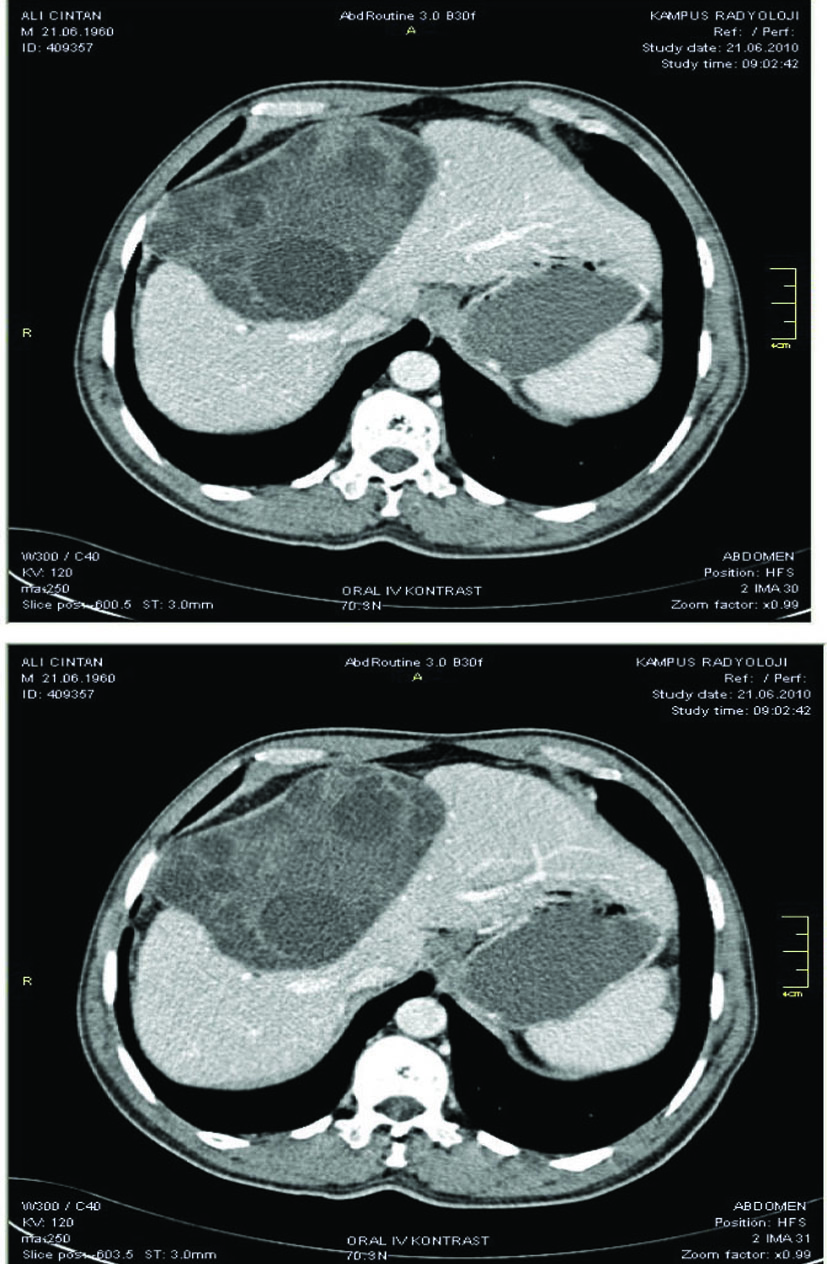 Click for large image | Figure 1. Computerized tomography (CT) of abdomen demonstrated a 12 × 10 × 7 cm multiple loculated cyst with daughter cysts in the right lobe of the liver. |
Tenofovir disoproxil (245 mg/day) was started as antiviral treatment for chronic hepatitis B. In collaboration with the infectious disease, he received albendazole for hydatide disease, and ciprofloxacine and doxycycline for brucellosis. He continued to receive albendazole for nearly 45 days, at the end of the course, the patient was well and there were no constitutional symptoms.
| Discussion | ▴Top |
This report describes for the first time a large liver hydatide cyst associated with hepatitis B-related liver cirrhosis and brucellosis. Human cystic echinococcosis (hydatid disease) is a helminthic cyst-forming disease of human and is caused by infection with the tapeworm E. granulosus [6].
In the definitive canine host, the adult cestode locates in the intestine, and its eggs, or oncospheres, are liberated into the feces. These eggs which ingested by an intermediate host such as human penetrate the intestinal wall and migrate to the liver via portal vein. In the liver, trapped oncospheres (eggs) develop by vesiculation and produce protoscolices. Oncosphere containing tissue endorses the development of metacestode, or hydatid cyst. Components of the hydatid cyst wall are host-derived external adventitial layer, intermediate acellular layer and worm-derived internal germinal layer. Approximately 70 percent of cysts develop in the liver, lung cysts account for 20 percent of cases [7].
Radiologic techniques (e.g., CT, magnetic resonance imaging, ultrasound) are the best techniques to detect the space occupying cysts or lesions caused by the Echinococcus granulosus [8, 9].
Furthermore, ELISA and indirect hem agglutination assays are the most useful diagnostic tools to determine the disease as well as to assess the viability of cysts. In case of involvement of the liver, sensitivity of the serologic tests is reported as substantially higher [10-13].
The possible approaches for treating the hepatic hydatid cyst include antihelmintic chemotherapy, percutaneous drainage, and surgical resection [12]. The findings of physical and laboratory examination, abdominal imaging, endoscopy and liver biopsy revealed hepatitis B-related cirrhosis in presented case.
In presented case, we preferred nonsurgical approach to treat him because of paranchymal liver disease. So, we started with albendazole, 10 mg/kg/day for at least three to six months. Half-life of albendazole is significantly prolonged by liver disease. So, close follow-up with laboratory studies is needed to determine hepatotoxicity and neutropenia in patients who are taking albendazole. For these reasons, we closely observed this patient by the end of treatment and no drug toxicity detected [14].
The differential diagnosis for nocturnal fever associated with higher sedimentation rate in cirrhotic patients who have a liver mass may be due to paraneoplastic syndrome as well as systemic infections [15].
In this patient, no alpha-feto protein elevation was observed, and there was lack of radiologic features of the hepatocellular carcinoma. Furthermore, seropositivity for E. granulosus and radiologic features of the liver mass were consistent with type III hydatid cyst as well.
Striking features of this patient’s presentation were the recent development of nocturnal fever, relative leucopenia and higher sedimentation and C-reactive protein levels. These findings may be seen in cirrhotic patients who have variceal hemorrhage, ascites, spontaneous bacterial peritonitis, or hepatic encephalopathy [16].
In presented case, the common complications of cirrhosis were not considered likely. It is important to recognize these infectious agents as causes of splenomegaly and relative leukopenia, because they must be considered in the differential diagnosis of fever in cirrhotic patients. Both the cirrhosis and brucellosis are characterized by higher sedimentation and CRP levels and both conditions have been associated with splenomegaly and leucopenia [4].
In the course of hydatide disease, cyst rupture into the biliary tree with secondary cholangitis may cause fever. Diagnosis of perforation is usually made by CT scan, although ultrasonography may be helpful [6].
However, in this case, abdomen CT did not reveal perforation. Furthermore, no objective evidence of perforated cyst was seen (eosinophilia, icterus and severe pain on right upper abdomen). Additionally, the patient’s initial blood culture was positive for brucellosis. In our patient, brucellosis and hydatide disease were likely to account for the development the symptoms and findings.
The co-infection of Echinococcus with brucella in a patient with cirrhosis due to Hepatitis B virus (HBV) infection is a very rare clinical picture that has probably never been reported in medical literature. It can be concluded from this case report that multidisciplinary approach enhances treatment efficacy particularly in patients with hydatide disease.
| References | ▴Top |
- EASL Clinical Practice Guidelines: management of chronic hepatitis B. J Hepatol 2009;50(2):227-242.
pubmed doi - Mani H, Kleiner DE. Liver biopsy findings in chronic hepatitis B. Hepatology 2009;49(5 Suppl):S61-71.
pubmed doi - Craig PS, McManus DP, Lightowlers MW, Chabalgoity JA, Garcia HH, Gavidia CM, Gilman RH, et al. Prevention and control of cystic echinococcosis. Lancet Infect Dis 2007;7(6):385-394.
pubmed doi - Pappas G, Akritidis N, Bosilkovski M, Tsianos E. Brucellosis. N Engl J Med 2005;352(22):2325-2336.
pubmed doi - Pappas G, Papadimitriou P, Akritidis N, Christou L, Tsianos EV. The new global map of human brucellosis. Lancet Infect Dis 2006;6(2):91-99.
pubmed doi - McManus DP, Zhang W, Li J, Bartley PB. Echinococcosis. Lancet 2003;362(9392):1295-1304.
pubmed doi - Shantz PM. Echinococcosis. In: Geurrant RL, Walker DH, Weller PF, eds. Tropical infectious diseases: principles, pathogens & practice. Vol.2. Philadelphia: Churchill Livingstone. 1999;1005-1025.
- Caratozzolo M, Scardella L, Grossi G, et al. Diagnostic approach of abdominal hydatidosis by ultrasonography. Arch Hidatid 1991;30:531.
- Raether W, Hanel H. Epidemiology, clinical manifestations and diagnosis of zoonotic cestode infections: an update. Parasitol Res 2003;91(5):412-438.
pubmed doi - Eckert J, Deplazes P. Biological, epidemiological, and clinical aspects of echinococcosis, a zoonosis of increasing concern. Clin Microbiol Rev 2004;17(1):107-135.
pubmed doi - Lorenzo C, Ferreira HB, Monteiro KM, Rosenzvit M, Kamenetzky L, Garcia HH, Vasquez Y, et al. Comparative analysis of the diagnostic performance of six major Echinococcus granulosus antigens assessed in a double-blind, randomized multicenter study. J Clin Microbiol 2005;43(6):2764-2770.
pubmed doi - Dunn M. Parasitic diseases. In: Schiff ER, Sorrell MF, Maddrey WC, eds. Diseases of the liver, 9th ed. Philadelphia: Lippincott Williams&Wilkins. 2003;1509.
- Babba H, Messedi A, Masmoudi S, Zribi M, Grillot R, Ambriose-Thomas P, Beyrouti I, et al. Diagnosis of human hydatidosis: comparison between imagery and six serologic techniques. Am J Trop Med Hyg 1994;50(1):64-68.
pubmed - Opatrny L, Prichard R, Snell L, Maclean JD. Death related to albendazole-induced pancytopenia: case report and review. Am J Trop Med Hyg 2005;72(3):291-294.
pubmed - Yang YY, Lin HC. Bacterial infections in patients with cirrhosis. J Chin Med Assoc 2005;68(10):447-451.
pubmed doi - Schuppan D, Afdhal NH. Liver cirrhosis. Lancet 2008;371(9615):838-851.
pubmed doi
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


