| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 4, Number 6, June 2013, pages 416-419
Possible Cefcapene Pivoxil- or Clarithromycin-Induced Severe Hyperglycemia in a Patient With Type 2 Diabetes: A Case Report
Yoji Miyoshia, b
aDivision of Endocrinology, Diabetes and Metabolism, Sayama General Clinic, Japan
bCorresponding address: Division of Endocrinology, Diabetes and Metabolism, Sayama General Clinic, 4-15-25 Irumagawa, Sayama, Saitama 350-1305, Japan
Manuscript accepted for publication April 25, 2013
Short title: Antibiotics-Induced Hyperglycemia
doi: https://doi.org/10.4021/jmc1274w
| Abstract | ▴Top |
There are various reasons for the deterioration of glycemic control observed in patients with diabetes, one of which is drug-induced hyperglycemia. Antibiotics, especially the fluoroquinolones, have been reported to be associated with glucose disturbances. However, induction of hyperglycemia by cephem or macrolide antibiotics has rarely, if ever, been reported. Here, we report the case of possible antibiotics-induced severe hyperglycemia in a patient with type 2 diabetes. A 67-year-old Japanese diabetic man, who was not using oral hypoglycemic agents or insulin but whose condition was controlled with diet and exercise, presented at an otolaryngology clinic with nasal discharge and rhinorrhea. His glycosylated hemoglobin (HbA1c) level had been stable at 6.6-7.2% for several years. He was diagnosed with acute sinusitis and given an oral cephem antibiotic, cefcapene pivoxil, for 1 week. His otolaryngeal symptoms were slight and disappeared soon. Thereafter, therapy was switched to a macrolide antibiotic, clarithromycin, for 3 weeks. Twenty-five days after the initiation of antibiotic therapy, severe hyperglycemia was pointed out; his random serum glucose and HbA1c levels were 29.4 mmol/L and 10.6%, respectively. The patient required insulin and oral hypoglycemic agent therapy. The Naranjo probability scale suggests that the relationship between the administration of cefcapene pivoxil or clarithromycin and the patient’s severe hyperglycemia might be possible. To the best of our knowledge, there has been no previous report of a deterioration in glycemic control in a patient with diabetes administered a cephem (cefcapene pivoxil) or macrolide (clarithromycin) antibiotic. Considering the global prescription of cephem and macrolide antibiotics, awareness of the fact that some patients are at high risk for impaired glucose tolerance is important when prescribing antibiotics. Further studies are warranted to determine the incidence rate of hyperglycemia among patients with diabetes who are administered cephem and macrolide antibiotics.
Keywords: Cefcapene pivoxil; Clarithromycin; Drug-induced hyperglycemia; Type 2 diabetes
| Introduction | ▴Top |
Various factors can cause the sudden deterioration of glycemic control in patients with diabetes, one of which is drug-induced hyperglycemia [1]. Antibiotics, especially the fluoroquinolones, have been reported to be associated with alterations in glycemic control among patients with diabetes as well as those without diabetes [2-5]. However, cephem or macrolide antibiotics have rarely, if ever, been reported to induce hyperglycemia.
We herein report the case of a patient with diabetes who developed severe hyperglycemia following treatment with a cephem antibiotic, cefcapene pivoxil hydrochloride (CFPN-PI), and a macrolide antibiotic, clarithromycin (CAM), for acute sinusitis.
| Case Report | ▴Top |
The patient was a 67-year-old Japanese man with diabetes and hypertension (height, 172 cm; weight, 66 kg). He also had a history of coronary artery disease as he had suffered a myocardial infarction and undergone percutaneous coronary intervention 5 years previously. His medications included enalapril maleate 2.5 mg/day (an ACE inhibitor), ticlopidine hydrochloride 100 mg twice daily (an anticoagulant), and rebamipide 100 mg twice daily (a stomachic). His cardiac function was stable and he had not felt any cardiac symptoms for several years. Although he had diabetes, he had never taken any medications for diabetes, but instead had controlled his condition with diet and exercise. Over the past several years, his random serum glucose levels were between 5.83 and 9.66 mmol/L, and his glycosylated hemoglobin (HbA1c, NGSP) level had been stable at 6.6-7.2% (Fig. 1).
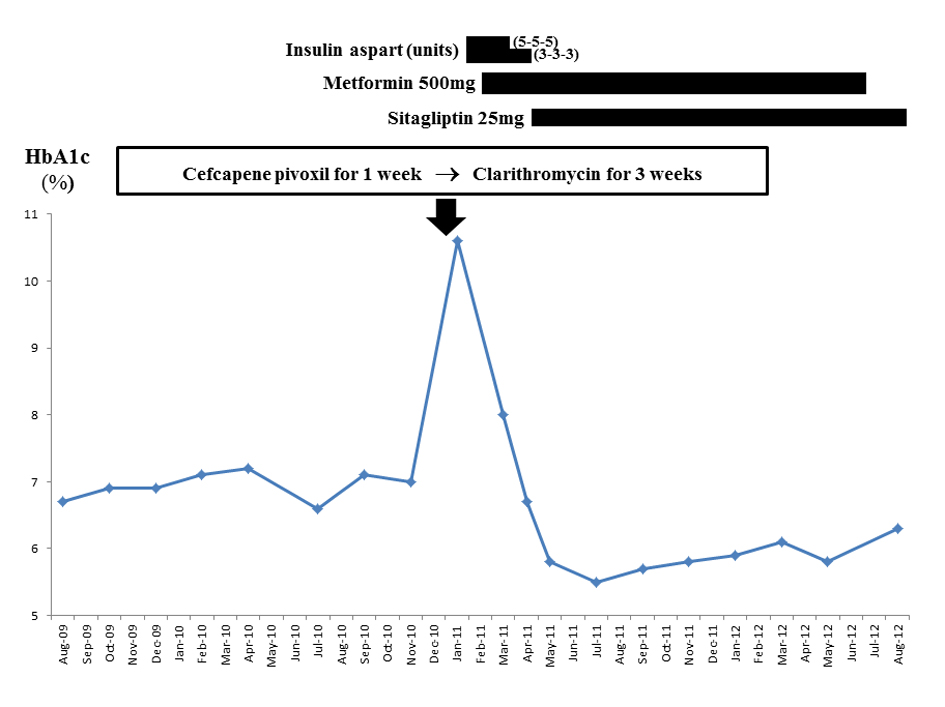 Click for large image | Figure 1. Clinical course. On December 20, 2010, the patient was administered an oral antibiotic, cefcapene pivoxil hydrochloride (CFPN-PI) 100 mg 3 times a day for 1 week. One week later, he was switched to clarithromycin (CAM) 200 mg/day for 3 weeks (arrow). His glycosylated hemoglobin (HbA1c, NGSP) level deteriorated from 7.0% on November 19, 2010, to 10.6% on January 14, 2011. Subcutaneous administration of insulin aspart was initiated at a dose of 5 units before every meal on January 28, 2011. Thereafter, his HbA1c level was markedly improved. The dose of insulin was decreased and the oral hypoglycemic agents (metformin 500 mg/day and sitagliptin 25 mg/day) were administered. In August 2012, his HbA1c level was 6.3% without insulin and metformin. No deterioration in glycemic control was observed at the 2-year follow-up visit. |
In December 2010, the patient presented at an otolaryngology clinic with symptoms of nasal discharge and rhinorrhea. He was diagnosed with acute sinusitis and administered oral CFPN-PI on December 20, 2010. Although his otolaryngeal symptoms were slight and disappeared a few days after taking CFPN-PI, he was switched to CAM on December 27, 2010, when he experienced a sudden onset of thirst and pollakiuria. Eighteen days later (on January 14, 2011), he was diagnosed with hyperglycemia and referred to our endocrinology clinic for an evaluation of the sudden deterioration in serum glucose levels. At this point, his random serum glucose level was 29.4 mmol/L and his HbA1c level was 10.6%. Other laboratory findings were as follows: blood urea nitrogen, 4.2 mmol/L (reference, 2.9 - 7.1); serum creatinine, 73.3 mmol/L (reference, 54.0 - 92.0); plasma beta-hydroxybutyric acid, 97 mmol/L (reference, < 76); random serum C-peptide, 0.80 nmol/L. An anti-glutamic acid decarboxylase antibody test was negative. His serum C-reactive protein (CRP) level and white blood cell (WBC) count were less than 0.48 nmol/L (reference, < 2.86) and 4.63 × 109/L (reference, 3.3 - 9.0), respectively. Although the patient’s sinusitis symptoms had disappeared a few days after the initiation of antibiotic therapy, his serum glucose readings ranged from 22.2 to 27.8 mmol/L. Thus, the patient required insulin and oral hypoglycemic agents (Fig. 1).
| Discussion | ▴Top |
It is common to encounter cases of deterioration of glycemic control among patients with type 2 diabetes. Although CFPN-PI or CAM might be considered a possible cause, the other factors also should be taken into consideration. Various factors affect glycemic control, including deteriorations in the living environment of the surrounding area, other diseases, physical stress induced by infection [6, 7], and drugs [1].
In our case, no changes in the patient’s living environment had occurred at that point in time. He had no pertinent history of alcohol or tobacco use. He drank Japanese tea, but not sweet beverages, eliminating the possibility of soft-drink ketosis. Extensive investigations confirmed that no diseases of the liver, pancreas, or gastrointestinal system were present (data not shown). The stress by infection is a known cause of hyperglycemia [6, 7]. However, the patient’s otolaryngeal symptoms were slight, and they improved rapidly a few days after CFPN-PI administration. About 3 weeks after the improvement of symptoms, severe hyperglycemia was recognized (on January 14, 2011), when markers of inflammation (CRP and WBC) were within normal limits. Thus, it is unlikely that a stress-induced phenomenon led to the marked hyperglycemia observed in our patient. Drug-induced hyperglycemia thus remains a possibility [1]. Disorders of glucose metabolism have been associated with a number of drugs, including antibiotics, corticosteroids, and antipsychotic agents. Our patient’s medications (enalapril, ticlopidine, and rebamipide) are unlikely to inhibit glucose homeostasis because the patient had been taking these medications on a regular basis for several years prior to his developing severe hyperglycemia.
Antibiotics, especially fluoroquinolones (gatifloxacin, levofloxacin, etc), have been reported to cause abnormalities in blood glucose homeostasis, such as hypoglycemia and hyperglycemia [2-5, 8]. In vitro studies showed that some fluoroquinolones can block ATP-sensitive potassium channels of pancreatic β-cells and stimulate insulin secretion, leading to hypoglycemia [9, 10]. On the other hand, Yamada et al. showed that chronic treatment with gatifloxacin decreases islet insulin content by inhibiting insulin biosynthesis [11]. Ishiwata et al. showed that levofloxacin [8] and gatifloxacin [12] associated histamine releases can lead to increased serum epinephrine concentrations and hyperglycemia in rats. These findings suggest that fluoroquinolones can induce hyperglycemia by several mechanisms. Thus, the accurate mechanisms by which antibiotics induce hyperglycemia remain to be determined. Considering the worldwide prescription of CFPN-PI and CAM, it may be prudent to use these antibiotics with caution in patients with diabetes.
Our patient’s clinical course was characteristic. A few days after the initiation of antibiotic therapy, the patient’s otolaryngeal symptoms disappeared, whilst he had a sudden onset of thirst and pollakiuria. It seems to be associated with the fact that an antibiotic-induced hyperglycemia often takes several days to develop [2, 11]. His intrinsic insulin secretion was not depleted and he had no ketosis, suggesting the deterioration of insulin resistance. The relationship between the administration of CFPN-PI or CAM and our patient’s subsequent development of hyperglycemia might be possible, as measured by the Naranjo probability scale [13].
In conclusion, we have presented the case of a patient with diabetes who developed severe hyperglycemia following antibiotic treatments. To the best of our knowledge, there has been no previous report of a deterioration in glycemic control in a patient with diabetes administered a cephem (CFPN-PI) or macrolide (CAM) antibiotic. Whether the initiation of antibiotic therapy itself or other factors precipitated the severe hyperglycemia is unknown. Further studies are warranted to determine the incidence rate of hyperglycemia among patients with diabetes who are administered cephem and macrolide antibiotics. In addition, further evaluation is needed to establish the mechanisms for precipitation of hyperglycemia in patients treated with antibiotics.
Acknowledgments
We wish to thank Dr. Satoshi Katayama for expert advice regarding antibiotics for acute sinusitis.
Competing Interests
The author declares that he has no competing interests.
Abbreviations
HbA1c: glycosylated hemoglobin; CFPN-PI: cefcapene pivoxil hydrochloride; CAM: clarithromycin; ACE: angiotensin-converting enzyme; CRP: C-reactive protein; WBC: white blood cell
| References | ▴Top |
- Pandit MK, Burke J, Gustafson AB, Minocha A, Peiris AN. Drug-induced disorders of glucose tolerance. Ann Intern Med. 1993;118(7):529-539.
doi pubmed - Park-Wyllie LY, Juurlink DN, Kopp A, Shah BR, Stukel TA, Stumpo C, Dresser L, et al. Outpatient gatifloxacin therapy and dysglycemia in older adults. N Engl J Med. 2006;354(13):1352-1361.
doi pubmed - Biggs WS. Hypoglycemia and hyperglycemia associated with gatifloxacin use in elderly patients. J Am Board Fam Pract. 2003;16(5):455-457.
doi pubmed - Arce FC, Bhasin RS, Pasmantier R. Severe hyperglycemia during gatifloxacin therapy in patients without diabetes. Endocr Pract. 2004;10(1):40-44.
pubmed - Donaldson AR, Vandiver JR, Finch CK. Possible gatifloxacin-induced hyperglycemia. Ann Pharmacother. 2004;38(4):602-605.
doi pubmed - McCowen KC, Malhotra A, Bistrian BR. Stress-induced hyperglycemia. Crit Care Clin. 2001;17(1):107-124.
doi - Losser MR, Damoisel C, Payen D. Bench-to-bedside review: Glucose and stress conditions in the intensive care unit. Crit Care. 2010;14(4):231.
doi pubmed - Ishiwata Y, Itoga Y, Yasuhara M. Effect of levofloxacin on serum glucose concentration in rats. Eur J Pharmacol. 2006;551(1-3):168-174.
doi pubmed - Maeda N, Tamagawa T, Niki I, Miura H, Ozawa K, Watanabe G, Nonogaki K, et al. Increase in insulin release from rat pancreatic islets by quinolone antibiotics. Br J Pharmacol. 1996;117(2):372-376.
doi pubmed - Saraya A, Yokokura M, Gonoi T, Seino S. Effects of fluoroquinolones on insulin secretion and beta-cell ATP-sensitive K+ channels. Eur J Pharmacol. 2004;497(1):111-117.
doi pubmed - Yamada C, Nagashima K, Takahashi A, Ueno H, Kawasaki Y, Yamada Y, Seino Y. Gatifloxacin acutely stimulates insulin secretion and chronically suppresses insulin biosynthesis. Eur J Pharmacol. 2006;553(1-3):67-72.
doi pubmed - Ishiwata Y, Yasuhara M. Gatifloxacin-induced histamine release and hyperglycemia in rats. Eur J Pharmacol. 2010;645(1-3):192-197.
doi pubmed - Naranjo CA, Busto U, Sellers EM, Sandor P, Ruiz I, Roberts EA, Janecek E, et al. A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther. 1981;30(2):239-245.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


