| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 4, Number 6, June 2013, pages 385-388
Strychnine Intoxication: A Case Report
Ana Lagesa, e, João Pinhob, Ricardo Alvesa, Carlos Capelac, Esmeralda Lourençob, Luís Lencastred
aInternal Medicine Department, Hospital de Braga, Portugal
bNeurology Department, Hospital de Braga, Portugal
cEmergency Department, Hospital de Braga, Portugal
dIntensive Care Unit, Hospital de Braga, Portugal
eCorresponding author: Ana Lages, Internal Medicine Department, Hospital de Braga, Sete Fontes, Sao Victor, 4710-243 Braga, Portugal
Manuscript accepted for publication March 20, 2013
Short title: Strychnine Intoxication
doi: https://doi.org/10.4021/jmc1189w
| Abstract | ▴Top |
Strychnine acts as an inhibitor of post-synaptic neuronal inhibition and intoxication leads to distinct clinical manifestations which may culminate in death. Since its commercialization is prohibited in most countries, cases of strychnine intoxication are now rare. We present a case of an elderly patient who voluntarily ingested a white powder thought to be strychnine. He developed myoclonus, startle response, and episodes of generalized muscle contractions accompanied by respiratory arrest in one occasion. Diazepam, valproic acid and supportive treatments were able to control manifestations, however the patient died after 2 days. Our aim is to alert clinicians that, despite its rarity, strychnine intoxication may still be seen in emergency departments, and clinical outcome can be influenced by rapid recognition and timely institution of adequate treatment.
Keywords: Strychnine; Intoxication; Glycine antagonist; Generalized muscle contractions; Startle.
| Introduction | ▴Top |
Strychnine, a white powder alkaloid derived from the seeds of the tree Strychnos nux-vomica, has had its use, throughout history, as an antiseptic, stomach tonic, circulatory and central nervous system stimulant and, more recently, as a poison for animal control [1]. In the European Union, where it had its use as a rodenticide, authorities have prohibited its sale in 2003 and recalled all supplies in 2006. Nevertheless, rare intoxication (accidental or deliberated) reports due to strychnine continue to be published in medical literature, some with the patient being discharged alive [2, 3]. Pharmacologically it is a competitive antagonist of glycine, an important inhibitory neurotransmitter in the ventral horns of the spinal cord, brainstem, and higher centers [4]. It undergoes extensive metabolism by hepatic cytochrome P-450 2B, has a biological half-life of 10 - 12 hours, and up to 20% is excreted unchanged in the urine within 24 hours [5]. Despite its rarity, strychnine intoxication distinct manifestations should not be forgotten. This is especially true for clinicians working in the emergency department, since rapid identification and supportive treatment may prevent significant morbidity and mortality [2].
| Case Report | ▴Top |
We present the case of an 87-year-old white male, brought to the emergency department by his family after a suspected ingestion of strychnine. The patient was a retired forest ranger and had no previous history of mental illness. His past medical history was significant for chronic kidney disease, hyperuricemia, diabetes mellitus, and osteoarthritis. His medications included gliclazide, allopurinol, alprazolam, cobamamide and glucosamine. At admission, he had no complaints, denied any type of poison ingestion and asked to be discharged. When questioned, the patient admitted possessing a bottle of strychnine powder for about twenty years. His daughter insisted that she had seen him ingesting a small amount of a white powder after a familial dispute. Presenting vital signs and physical examination were significant only for anxiety and paroxysmal jerky movements of the extremities. Admission blood tests results are shown in Table 1.
 Click to view | Table 1. Blood Tests Results |
The patient was kept under observation and 12 hours after white powder ingestion, while being repositioned in bed, he developed a series of powerful repetitive generalized tonic muscle contractions with preserved consciousness, culminating in respiratory arrest. Contractions resolved after IV administration of 10 mg of diazepam and bag-valve-mask ventilation. Progressive recovery of consciousness was observed. He was transferred to an intermediate care unit. By then the patient was fully awake and orientated, restless, with adequate speech and generalized hyperreflexia. An exuberant generalized startle response could be elicited by minimal tactile and auditory stimuli. Each startle response elicited a series of repetitive generalized extension tonic muscle contractions, prominent trismus and facial muscles contraction, with apparent preserved consciousness, accompanied by transient desaturation and difficult spontaneous ventilation, without the need of ventilation support. These episodes were self-limited, resolved more quickly and were less frequent if the patient was maintained in a low light, sound and movement ambiance. Analytical study showed lactic acidosis, slightly elevated myoglobin and white cell count - see Table 1 (Day 1) for more detail. Brain CT scan was unremarkable. Symptomatic treatment with sodium valproate, initial dose of 750 mg, followed by a 1,600 mg (1 mg/kg/h) 24 h perfusion, led to termination of the muscle contractions. Elevated myoglobin and lactic acidosis were managed with fluid therapy. Reduction of frequency and intensity of the startle response occurred progressively. Albeit resolution of symptoms, the patient died 2 days after emergency department initial admission, following a cardiogenic pulmonary edema that did not respond to standard of care attitudes.
| Discussion | ▴Top |
It is well known that symptoms begin 5 to 30 minutes after strychnine intake, as it is readily absorbed by all routes. Clinical effects of ingestion have been seen at doses as small as 2 mg in a child and 20 mg in an adult [1]. The dose-dependent effects remain controverse. It is difficult to define a lethal dose as the published data are variable from one study to another, but it is possible to admit that it is situated between 30 - 100 mg [3]. By competing with glycine for glycinergic receptors (prevents the entrance of chloride, in the cell, that is responsible for a hyperpolarization and therefore stabilizing the membrane potential, diminishing the neuron excitability), strychnine inhibits post-synaptic inhibition, leading to increased motor neuron activity [3]. Classical manifestations may include a swift prodromal stage with anxiety, increased sense of awareness and hyperreflexia followed by a well documented clinical stage with nystagmus, risus sardonicus, trismus, intense generalized muscle contractions with preserved consciousness, tactile, auditory and visual stimuli hypersensitivity which may culminate in respiratory arrest and death within hours after ingestion due to contraction of the diaphragm, thoracic and abdominal muscles [5]. Sustained muscle contractions can lead to rhabdomyolysis, renal failure, hyperthermia and lactic acidosis. Vomiting, cardiac rhythm alterations, arterial hypertension and other analytical alterations like leukocytosis have also been described as symptoms of strychnine intoxication (Fig. 1). Other conditions such as tetanus, epileptic seizures, CNS infections, drug withdrawal syndromes, and amphetamine intoxication, may have similar manifestations. Nevertheless time course, clinical history and neurological examination are helpful for differentiating these conditions. Despite the delayed onset of overt clinical symptoms with generalized muscle contractions and startle response, an anxious patient with occasional myoclonus of the extremities was initially described, constituting a prolonged, not yet reported in literature, prodromal stage of strychnine intoxication. Confirmation can be attained by qualitative or quantitative strychnine analysis in body fluids or tissues, not available at our institution or in a timely fashion in other nearby facilities. Since the clinical index of suspicion was very elevated regarding the possibility of strychnine intoxication, further attempts in confirming its presence were not pursued. Treatment is supportive and includes benzodiazepines like diazepam (reports of use of 1 mg/kg [1]), lorazepam and clonazepam, GABA receptor-acting anticonvulsants (it may counteract the strychnine effect at the postsynaptic membrane by its inhibitory effect in the motor neuron [3]), mostly phenobarbital and sodium valproate (no specific dosages are described in literature), neuromuscular blocking agents, like atracurium or vecuronium, if previous muscle contractions controlling attempts were not successful, oxygen and airway support, as well as prevention of hemodynamic and metabolic complications (see above) [2, 3]. Gastric lavage and induced emesis must be carefully considered, given the risk of precipitating motor manifestations that can culminate in death it may be attempted after the control of muscle contractions. Despite successful treatment of involuntary movements with diazepam and sodium valproate, and adequate supportive treatment, the patient died after a cardiogenic pulmonary edema, probably due to excessive IV fluids administration allied with presumed, and previously not known, heart failure (elevated NT-Pro B-type Natriuretic Peptide) (Table 1) in a diabetic elderly. Confirmation of the cause of death was only possible if an autopsy had been performed, which was not requested by the family.
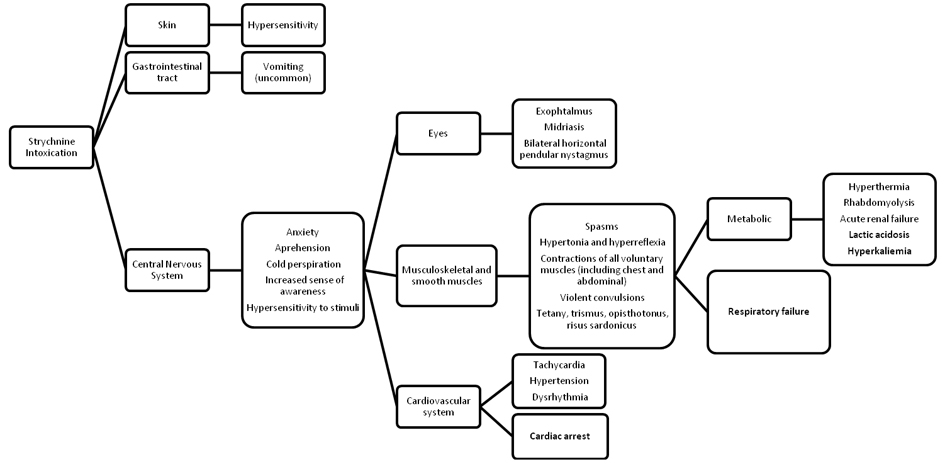 Click for large image | Figure 1. Clinical manifestations and complications of strychnine intoxication adapted from S Arzalier-Daret and D. du Cheyron [3]. |
Definite confirmation of strychnine intoxication requires its identification in blood, gastric fluid or urine samples, nowadays unavailable at the majority of institutions. The clinical picture described, even though with a delayed onset never reported to this date, strongly suggests this diagnosis. Since it is a substance no longer commercialized and thus not present in our every day routine, it calls for an extremely suspicious mind to timely rise this clinical hypothesis. When typical clinical manifestations are recognized early, appropriate treatment can result in a good outcome [2, 3].
Declaration
The authors have no financial disclosures and this work has not been supported by any institution or company. The authors report no conflict of interests.
| References | ▴Top |
- Wood D, Webster E, Martinez D, Dargan P, Jones A. Case report: Survival after deliberate strychnine self-poisoning, with toxicokinetic data. Crit Care. 2002;6(5):456-459.
doi pubmed - Parker AJ, Lee JB, Redman J, Jolliffe L. Strychnine poisoning: gone but not forgotten. Emerg Med J. 2011;28(1):84.
doi pubmed - Arzalier-Daret S, Cheyron D. Intoxication par la strychnine en 2011 :une menace toujourspresente!. Reanimation 2011;20:446-451.
doi - Smith BA. Strychnine poisoning. J Emerg Med. 1990;8(3):321-325.
doi - Makarovsky I, Markel G, Hoffman A, Schein O, Brosh-Nissimov T, Tashma Z, Dushnitsky T, et al. Strychnine—a killer from the past. Isr Med Assoc J. 2008;10(2):142-145.
pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


