| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 4, Number 6, June 2013, pages 365-368
Papillary Thyroid Cancer Arising From a Thyroglossal Duct Cyst
James R. Hoffmanna, Chien Chenb, c, Donald Bodennerc, d, Brendan C. Stack, Jrc, e, f
aUAMS College of Medicine, USA
bDepartment of Pathology, UAMS, USA
cUAMS Thyroid Center, USA
dDepartment of Geriatrics, UAMS, USA
eDepartment of-Otolaryngology-Head and Neck Surgery, USA
fCorresponding author: Brendan C. Stack, Department of Otolaryngology-Head and Neck Surgery, 4301 W. Markham Street Slot 543, Little Rock, AR 72205
Manuscript accepted for publication January 2, 2013
Short title: Papillary Thyroid Cancer Arising
doi: https://doi.org/10.4021/jmc1033w
| Abstract | ▴Top |
Interesting case presentation of papillary thyroid cancer is arising from a thyroglossal duct cyst. Retrospective case is review. We present a case of 36-year-old male who presented with nearly a two month history of a midline mass. Preoperative imaging revealed a midline mass approximately 2 cm in diameter, bilateral neck adenopathy, and a normal thyroid. The FNA of the midline mass was positive for papillary thyroid carcinoma. The patient underwent a total thyroidectomy, bilateral neck dissection, and a Sistrunk procedure. The patient was treated with post operative radio iodine. We report salient details of our case and also review relevant literature of this source of thyroid cancer. Thyroglossal duct cysts may be the origin of metastatic papillary thyroid cancer.
Keywords: Thyroglossal duct cyst; Papillary thyroid carcinoma; Fine needle aspiration cytology; Thyroid gland
| Introduction | ▴Top |
Thyroglossal duct cysts are the most prevalent form of congenital cysts that are present within the neck - reported as having a frequency of two times that of a branchial cleft cyst. While thyroglossal duct cysts are sometimes asymptomatic and frequently benign, some may present with symptoms and corresponding issues that may include potentially serious complications including infection or even, on rare occasions (approximately 1%) malignancy. Although the incidence of carcinoma within a thyroglossal duct cyst is quite rare, there have been numerous efforts to characterize and understand more regarding the etiology, histopathology, and treatment of this malignancy considering its variable development and presentation. As discussed in previous studies, carcinomas of a thyroglossal duct cyst have a frequent association (approximately 11-33%) with carcinomas in the thyroid gland (most frequently, papillary thyroid carcinoma) [1-7]. As a result of this association, efforts must be taken to determine whether these tumors are metastasis from a primary thyroid cancer or whether this is a primary papillary carcinoma within a thyroglossal duct cyst. We are presenting a case report that is suggestive of a papillary thyroid carcinoma originating from a thyroglossal duct cyst.
| Case Report | ▴Top |
Our patient is a 36-year-old male with a past medical history only notable for gout and kidney stones who initially presented with nearly a two month history of a midline mass that the patient originally noted upon self inspection. He denied dysphagia, odynophagia, hoarseness, tremor, palpitation, heat or cold intolerance, constipation, diarrhea and reported that his energy level was adequate. His history is otherwise negligible other than a 10 pack year smoking history (discontinued five years previously).
His physical exam revealed the presence of palpable lymphadenopathy in bilateral levels two and three with a midline mass at the level of the hyoid bone that measured approximately 2 cm in diameter. His exam was otherwise unremarkable with vital signs within normal range and BMI of 31.7.
He had a CT scan that showed the midline mass approximately 2 cm in diameter and bilateral neck adenopathy. An ultrasound was then performed which revealed a normal right and left lobe of the thyroid that were completely devoid of nodules. Furthermore, a cystic mass (2.5 × 1.2 × 2 cm) was noted near the region of the hyoid bone. These findings led to a fine needle aspiration (FNA) with ultrasound guidance. The FNA was positive for papillary thyroid carcinoma. Fine needle aspirations of the bilateral lymphadenopathy revealed papillary thyroid carcinoma as well (Fig. 1). This FNA illustrates the typical features of papillary thyroid carcinoma which include, nuclear enlargement, clearing, elongation, grooves and pseudo-inclusions. These features are best seen on Pap stain as utilized in this particular image.
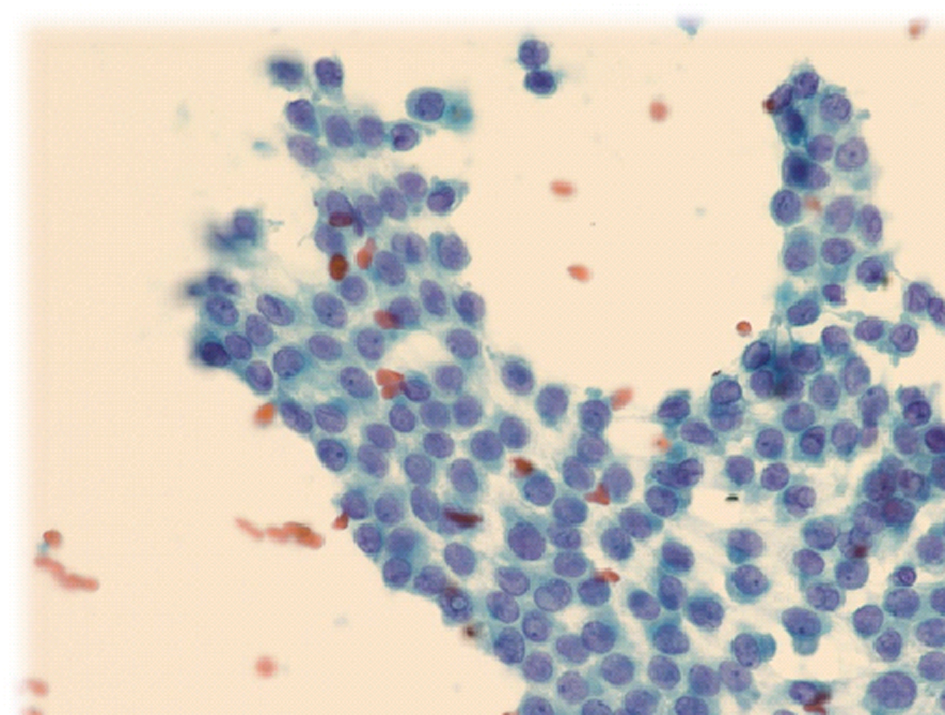 Click for large image | Figure 1. Papanicolaou stain of the aspirate from the thyroglossal duct. This was positive for papillary thyroid cancer. 400 ×. |
Due to the fact that the cystic lesion was noted to be in the region of the hyoid bone, this mass was suspected to be a thyroglossal duct cyst. The patient was then scheduled for the following procedure: total thyroidectomy, bilateral neck dissection, and a Sistrunk procedure.
Upon gross inspection of the thyroglossal mass, the patient was noted to have a tan-white, irregular lesion (1.5 × 1.2 × 0.6 cm) that was firm upon palpation. Intraoperatively, the patient was noted to have multiple cystic-appearing lymph nodes in levels 1 through 4 on the left. Some of the lymph nodes had a darkish hue to them. There was a large level 1 lymph node on the left which was adjacent to the presumed primary tumor, the thyroglossal duct cyst. The thyroid itself appeared unremarkable with a complete lack of masses.
Surgical pathology confirmed the presence of papillary thyroid carcinoma in the thyroglossal duct cyst (Fig. 2) and five of seventy-one lymph nodes (Fig. 3). The tumor was invasive with mild extension into the adjacent fibro adipose tissue.
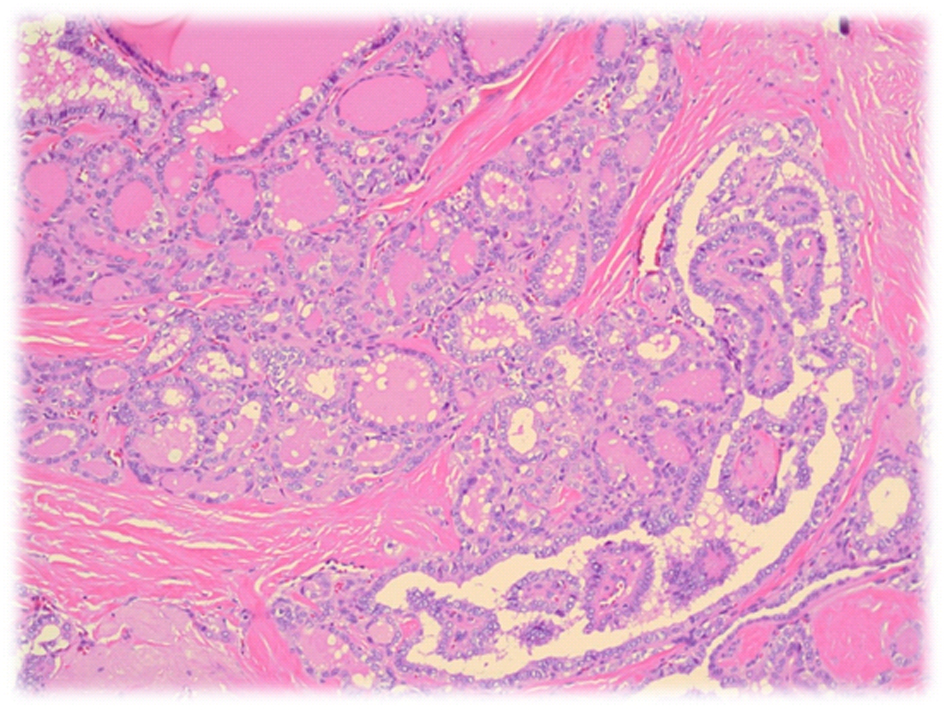 Click for large image | Figure 2. Permanent histology of the thyroglossal duct cyst demonstrating papillary thyroid cancer. Hematoxylin and eosin, 200 ×. |
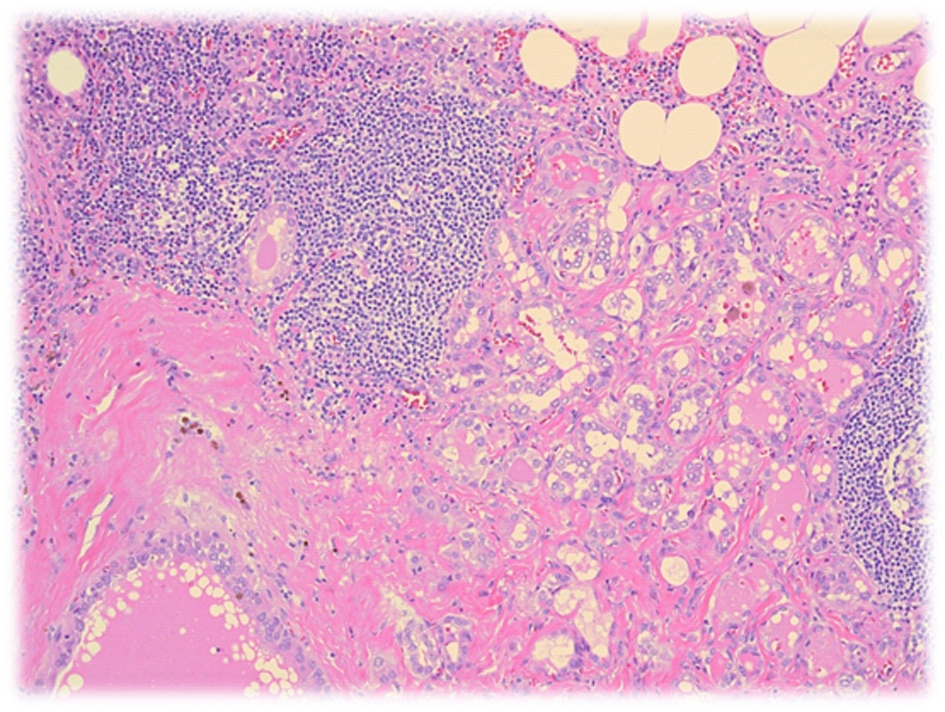 Click for large image | Figure 3. Permanent histology of the thyroglossal duct cyst demonstrating papillary thyroid cancer. Hematoxylin and eosin, 200 ×. |
This patient endured a rather long and complicated recovery in the hospital following this surgical procedure. He did well overnight initially with the two 15-French drains productive of serosanguinous output. On the second postoperative day, the patient was noted to have a milky output from the left neck drain - a chyle leak was suspected. The patient was started on a low fat diet and a pressure dressing was placed over the left neck. Following these measures, there was no notable improvement in the chyle leak. The patient was taken back to the operating room for a neck exploration. No definitive leak was found and a rotation flap of the sternothyroid muscle was utilized to sew over the thoracic duct - the sternocleidomastoid was also rotated in. The patient did well after the procedure and drain output dropped. However, two days following this procedure, the left neck drain began to have increased output which was again milky in appearance. The patient was scheduled for embolization by lymphangiogram. Unfortunately, this was unsuccessful, as no distal lymph vessels were able to be canalized. CT surgery was consulted for thoracic duct ligation. The patient underwent video-assisted thorascopic surgery which was converted to an open mini thoracotomy for ligation of the thoracic duct. A chest tube was placed following this procedure. During this period, the patient was also started on TPN for nutritional support. The neck drain was subsequently removed. His diet was slowly advanced to a low fat diet. Once the low fat diet was started and there was no evidence of chylous leak, the chest tube was removed and TPN was discontinued. Patient was discharged home following twenty days of hospitalization tolerating a low fat diet, ambulating without any problems, and with the chyle leak controlled.
| Discussion | ▴Top |
During the fourth week of gestation, a thyroglossal duct arises from the medial thyroid anlage (first and second pharyngeal pouches). This duct forms as a diverticulum that subsequently travels from the ventral portion of the foramen cecum and usually courses anterior to the body of the hyoid bone although it may be posterior or through the bone. It travels through the midline neck to the position of the normal thyroid in the base of the neck by the 7th week. This tract usually atrophies and disintegrates by the 10th week of gestation. Although it is uncertain as to the potential etiology for the formation of a thyroglossal duct cyst, a post-mortem study involving 200 adults found the incidence to be approximately 7% [1].
In the pediatric population, the thyroglossal duct cyst represents the most common cause of a midline neck mass. Due to numerous reasons in patients of all ages presenting with a thyroglossal duct cyst - cosmetic, patient discomfort and inflammation/infection - the typical recommendation is to excise the clinically apparent cyst by means of the Sistrunk procedure [7]. This procedure consists of a removal of the thyroglossal duct cyst, the central portion of the hyoid bone, and the thyroglossal duct all in continuity. The recurrence rate is less than 4% following this procedure [3].
Further procedures, such as neck dissection and total thyroidectomy, are typically only warranted for more extensive malignancies. Although a carcinoma within the thyroglossal duct cyst is rare (0.7-1%), it is important to be aware of this possibility in terms of how it may affect treatment. The necessity for expanding the surgery to include bilateral neck dissection and a total thyroidectomy is typically performed if there is evidence of lymph node, direct extension of the malignancy and/or intrathyroidal metastatic lesions (the latter two of which are indications for thyroidectomy and neck dissection). However, even in the presence of malignancy, the Sistrunk procedure will suffice for non-metastatic disease and for medically high risk patients [5]. Fortunately, following this procedure when papillary thyroglossal duct cyst carcinoma is present, the overall survival rate is at approximately 95.6% over a period of 10 years postoperatively [4].
Due to the accessibility of these midline masses, fine needle aspiration cytology, FNAC, is a rapid, safe, well-tolerated and relatively inexpensive procedure for initial evaluation. However, as discussed in a review of literature by Yang et al, a preoperative FNAC has shown to have poor true- and false-negative rates, at 53% and 47%, respectively [4, 5]. In contrast, according to Miccoli et al, patients that underwent a repeat FNAC resulted in 100% sensitivity and specificity in a group of nine patients subjected to this procedure, especially when performed under ultrasound guidance. Furthermore, other diagnostic techniques are typically unable to make a preoperative diagnosis (CT, ultrasound, scintigraphy) [4, 6]. Thus, based on these previous studies, workups of these midline masses benefit from an ultrasound-guided FNAC.
Despite the rare incidence of papillary carcinoma in a thyroglossal duct cyst, many efforts have been undertaken to further characterize proper workup, symptoms, and subsequent treatment and, as discussed above, significant improvements have been made. However, one important topic to address is the importance of recognizing whether this malignancy is within the thyroglossal duct cyst is primary or secondary to a metastatic tumor primary from the thyroid proper. This is important not only in terms of surgical treatment, but also in terms of prognosis [7].
The incidence of thyroid gland involvement in association with thyroglossal duct cyst papillary carcinoma has been shown to range from 11-33% [1, 3]. Typically, a metastatic tumor from the thyroid to thyroglossal duct cyst would indicate the necessity to perform a total thyroidectomy in addition to the Sistrunk procedure for treating primary papillary carcinoma of the thyroglossal duct cyst (in the absence of evidence of other malignancy - thyroid, lymph nodes, etc.). Furthermore, thyroglossal duct cyst papillary carcinoma has a much lower metastatic rate in comparison to a papillary carcinoma arising from the thyroid proper (7% and 87%, respectively) [7].
These two variable forms of presentation of this malignancy seem to have a different appearance pathologically. In fact, the diagnosis of a primary thyroglossal duct cyst papillary carcinoma requires the identification of malignant cells interspersed with normal ectopic thyroid in addition to the recognition of the duct wall or its remnant. The duct wall is usually lined by columnar cells. The combination of these features allows an additional means of differentiation of a metastatic papillary carcinoma arising from thyroid proper from the primary form of thyroglossal duct cyst papillary carcinoma.
Despite the relatively frequent association of primary thyroid involvement in addition to a thyroglossal duct cyst carcinoma, our case likely represents the primary papillary thyroid carcinoma arising from the thyroglossal duct rather than a metastasis due to a number of reasons: the location of the lesion was high in the central neck (typical of a thyroglossal duct remnant), the lack of residual lymph node, the unencapsulated, stellate and irregular nature of the lesion (not consistent with a lymph node metastasis) and, most importantly, the lack of a primary lesion in the entirely submitted thyroid.
Conclusion
By utilizing ultrasound-guided FNAC, we were able to obtain a diagnosis of papillary carcinoma of the thyroglossal duct cyst. This enabled an understanding of how to approach this patient in terms of treatment. Ultrasound-guided biopsy should be employed in order to characterize this neck mass prior to any form of treatment.
Furthermore, histopathology may allow a determination of whether this malignancy in the thyroglossal duct cyst is primary or due to a secondary metastasis from a thyroid malignancy - information which is useful in recognizing prognosis as well as for formulating treatment.
Summary
1). Papillary thyroid cancer can arise from a thyroglossal duct cyst. 2). Conventional ultrasound and fine needle aspiration techniques should be used when evaluating all neck masses, including those of thyroid or thyroglossal duct origins. 3). Society guidelines (namely, American Thyroid Association) can provide guidance in the proper diagnosis and management of well-differentiated thyroid cancers.
| References | ▴Top |
- Randolph GW and Kamani DV. "Thyroglossal duct cysts and ectopic thyroid." UpToDate. http://www.uptodate.com/contents/thyroglossal-duct-cysts-and-ectopic-thyroid?source=search_result&selectedTitle=1%7E18#>.
- Weiss SD, Orlich CC. Primary papillary carcinoma of a thyroglossal duct cyst: report of a case and literature review. Br J Surg. 1991;78(1):87-89.
doi - Heshmati HM, Fatourechi V, van Heerden JA, Hay ID, Goellner JR. Thyroglossal duct carcinoma: report of 12 cases. Mayo Clin Proc. 1997;72(4):315-319.
doi pubmed - Albarak Y, Albarak F, Kaya Z, Esref K, Aylu B. A Case of Papillary Carcinoma in a Thyroglossal Cyst Without a Carcinoma in the Thyroid Gland. Wiley Online Library 2010; Vol 39, No 1.
- Patel SG, Escrig M, Shaha AR, Singh B, Shah JP. Management of well-differentiated thyroid carcinoma presenting within a thyroglossal duct cyst.J SurgOncol. 2002;79(3):134-139; discussion 140-131.
- Miccoli P, Minuto MN, Galleri D, Puccini M, Berti P. Extent of surgery in thyroglossal duct carcinoma: reflections on a series of eighteen cases. Thyroid. 2004;14(2):121-123.
doi pubmed - Falconieri G, Della Libera D, Zanella M. Papillary thyroid carcinoma of the thyroglossal duct cyst: comparative cytohistologic and immunochemical study of 2 new cases and review of the literature. Int J SurgPathol. 2001;9(1):65-71.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


