| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 13, Number 8, August 2022, pages 414-420
Reverse Takotsubo Cardiomyopathy in a Patient With Commotio Cordis
Yasir Ahmeda, e, Muhammad Rafiqueb, Sajjad Ahmadc, Bassam Omard, Christopher Malozzid
aDepartment of Internal Medicine, United Health Services Hospitals, Binghamton, NY, USA
bSt. Bernards Health Care System, Heart and Vascular, Jonesboro, AZ, USA
cMosaic Lifecare at St. Joseph Cardiovascular Care, Saint Joseph, MO, USA
dDepartment of Cardiology, University of South Alabama Health University Hospital, Mobile, AL, USA
eCorresponding Author: Yasir Ahmed, Department of Internal Medicine, United Health Services Hospitals, Binghamton, NY, USA
Manuscript submitted May 15, 2022, accepted August 10, 2022, published online August 19, 2022
Short title: Reverse TCM in a Patient With CC
doi: https://doi.org/10.14740/jmc3951
| Abstract | ▴Top |
Takotsubo cardiomyopathy (TCM), also known as stress cardiomyopathy or “broken heart syndrome”, is characterized by acute transient regional left ventricular systolic dysfunction in the absence of obstructive coronary artery disease or acute plaque rupture. Atypical forms and rare anatomical variants can have different presentations; hence, recognition becomes more important. Prognosis is much more favorable if managed appropriately. An equally infrequent cause of cardiac arrest is commotio cordis (CC). This is defined as sudden cardiac death secondary to a blunt chest wall impact leading to ventricular arrhythmias. We report a case with findings of TCM and/or CC in a patient with a blunt chest trauma in the setting of motor vehicle accident.
Keywords: Cardiomyopathy; Takotsubo; Stress cardiomyopathy; Reverse takotsubo; Commotio cordis
| Introduction | ▴Top |
Cardiac arrest can take many forms. In the case of traumatic injuries, such as motor vehicle crashes, cardiac trauma is usually defined as blunt or penetrating. Often not considered is the emotional stress inflicted by such an accident. This type of “trauma” can lead to another form of cardiac injury. Takotsubo cardiomyopathy (TCM), otherwise known as stress cardiomyopathy, was first described in 1990 by Sato and colleagues as a reversible cardiomyopathy, demonstrating a very interesting motion of the left ventricle (LV) [1]. Takotsubo is a Japanese word which mean “octopus trap”. This term is aptly assigned in this condition as the shape of the LV at the end of systole resembled the octopus pots of Japanese fisherman. TCM is an acute phenomenon that is reversible and related to profound stress [1]. Commotio cordis (CC) is defined as sudden cardiac death secondary to blunt chest wall impact. The impact leads to ventricular tachycardia (VT) or ventricular fibrillation (VF). It is one of the common causes of sudden cardiac death, especially in young athletes after hypertrophic cardiomyopathy and congenital coronary artery anomalies [2]. This article discusses two less frequently encountered causes of cardiac injury, TCM and CC.
| Case Report | ▴Top |
Investigations
A 52-year-old man with diabetes mellitus type II, gastric bypass surgery and depression was involved in a motor vehicle accident and was transferred from an outside hospital (OSH) for trauma team services. The accident was witnessed, and the patient reportedly swerved off the road and hit a tree head on. Upon impact, he recalls hitting his chest against the steering wheel. Airbags were reportedly deployed as well. He was seen trying to make an exit out of the car and trying to initiate a phone call to 911. He reportedly collapsed and bystanders began cardiopulmonary resuscitation (CPR). Upon arrival of the paramedics, he was found to be in asystole and acute cardiac life support (ACLS) was immediately initiated. He did not require defibrillation during resuscitation. At the OSH, he reportedly developed pulseless electrical activity, requiring continued ACLS treatment. He was successfully resuscitated and intubated prior to arrival. He was also receiving volume resuscitation with intravenous fluids and packed red blood cells. Upon arrival, his systolic blood pressure was 60 mm Hg and heart rate was 164 bpm. He was admitted to surgical intensive care unit (SICU). Radiographic imaging studies excluded significant injuries that would require surgical intervention.
Diagnosis
The patient’s initial electrocardiogram (ECG) showed sinus tachycardia without significant ST-segment changes (Fig. 1). Initial troponin was 3.15 ng/mL that peaked to 10.9 ng/mL. His total creatine kinase (CK) was 768 U/L and CK-MB portion was 7.6 ng/mL. Urine drug screen was negative for illicit substances. Transthoracic echocardiogram (TTE) showed a left ventricular ejection fraction (LVEF) of 35-40%. There was preservation of apical wall motion with hypokinesis to akinesis of the basal and mid-left ventricular (MLV) wall segments. This pattern suggested reverse TCM (Fig. 2). However, due to the significant rise in troponin, treatment for acute coronary syndrome (ACS) was initiated. The patient received aspirin, ticagrelor, and was placed on a heparin infusion. He underwent left heart catheterization and coronary angiography revealed mild nonobstructive coronary artery disease (CAD) (Fig. 3a, b). A diagnosis of reverse TCM was made. Consideration was also given to CC as a possible contributor to this patient’s cardiac arrest. Computed tomography (CT) of the chest revealed a retrosternal isodensity consistent with retrosternal hematoma and bilateral pulmonary contusions consistent with chest trauma. Ticagrelor and heparin were subsequently discontinued, and he was maintained on aspirin and statin therapy. The patient improved over the course of next 2 days and he was moved out of ICU level care. Meanwhile his medical records were obtained. He had workup done for premature ventricular contractions (PVCs), including a TTE performed 2 months prior to this hospitalization which showed an EF of 60-65% and no wall motion abnormalities. A 24-h Holter monitor and then a 30-day event recorder did not reveal any serious arrhythmias that could be implicated for his cardiac arrest.
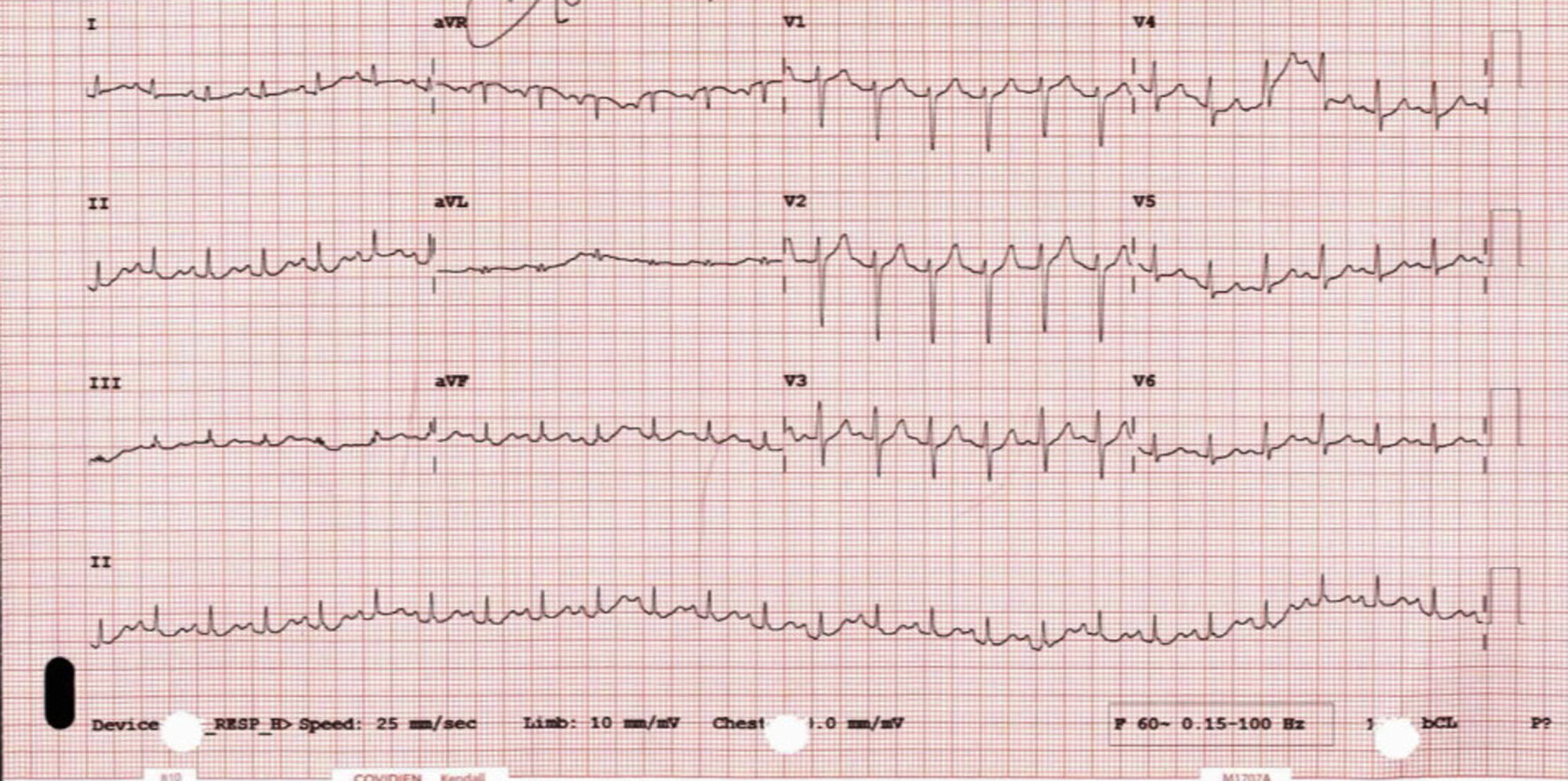 Click for large image | Figure 1. ECG: sinus tachycardia, no significant ST-segment changes. ECG: electrocardiogram. |
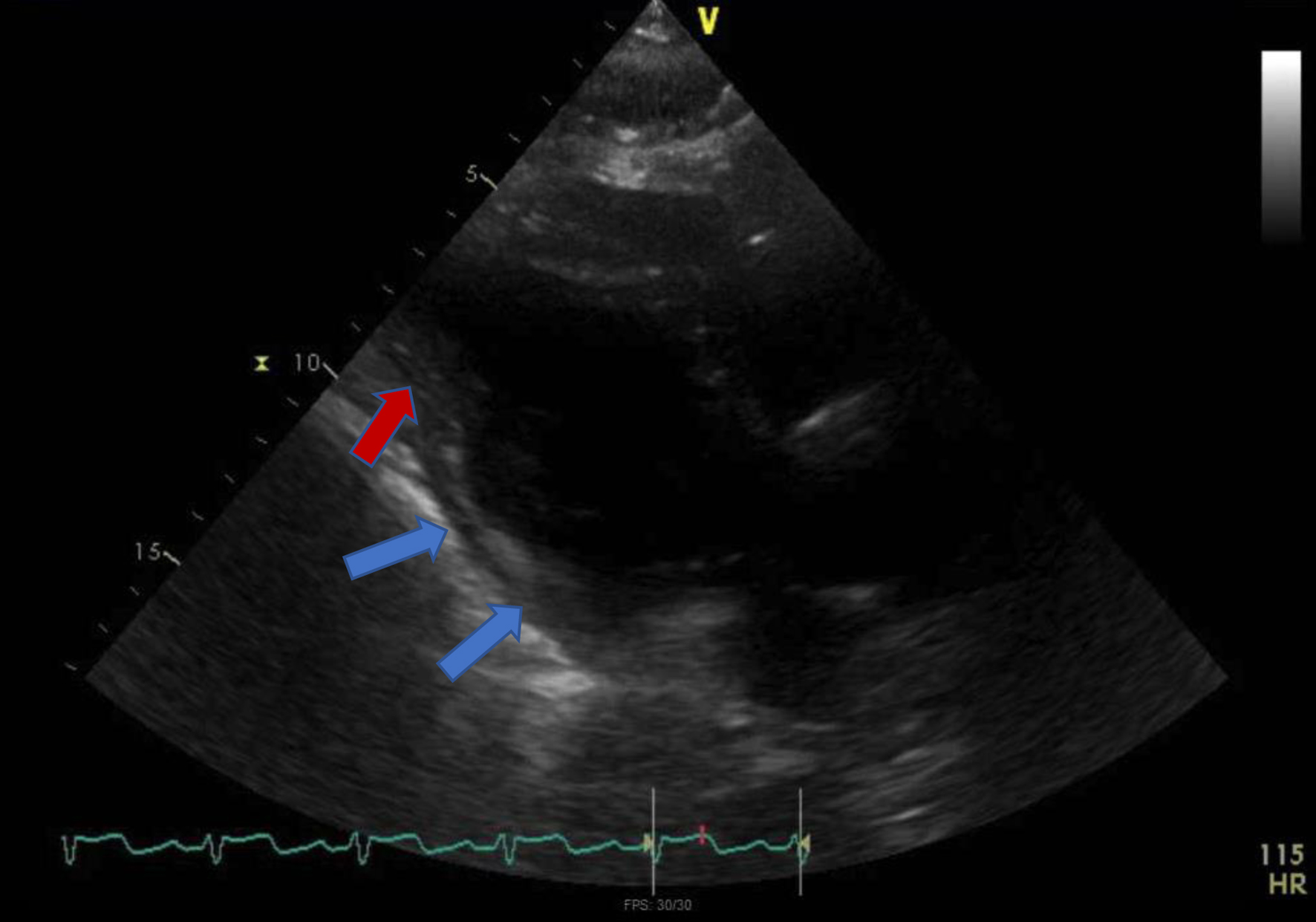 Click for large image | Figure 2. TTE: parasternal long axis view showing “ballooning” of basal and mid segments (blue arrows) while preserved contractility in the apex (red arrow). TTE: transthoracic echocardiogram. |
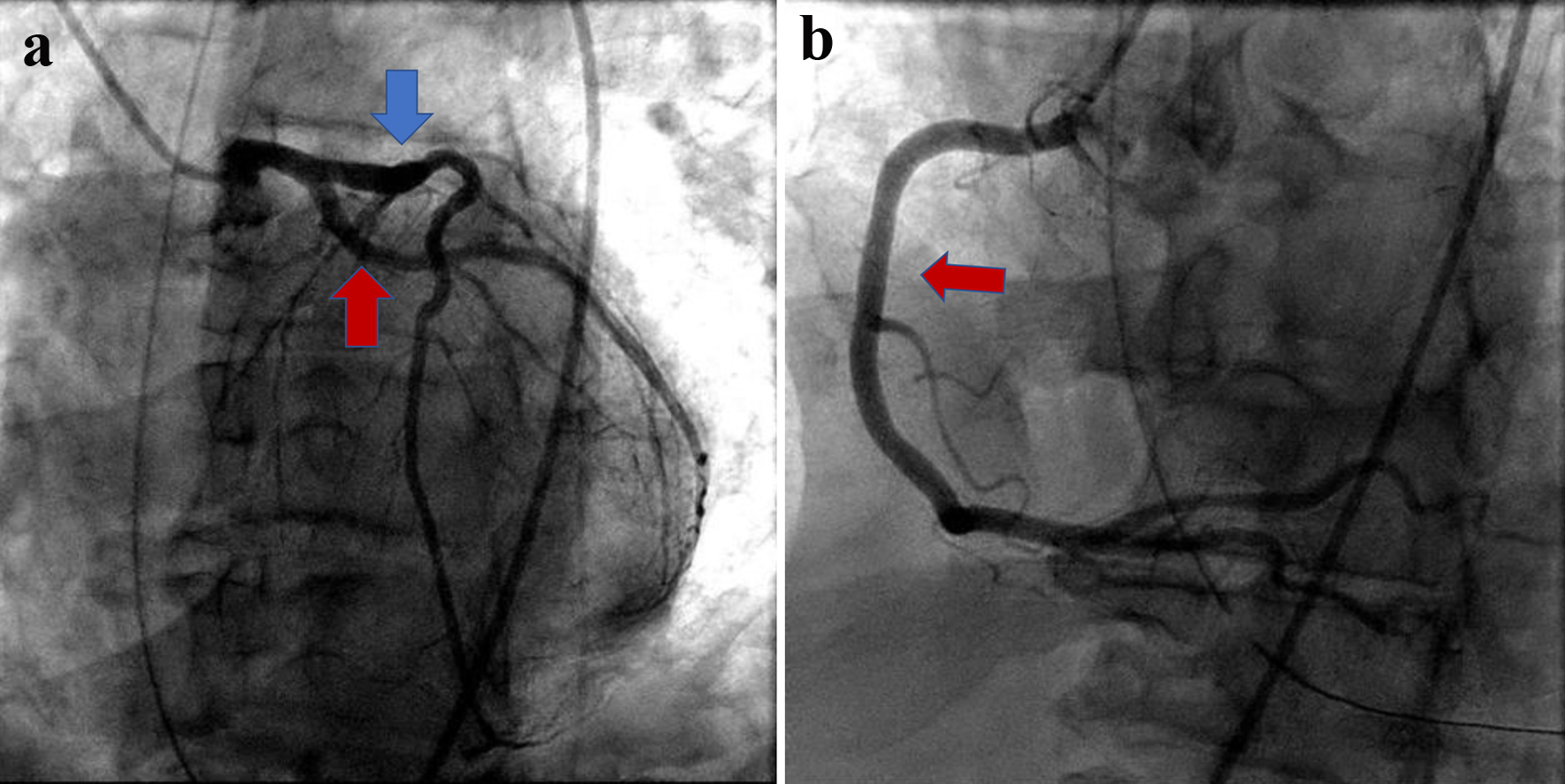 Click for large image | Figure 3. (a) Coronary angiogram with no significant obstructive disease in left anterior descending artery (blue arrow) and circumflex artery (red arrow). (b) Coronary angiogram showing patent right coronary artery (red arrow). |
A repeat TTE was obtained on hospital day 5 that showed a recovered EF of 55-60% and no wall motion abnormalities (Fig. 4). The patient was discharged from the hospital after vast clinical improvement with an early follow-up in cardiology clinic and with an electrophysiologist (EP).
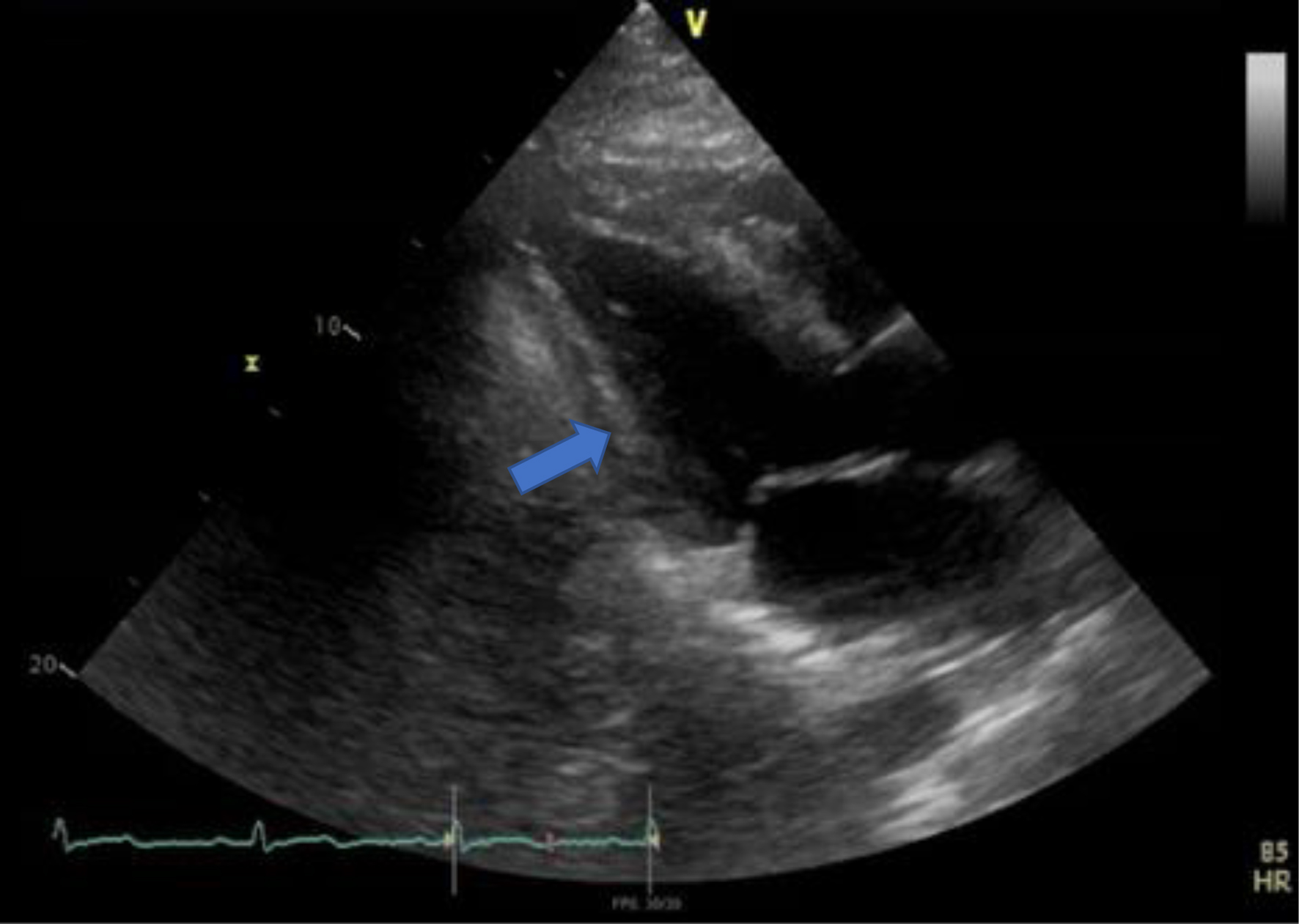 Click for large image | Figure 4. Repeat TTE parasternal long axis view with no more basal and mid segments ballooning (blue arrow). TTE: transthoracic echocardiogram. |
Treatment
At the time of discharge, he was fitted with a wearable defibrillator vest. Cardiac magnetic resonance (CMR) imaging was done that ruled out arrhythmogenic right ventricular cardiomyopathy. He underwent automated implantable cardioverter defibrillator (AICD) placement as an outpatient for secondary prevention of cardiac arrest.
Follow-up and outcomes
The patient continued to follow-up in cardiology clinic. Presently, he is asymptomatic and has not had any acute events since his accident.
| Discussion | ▴Top |
There is systolic apical ballooning of the LV in the typical form of TCM, reflecting hypokinesis/akinesis of mid and apical segments, and there is often hyperkinesis of the basal walls that occurs in up to 80% of patients. Atypical forms such as MLV variant and inverted or basal variant have also been described. In MLV variant, ballooning and hypokinesia is seen in MLV area and hyperkinesia in apical and basal segments and it occurs in about 15% of cases. In the inverted or basal variant, circumferential basal hypokinesia and apical hypercontractility is seen and it occurs in about 5% [3, 4]; hence, TCM should not be considered exclusively as apical ballooning syndrome (Table 1). Reverse TCM is an atypical variant, characterized by basal hypokinesis/akinesis and apical sparing or hyperkinesis and sometimes referred to as “inverted takotsubo”, “nutmeg” or “artichoke heart” [4].
 Click to view | Table 1. Anatomical Variants of Takotsubo Syndrome and Their Prevalence, According to the Heart Failure Association of the European Society of Cardiology [2] |
Stress cardiomyopathy is more common in women than men and occurs predominantly in older adults [5]. In the International Takotsubo Registry of 1,750 patients with stress cardiomyopathy, 89.9% were women with mean age of 66.4 years [6]. The prevalence of TCM is approximately 1-2% in patients presenting with troponin-positive suspected ACS or suspected ST-elevation myocardial infarction [7, 8]. Reverse TCM was found in 2.2% of the patients in International Takotsubo Registry [3].
The pathogenesis of stress cardiomyopathy is complex and there are multiple postulated mechanisms which include catecholamine excess [9, 10], microvascular dysfunction and coronary artery spasm. Association of stress cardiomyopathy with physical or emotional stress [6] suggests that it may be caused by diffuse catecholamine-induced microvascular spasm or dysfunction, resulting in myocardial stunning [11], or by direct catecholamine-associated myocardial toxicity [12]. Since most of the patients with TCM are postmenopausal women, estrogen deficiency has also been suggested as a possible underlying mechanism [13]. Previous studies have shown that TCM is predominantly preceded by emotional triggers [9]. More recent studies have shown that the disease may also occur with physical triggers or even without any evident preceding trigger [14]. More than half of all patients with TCM had an acute, former, or chronic neurologic or psychiatric disorder; however, the absence of a trigger does not preclude a diagnosis of this disorder [6]. Patients with atypical TCM were found to be young, have experienced neurologic abnormalities more often, but interestingly the presence of emotional or physical trigger was comparable to typical TCM contrary to the common belief [3].
Reverse TCM presents like typical TCM and mimics ACS symptoms including chest pain, dyspnea, nausea, diaphoresis, abdominal pain, or syncope [15]. ECG changes can vary from T-wave changes, ST-segment deviation, bundle branch block or QT prolongation. ST-segment depression was more frequent in atypical TCM, and ST-segment elevation and T-wave inversion were less frequent compared to typical TCM which was attributed to difference in wall motion patterns [3]. More than 80% of the patients have elevated troponin at the time of presentation along with ECG changes in TCM [6]. Mayo Clinic diagnostic criteria are mostly used for diagnosing this condition [16]. Typical diagnostic workup includes ECG, cardiac enzymes, TTE, and coronary angiogram, but the ultimate diagnosis is made by cardiac catheterization and left ventriculography. Although the presence of CAD does not exclude the diagnosis of TCM, 15.3% of patients were noted to have co-existing CAD [17, 18].
In low-risk cases of takotsubo syndrome, if LVEF is > 45%, they can be discharged from the hospital. In patients with LVEF of 35-45%, heart failure medications including beta-blocker (metoprolol or carvedilol) are recommended unless beta-blockers are contraindicated [4, 10, 19]. Monitoring with continuous ECG in coronary care unit is recommended when life-threatening complications are anticipated [20]. The rate of in-hospital complications is comparable between TCM and ACS [6]. Potential complications include cardiogenic shock, cardiac arrest, ventricular arrhythmias, and LV thrombus [4]. Approximately 10% of patients with stress cardiomyopathy may present with cardiogenic shock which should be managed supportively. In patients with left ventricular outflow tract (LVOT) obstruction, inotropes should be used cautiously as they can increase LVOT pressure gradient which in turn worsens the shock and leads to overall worse outcomes [21]. Left ventricular thrombus was identified in 1.3% of patients in International Takotsubo Registry study. It should be treated with anticoagulation [6].
Patients who survive the acute episode typically recover systolic ventricular function completely. Stress cardiomyopathy can reoccur in 5-22% of patients, 3 months to 10 years after the first episode [4].
The word “CC” is derived from Latin which mean “agitation of the heart”, and is defined as sudden cardiac death secondary to blunt chest wall impact, thus its relationship to sudden cardiac death in sports. It has been identified as one of the common causes of sudden cardiac death especially in young athletes [2]. Since its establishment in the mid-1990s, National Commotio Cordis Registry has published over 200 confirmed cases of CC [2, 22]. The increase in number is attributed to more awareness, hence more reporting rather than increase in the actual incidence of the disease. The diagnosis of CC is mostly based upon the clinical scenario (i.e., blunt chest trauma followed by collapse), available electrocardiographic data demonstrating VF, and the absence of structural heart disease or myocardial trauma on imaging studies [2].
Sudden death due to CC is primarily an electrical event, with VF occurring shortly after chest wall impact [22, 23]. The two most important variables in the development of VF in cases of CC are a blow directly over the precordium and the timing of chest wall impact within the cardiac cycle [22, 24]. Chest impact occurring during a 10 - 20 ms window on the upslope of the T-wave before it reaches its peak has been described as the period when the myocardium is repolarizing and is most susceptible to ventricular arrhythmia development [2, 24]. The most common rhythm noticed is VF followed by VT. Although asystole is seen more than VF or VT on first ECG reading, it is not thought to be the initial rhythm [25]. Hence, the recognition of CC is important as restoration of VF/VT, if present, to sinus rhythm with defibrillation can potentially improve survival. This statement is supported by recent data showing improved survival of 58% in reported cases between 2006 and 2012 compared to 34% during 1993 and 2012 [26], which is related to earlier recognition and activation of emergency medical services. The institution of CPR and availability of defibrillator within 3 min of the event increases the likelihood of survival [24]. The success rate with defibrillation with an automated external defibrillator (AED) within 1 and 2 min of ventricular resuscitation was 100% and 92% in animal studies [27]. There was a marked drop to 25% success rate after 6 min. There is more widespread availability of AED and trained personnel who can initiate CPR and use AED at professional as well as youth sports events in recent times due to increased awareness.
Conclusion
CC and TCM are both less frequent causes of cardiac injury and in our case, CC might have caused it or at least contributed towards reverse TCM. Despite grave presentation, timely institution of resuscitative process proved lifesaving and patient was able to make a full recovery, which is thought to be the key to improved survival. We intend to add valuable information to literature by sharing our experience.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Informed consent was obtained.
Author Contributions
Yasir Ahmed drafted initial document for publication, collected EKGs and images, coordinated with authors and supervisor, and finalized the report for submission. Mohammad Rafique contributed to critical analysis of the case and finalizing draft for publication and contributed to discussion. Sajjad Ahmad contributed to discussion and analysis of imaging and proofreading the article/draft before submission for any mistakes and omissions. Bassam Omar contributed to proofreading and review of the article and selecting images for the article.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Sato M, Fujita S, Saito A, Ikeda Y, Kitazawa H, Takahashi M, Ishiguro J, et al. Increased incidence of transient left ventricular apical ballooning (so-called 'Takotsubo' cardiomyopathy) after the mid-Niigata Prefecture earthquake. Circ J. 2006;70(8):947-953.
doi pubmed - Maron BJ, Estes NA, 3rd. Commotio cordis. N Engl J Med. 2010;362(10):917-927.
doi pubmed - Ghadri JR, Cammann VL, Napp LC, Jurisic S, Diekmann J, Bataiosu DR, Seifert B, et al. Differences in the clinical profile and outcomes of typical and atypical takotsubo syndrome: data from the international takotsubo registry. JAMA Cardiol. 2016;1(3):335-340.
doi pubmed - Lyon AR, Bossone E, Schneider B, Sechtem U, Citro R, Underwood SR, Sheppard MN, et al. Current state of knowledge on Takotsubo syndrome: a position statement from the taskforce on takotsubo syndrome of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2016;18(1):8-27.
doi pubmed - Sharkey SW, Lesser JR, Zenovich AG, Maron MS, Lindberg J, Longe TF, Maron BJ. Acute and reversible cardiomyopathy provoked by stress in women from the United States. Circulation. 2005;111(4):472-479.
doi pubmed - Templin C, Ghadri JR, Diekmann J, Napp LC, Bataiosu DR, Jaguszewski M, Cammann VL, et al. Clinical Features and Outcomes of Takotsubo (Stress) Cardiomyopathy. N Engl J Med. 2015;373(10):929-938.
doi pubmed - Kurowski V, Kaiser A, von Hof K, Killermann DP, Mayer B, Hartmann F, Schunkert H, et al. Apical and midventricular transient left ventricular dysfunction syndrome (tako-tsubo cardiomyopathy): frequency, mechanisms, and prognosis. Chest. 2007;132(3):809-816.
doi pubmed - Prasad A, Dangas G, Srinivasan M, Yu J, Gersh BJ, Mehran R, Stone GW. Incidence and angiographic characteristics of patients with apical ballooning syndrome (takotsubo/stress cardiomyopathy) in the HORIZONS-AMI trial: an analysis from a multicenter, international study of ST-elevation myocardial infarction. Catheter Cardiovasc Interv. 2014;83(3):343-348.
doi pubmed - Wittstein IS, Thiemann DR, Lima JA, Baughman KL, Schulman SP, Gerstenblith G, Wu KC, et al. Neurohumoral features of myocardial stunning due to sudden emotional stress. N Engl J Med. 2005;352(6):539-548.
doi pubmed - Paur H, Wright PT, Sikkel MB, Tranter MH, Mansfield C, O'Gara P, Stuckey DJ, et al. High levels of circulating epinephrine trigger apical cardiodepression in a beta2-adrenergic receptor/Gi-dependent manner: a new model of Takotsubo cardiomyopathy. Circulation. 2012;126(6):697-706.
doi pubmed - Gianni M, Dentali F, Grandi AM, Sumner G, Hiralal R, Lonn E. Apical ballooning syndrome or takotsubo cardiomyopathy: a systematic review. Eur Heart J. 2006;27(13):1523-1529.
doi pubmed - Nef HM, Mollmann H, Kostin S, Troidl C, Voss S, Weber M, Dill T, et al. Tako-Tsubo cardiomyopathy: intraindividual structural analysis in the acute phase and after functional recovery. Eur Heart J. 2007;28(20):2456-2464.
doi pubmed - Milinis K, Fisher M. Takotsubo cardiomyopathy: pathophysiology and treatment. Postgrad Med J. 2012;88(1043):530-538.
doi pubmed - Sharkey SW, Windenburg DC, Lesser JR, Maron MS, Hauser RG, Lesser JN, Haas TS, et al. Natural history and expansive clinical profile of stress (tako-tsubo) cardiomyopathy. J Am Coll Cardiol. 2010;55(4):333-341.
doi pubmed - Amsterdam EA, Wenger NK, Brindis RG, Casey DE, Jr., Ganiats TG, Holmes DR, Jr., Jaffe AS, et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;130(25):e344-426.
doi - Scantlebury DC, Prasad A. Diagnosis of Takotsubo cardiomyopathy. Circ J. 2014;78(9):2129-2139.
doi pubmed - Prasad A, Lerman A, Rihal CS. Apical ballooning syndrome (Tako-Tsubo or stress cardiomyopathy): a mimic of acute myocardial infarction. Am Heart J. 2008;155(3):408-417.
doi pubmed - Parodi G, Citro R, Bellandi B, Del Pace S, Rigo F, Marrani M, Provenza G, et al. Tako-tsubo cardiomyopathy and coronary artery disease: a possible association. Coron Artery Dis. 2013;24(6):527-533.
doi pubmed - Izumi Y, Okatani H, Shiota M, Nakao T, Ise R, Kito G, Miura K, et al. Effects of metoprolol on epinephrine-induced takotsubo-like left ventricular dysfunction in non-human primates. Hypertens Res. 2009;32(5):339-346.
doi pubmed - Schneider B, Athanasiadis A, Schwab J, Pistner W, Gottwald U, Schoeller R, Toepel W, et al. Complications in the clinical course of tako-tsubo cardiomyopathy. Int J Cardiol. 2014;176(1):199-205.
doi pubmed - Fefer P, Chelvanathan A, Dick AJ, Teitelbaum EJ, Strauss BH, Cohen EA. Takotsubo cardiomyopathy and left ventricular outflow tract obstruction. J Interv Cardiol. 2009;22(5):444-452.
doi pubmed - Link MS. Commotio cordis: ventricular fibrillation triggered by chest impact-induced abnormalities in repolarization. Circ Arrhythm Electrophysiol. 2012;5(2):425-432.
doi pubmed - Link MS, Wang PJ, Pandian NG, Bharati S, Udelson JE, Lee MY, Vecchiotti MA, et al. An experimental model of sudden death due to low-energy chest-wall impact (commotio cordis). N Engl J Med. 1998;338(25):1805-1811.
doi pubmed - Madias C, Maron BJ, Weinstock J, Estes NA, 3rd, Link MS. Commotio cordis—sudden cardiac death with chest wall impact. J Cardiovasc Electrophysiol. 2007;18(1):115-122.
doi pubmed - Maron BJ, Gohman TE, Kyle SB, Estes NA, 3rd, Link MS. Clinical profile and spectrum of commotio cordis. JAMA. 2002;287(9):1142-1146.
doi pubmed - Maron BJ, Haas TS, Ahluwalia A, Garberich RF, Estes NA, 3rd, Link MS. Increasing survival rate from commotio cordis. Heart Rhythm. 2013;10(2):219-223.
doi pubmed - Link MS, Maron BJ, Stickney RE, Vanderbrink BA, Zhu W, Pandian NG, Wang PJ, et al. Automated external defibrillator arrhythmia detection in a model of cardiac arrest due to commotio cordis. J Cardiovasc Electrophysiol. 2003;14(1):83-87.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


