| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 3, Number 5, October 2012, pages 304-307
A Case of Brucellosis With Simultaneous Dactylitis and Sacroiliitis
Ibrahim Batmaza, c, Recep Tekinb, Mustafa Akif Sariyildiza, Ozcan Devecib, Remzi Cevika
aDicle University Faculty of Medicine, Department of Physical Medicine and Rehabilitation, Diyarbakir, Turkey
bDicle University School of Medicine, Department of Clinical Microbiology and Infectious Disease, Diyarbakir, Turkey
cCorresponding author: Ibrahim Batmaz
Manuscript accepted for publication May 10, 2012
Short title: Brucellosis With Simultaneous Dactylitis and Sacroiliitis
doi: https://doi.org/10.4021/jmc701w
| Abstract | ▴Top |
Brucellosis is a zoonosis of worldwide distribution caused by small gram-negative nonencapsulated coccobacilli of the genus Brucella. Musculoskeletal involvement is one of the most common locations and includes spondylitis, sacroiliitis, osteomyelitis, peripheral arthritis, bursitis, and tenosynovitis. The most common osteoarticular finding in adult is sacroiliitis. However, dactylitis is seemed very rare in osteoarticular involvement with brucellosis. We report a very rare case of brucellosis with simultaneous dactylitis and sacroiliitis.
Keywords: Brucellosis; Dactylitis; Osteoarticular involvement; Sacroiliitis
| Introduction | ▴Top |
Brucellosis is a type of zoonosis caused by the Brucella type of bacteria and transmitted to humans by the meat, bodily fluids like milk and urine or the fetal material from infected animals like sheep, goat, cattle and pigs. Another way of transmission is the ingestion of the dairy products prepared with the milk from infected animals. Brucellosis manifests itself with high fever, shivering and pain in the muscles and large joints [1].
Osteoarticular involvement is the most frequently observed complication of brucellosis [2]. Osteoarticular involvement includes spondylitis, sacroiliitis, osteomyelitis, peripheral arthritis, bursitis, and tenosynovitis [3]. In this article, a case of brucellosis with a combination of sacroiliitis and dactylitis is presented.
| Case Report | ▴Top |
A 47-year-old male patient presented to our clinic with pain in his right hip that started 10 days ago. There was also a diffuse swelling in the 3rd finger of his left hand (Fig. 1). The patient described fever, night sweats, widespread muscle pain and fatigue that continued for the last two weeks. He did not have any history of trauma, psoriasis, diarrhoea, urethritis or any familial inflammatory arthropathy. During his physical examination, his temperature was 39 °C, blood pressure 120/70 mmHg, heart rate 98/min, and his respiration rate was 18/min. Other systemic examinations gave normal results. The locomotor system examination revealed diffuse swelling and pain in the 3rd finger of his left hand. The right sacroiliac joint was positive in terms of the compression and Mennell’s tests and the Fabere sign. The patient’s laboratory tests revealed his leukocyte count as 8 K/uL, sedimentation rate as 21 mm/h, CRP level 32 mg/dL (0 - 5 mg/dL), ALT value 116 mU/L and AST value as 99 mU/L. The serum uric acid and calcium levels and urine test results were within normal limits. The rheumatoid factor (RF), anti-nuclear antibody (ANA) and HLAB-27 tests were negative. However, the Rose Bengal test gave a positive result and Wright’s seroagglutination test was also positive for a 1/320 titre. Blood and urine cultures were obtained from the patient. On the 7th day of the blood culture, Brucella melitensis growth was detected. No infectious agents were observed to grow in the urine culture. While no pathologies were detected in the PA chest X-ray, the radiography of the left hand indicated a soft tissue swelling in the third finger. In the patient’s magnetic resonance imaging (MRI), marked fluid retention was observed around the flexor digitorum superficialis and profundus tendons at the level of the proximal phalanx of the 3rd finger of the left hand. Imaging with an intravenous contrast agent revealed contrast retention at this point (Fig. 2). The image was interpreted as diffuse inflammation in the digitorum superficialis and profundus tendons. In the MRI performed due to the pain in the patient’s right hip, the fat-suppressed T2-weighted images revealed diffuse hyperintense subchondral areas on the side of the right iliac bone facing the sacroiliac joint (Fig. 3). Contrast retention was also observed at this point during the intravenous contrast imaging performed. The image was interpreted as right sacroiliitis. Based on the patient’s complaints and the findings at hand, reactive brucella dactylitis and sacroiliitis was diagnosed and treatment was started with a combination of doxycycline (200 mg/d), rifampicin (600 mg/g), streptomycin (1gr/d) and indometacin (100 mg/d). On the 10th day of his treatment, the patient’s temperature dropped to normal and the swelling and pain in his finger healed completely. On the 19th day of his treatment, the pain in his right hip was markedly reduced. While the streptomycin treatment was ended on the 21st day, doxycycline 200 mg/d, rifampicin 600 mg/d and indometacin 100 mg/d were continued until the end of the 8th week. The patient was discharged after four weeks’ hospital stay.
 Click for large image | Figure 1. A diffuse swelling in the 3rd finger of left hand. |
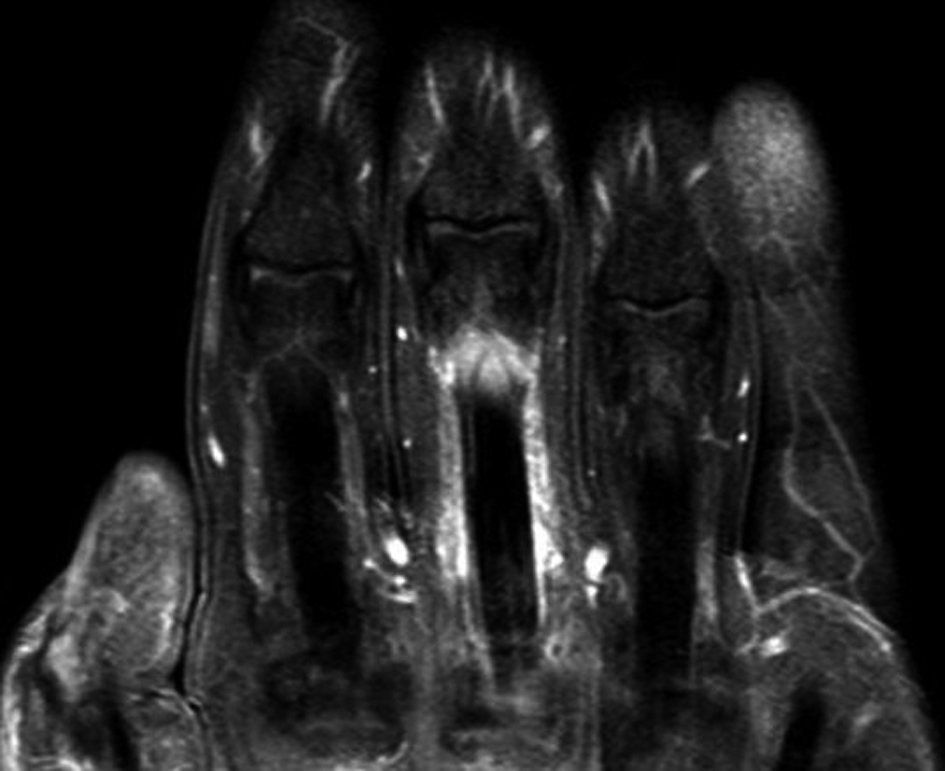 Click for large image | Figure 2. Tendon inflammation in the digitorum superficialis and profundus tendons (T1 weighted MRI with contrast). |
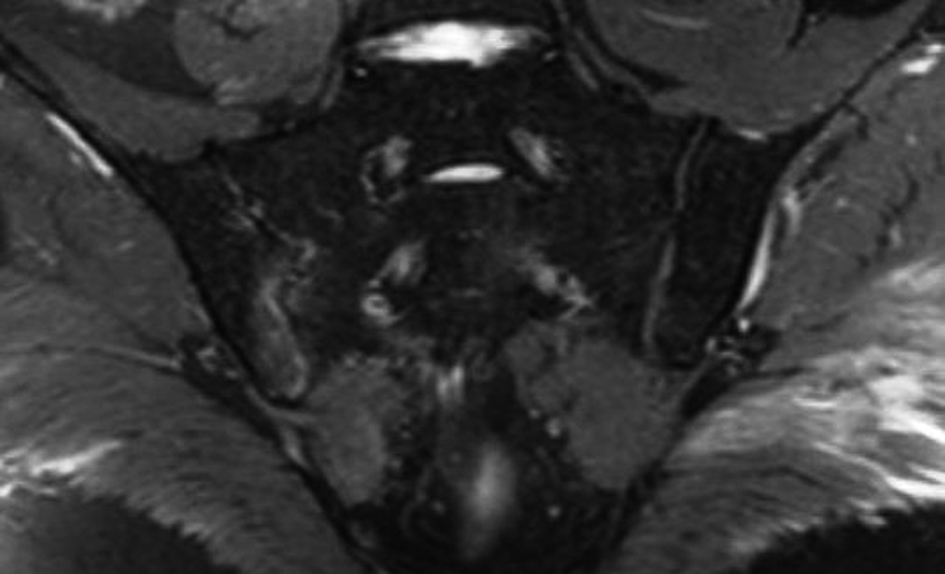 Click for large image | Figure 3. Revealed diffuse hyperintense subchondral areas on the side of the right iliac bone facing the sacroiliac joint (fat-suppressed T2-weighted MRI). |
| Discussion | ▴Top |
The frequency of osteoarticular involvement in brucellosis varies between 0-85% in the literature. This ratio has been reported as 21.3% in Spain [4], 28.5% in Iran [2], 42% in Greece [5], 47.7% in Saudi Arabia [6] and 59.2% in Macedonia [7]. In the studies conducted in Turkey, the frequency has been observed as 33.7-43% in the Mediterranean region [8-11], while it was 46.5% in the middle Anatolian region [12]. However, in a study conducted by Gur et al [13] in our region, this frequency was found as 69%.
Sacroiliitis is the most common type of osteoarticular involvement [12-15] which usually occurs unilaterally [13, 14], although there are reports claiming that bilateral involvement occurs more frequently [9, 12, 16]. Our patient also had unilateral sacroiliac joint involvement. In B.melitensis infections, 20-80% of the patients reveal findings suggesting musculoskeletal system involvement [14]. Also, Ariza et al [15] have demonstrated that the sacroiliac joint is the most commonly involved joint in patients where a B. melitensis infection is predominant. Similarly, the blood culture of our patient with sacroiliitis also indicated B.melitensis growth.
Dactylitis is characterised with arthritis in the small joints of the fingers and toes [17]. Inflammation along the finger flexor tendons, edema and enthesitis form the basic pathologies [18, 19]. Although dactylitis or ‘sausage fingers’ forms the characteristic feature of arthritis, this condition may also be observed in reactive arthritis, sarcoidosis, gout or flexor tendon sheath infections [20, 21]. Although dactylitis often occurs as an inflammation both in the joints and the flexor tendon sheaths of fingers and toes, it may also be observed in the form of isolated flexor tenosynovitis [18, 22]. Patients with brucellosis may develop bursitis and tendinitis in the periarticular region [13]. Dactylitis in a patient with brucellosis was previously reported by Ozgocmen et al [23]. Also in our case, we evaluated the diffuse swelling in the 3rd finger as brucella dactylitis and detected a diffuse tendon inflammation at the flexor digitorum profundus and superficialis in the MRI.
In a recent study, multiple articular involvement has been reported in 17% of the patients with brucellosis; with sacroiliitis and spondylodiscitis in 10 patients, sacroiliitis and peripheral arthritis in 4 patients, and sacroiliitis and bursitis in one patient [12]. As far as we know, our patient is the first case in the literature where a sacroiliitis and dactylitis are simultaneously observed. Moreover, except for the patients with brucella spondylitis [24], response to the treatment is good and fast in patients with osteoarticular involvement [25-27]. We have also observed a good response to the triple antibiotherapy in our patient.
In conclusion, dactylitis is an important feature of inflammatory arthritis and unusual complication of osteoarticular brucellosis. And also dactylitis may be found with sacroiilitis in patients with brucellosis.
Disclosure of Interests’ Conflict
All authors declared no conflicts of interest.
| References | ▴Top |
- Hall WH, Khan MY. Brucellosis. In: Hoeprich PD, Jordan MC, editors. Infectious Disease. Philadephia: JB Lippincott Company; 1989. p. 1281-82.
- Giannaccini G, Betti L, Pirone A, Palego L, Fabiani O, Fabbrini L, Mascia G, et al. Short-term effects of 3,4-methylen-dioxy-metamphetamine (MDMA) on 5-HT(1A) receptors in the rat hippocampus. Neurochem Int. 2007;51(8):496-506.
pubmed doi - Arkun R, Mete BD. Musculoskeletal brucellosis. Semin Musculoskelet Radiol. 2011;15(5):470-479.
pubmed doi - Colmenero JD, Reguera JM, Martos F, Sanchez-De-Mora D, Delgado M, Causse M, Martin-Farfan A, et al. Complications associated with Brucella melitensis infection: a study of 530 cases. Medicine (Baltimore). 1996;75(4):195-211.
pubmed doi - Andriopoulos P, Tsironi M, Deftereos S, Aessopos A, Assimakopoulos G. Acute brucellosis: presentation, diagnosis, and treatment of 144 cases. Int J Infect Dis. 2007;11(1):52-57.
pubmed doi - el-Desouki M. Skeletal brucellosis: assessment with bone scintigraphy. Radiology. 1991;181(2):415-418.
pubmed - Bosilkovski M, Krteva L, Caparoska S, Dimzova M. Osteoarticular involvement in brucellosis: study of 196 cases in the Republic of Macedonia. Croat Med J. 2004;45(6):727-733.
pubmed - Demiroglu YZ, Turunc T, Aliskan H, Colakoglu S, Arslan H. [Brucellosis: retrospective evaluation of the clinical, laboratory and epidemiological features of 151 cases]. Mikrobiyol Bul. 2007;41(4):517-527.
pubmed - Tasova Y, Saltoglu N, Sahin G, Aksu HS. Osteoarthricular involvement of brucellosis in Turkey. Clin Rheumatol. 1999;18(3):214-219.
pubmed doi - Pourbagher A, Pourbagher MA, Savas L, Turunc T, Demiroglu YZ, Erol I, Yalcintas D. Epidemiologic, clinical, and imaging findings in brucellosis patients with osteoarticular involvement. AJR Am J Roentgenol. 2006;187(4):873-880.
pubmed doi - Aydin M, Fuat Yapar A, Savas L, Reyhan M, Pourbagher A, Turunc TY, Ziya Demiroglu Y, et al. Scintigraphic findings in osteoarticular brucellosis. Nucl Med Commun. 2005;26(7):639-647.
pubmed doi - Turan H, Serefhanoglu K, Karadeli E, Togan T, Arslan H. Osteoarticular involvement among 202 brucellosis cases identified in Central Anatolia region of Turkey. Intern Med. 2011;50(5):421-428.
pubmed doi - Geyik MF, Gur A, Nas K, Cevik R, Sarac J, Dikici B, Ayaz C. Musculoskeletal involvement of brucellosis in different age groups: a study of 195 cases. Swiss Med Wkly. 2002;132(7-8):98-105.
pubmed - Serter G, Karakartal G, Gunhan C, Buke M, Yuce K, Dereli D. Clinical picture in adult brucellosis-typical and unusual. In: Tumbay E, Hilmi S, Ang O, editors. Brucella and Brucellosis in man and animals. Izmir: Publication of the Turkish Microbiological Society 1991;16:101-7.
- Ariza J, Pujol M, Valverde J, Nolla JM, Rufi G, Viladrich PF, Corredoira JM, et al. Brucellar sacroiliitis: findings in 63 episodes and current relevance. Clin Infect Dis. 1993;16(6):761-765.
pubmed doi - Cordero-Sanchez M, Alvarez-Ruiz S, Lopez-Ochoa J, Garcia-Talavera JR. Scintigraphic evaluation of lumbosacral pain in brucellosis. Arthritis Rheum. 1990;33(7):1052-1055.
pubmed doi - Olivieri I, D'Angelo S, Scarano E, Padula A. What is the primary lesion in SpA dactylitis? Rheumatology (Oxford). 2008;47(5):561-562.
pubmed doi - Olivieri I, Barozzi L, Favaro L, Pierro A, de Matteis M, Borghi C, Padula A, et al. Dactylitis in patients with seronegative spondylarthropathy. Assessment by ultrasonography and magnetic resonance imaging. Arthritis Rheum. 1996;39(9):1524-1528.
pubmed doi - Healy PJ, Groves C, Chandramohan M, Helliwell PS. MRI changes in psoriatic dactylitis—extent of pathology, relationship to tenderness and correlation with clinical indices. Rheumatology (Oxford). 2008;47(1):92-95.
pubmed doi - Dougados M, van der Linden S, Juhlin R, Huitfeldt B, Amor B, Calin A, Cats A, et al. The European Spondylarthropathy Study Group preliminary criteria for the classification of spondylarthropathy. Arthritis Rheum. 1991;34(10):1218-1227.
pubmed doi - Rothschild BM, Pingitore C, Eaton M. Dactylitis: implications for clinical practice. Semin Arthritis Rheum. 1998;28(1):41-47.
pubmed doi - Olivieri I, Barozzi L, Pierro A, De Matteis M, Padula A, Pavlica P. Toe dactylitis in patients with spondyloarthropathy: assessment by magnetic resonance imaging. J Rheumatol. 1997;24(5):926-930.
pubmed - Ozgocmen S, Ardicoglu O, Ozcakar L. Dactylitis in a patient with brucellosis. J Hand Surg Br. 2001;26(2):171-172.
pubmed doi - Ariza J, Gudiol F, Valverde J, Pallares R, Fernandez-Viladrich P, Rufi G, Espadaler L, et al. Brucellar spondylitis: a detailed analysis based on current findings. Rev Infect Dis. 1985;7(5):656-664.
pubmed doi - Serre H, Kalfa G, Brousson A, Sany J, Bertrand A, Simon L. [Osteoarticular manifestations of brucellosis. Current aspects]. Rev Rhum Mal Osteoartic. 1981;48(2):143-148.
pubmed - Colmenero JD, Porras JJ, Valdivielso P, Porras JA, de Ramon E, Cause M, Juarez C. [Brucellosis: a prospective study of 100 cases]. Med Clin (Barc). 1986;86(2):43-48.
pubmed - Alarcon GS, Bocanegra TS, Gotuzzo E, Espinoza LR. The arthritis of brucellosis: a perspective one hundred years after Bruce's discovery. J Rheumatol. 1987;14(6):1083-1085.
pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


