| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 14, Number 7, July 2023, pages 251-254
Efficacy and Safety of Carbon Dioxide Laser System in the Treatment of Scalp Sebaceous Adenoma With the Use of a New Scanner Unit
Paolo Bonana, Giustino Gallob, Irene Fuscob, c , Francesca Madeddub, Tiziano Zingonib
aLaser Cutaneous Cosmetic and Plastic Surgery Unit, Villa Donatello Clinic, Florence, Italy
bEl.En. Group, 50041 Calenzano, Italy
cCorresponding Author: Irene Fusco, El.En. Group, 50041 Calenzano, Italy
Manuscript submitted June 16, 2023, accepted July 15, 2023, published online July 31, 2023
Short title: CO2 Laser System in the Treatment of Scalp SA
doi: https://doi.org/10.14740/jmc4132
| Abstract | ▴Top |
Sebaceous adenoma (SA) is a rare solitary tumor that preferentially affects the forehead and scalp. The objective of this case report was to determine the efficacy and safety of a 10,600-nm carbon dioxide (CO2) laser device in the treatment of large scalp SA, using a new scanning system which allows to speed up the removal of the lesion. A 65-year-old male with SA on the scalp area underwent one session with the CO2 laser system. For this procedure, a new scanner system with 7-inch or 4-inch focal handpieces were used. A local anesthesia with lidocaine was performed before laser treatment. Some possible side effects such as dyschromia, burning sensation, bleeding and mild to moderate post-treatment erythema, itching, crusting, and edema, were checked. In order to monitor the effectiveness of the treatment, clinical photos that documented the patient lesion were captured before treatment and at 1 month of follow-up. The clinical and aesthetic results observed after laser procedure were excellent, with a complete remission of patient’s scalp SA lesion at 4 weeks’ follow-up. Patient satisfaction was very high, and no side effects were observed. This laser system technology allows for precise, effective, and targeted action on the lesions treated while simultaneously protecting the surrounding areas, ensuring the best possible re-epithelialization.
Keywords: Sebaceous adenoma; CO2 laser system; DermaSCAN scanner; Scalp area
| Introduction | ▴Top |
Sebaceous glands are distributed throughout the body, with the greatest number in the skin on the head and neck. They are a component on the pilosebaceous apparatus and are usually found in close association with hair follicles. The spectrum of sebaceous tumors ranges from the very common differentiated sebaceous hyperplasia to the rare and undifferentiated sebaceous carcinoma (SC) [1].
Sebaceous tumors can be grouped into three categories: sebaceous adenoma (SA), basal cell carcinoma with sebaceous differentiation, and SC [2]. Among these, SA is a rare solitary tumor that preferentially affects the forehead and scalp.
Although several treatment modalities have been reported, the full range and efficacy of options are unclear. Medications include antiandrogens, isotretinoin pills or capsules, trichloroacetic acid (rubbed onto your skin), cauterization, cryotherapy, excision, laser treatment, photodynamic therapy, and curettage [3].
Among these treatment therapeutic options, carbon dioxide (CO2) laser has demonstrated its efficacy in the SA removal with excellent results [4]. As demonstrated in a recent study [5], CO2 laser can produce considerable positive cosmetic outcomes with marked clinical improvement without any recurrence for SA removal and has been described to produce good (75%) clinical improvement and lesion shrinkage ranging from 50% to greater than 75% without lasting adverse effects.
In addition, it was also demonstrated from literature [6] that 8,040 SA lesions were successfully treated with CO2 laser. The lesions were treated with freehand handpieces in which the laser beam is fixed; and it is the physician who has to move over the lesion in order to remove it completely, and for large lesions, this procedure could be lengthy.
For these reasons, the objective of this case report was to determine the efficacy and safety of a 10,600-nm CO2 laser device in the treatment of large scalp SA, using a new scanning system which allows to speed up the removal of the lesion.
| Case Report | ▴Top |
Investigations and diagnosis
A 65-year-old male with a Fitzpatrick skin grade of III, was diagnosed with SA on the scalp area. The physical examination showed a 4 × 2 cm sized mass palpable in the center of patient’s scalp. Clinically, it occurs in the form of small skin reliefs (papules) appeared probably as a result of excessive sun exposure of the scalp area where the patient’s hair was thinner. Following the proper physical examination, a collection of patient’s anamnestic information to exclude familiarity with other more serious pathologies was done.
Treatment, follow-up and outcomes
For the treatment of SA, patient underwent one session with the CO2 laser system (DEKA MELA, Calenzano, Italy).
For this procedure, a new scanner system (DermaSCAN scanner, DEKA MELA, Calenzano, Italy) with 7-inch or 4-inch focal handpieces was used. During the initial phase, the 4-inch focal handpiece was used, and the following parameters were chosen to remove most of the lesion in a short time: power 4 - 10 W, dwell time 0.2 ms, a high-power pulse (UP/HP pulse) and cue ball for the scanning shape. In the final stages, however, the following parameters were used to refine the lesion: power 0.5 - 1 W, a high-power pulse (UP/HP pulse) and point (no scanning movement) for the shape. Finally, in order to give homogeneity and uniformity to the tissue, the following parameters were used with the 7-inch focal handpiece: power 8 - 15 W, dwell time 0.2 - 0.3 ms, CW pulse and hexagon for the shape.
This new scanning system is a microscanner that was developed for surgical dermatology treatments to enhance vaporization capability of standard freehand handpieces, and it is therefore particularly useful for those dermatological surgery treatments where larger areas need to be removed.
A local anesthesia with lidocaine was performed before laser treatment.
After treatment, it was suggested the application of topical antibiotics on the lesion covered by a hydrocolloid transparent patch. This patch has a high absorbency and can manage the exudate and secretions of the skin. The patient can remove the patch every day and wash the treated area with a cleansing foam and then reapply it, for 1 - 2 weeks, without crust formation, and protect the wound with sunscreen.
Some possible side effects such as dyschromia, burning sensation, bleeding and mild to moderate post-treatment erythema, itching, crusting, and edema, were checked.
In order to monitor the effectiveness of the treatment, clinical photos that documented the patient lesion were captured before treatment and at 1 month of follow-up. The patient’s informed consent was acquired regarding the risks, advantages, and treatment options.
The clinical and aesthetic results observed after laser procedure were excellent, as reported in Figure 1, with a complete remission of patient’s scalp SA lesion at 4 weeks’ follow-up. Patient satisfaction was very high, and no side effects were observed.
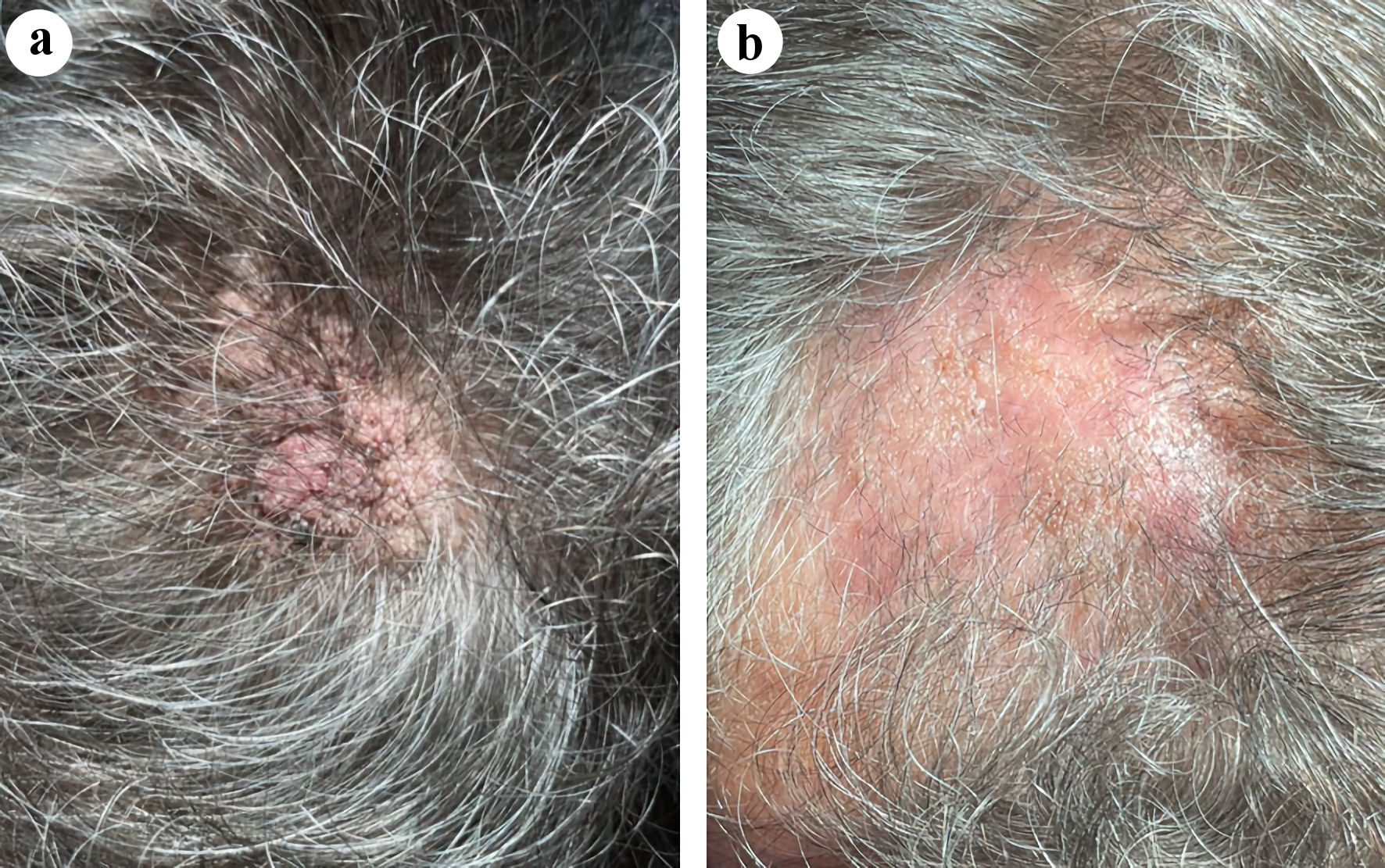 Click for large image | Figure 1. Case presentation of a 65-year-old male patient affected by sebaceous adenoma on the scalp area. (a) Before treatment. (b) A complete removal of lesion was observed at 4 weeks’ follow-up after the laser treatment session. |
| Discussion | ▴Top |
The CO2 laser has been used extensively in dermatological surgery departments and is currently recognized as the gold standard for the vaporization of soft tissues [7, 8].
The CO2 laser therapy is common successfully used for cutaneous disorder associated with cosmetic problems, such as sebaceous gland hyperplasia [9] nevus sebaceous [10] eccrine hidrocystomas [11], and common dermatosis like the severe Favre-Racouchot syndrome [12]. Recent studies also demonstrated the efficacy of this system in the management of burn and postsurgical scars [13, 14].
Furthermore, the CO2 laser can be used in any phototype and race, provides a safe and effective result for different dermatological pathologies [15].
The advantages of CO2 laser include a reduced healing time, an infrequent need for anesthesia, reduced thermal damage, less bleeding, less inflammation, and minimal undesirable side effects (unaesthetic scarring and dyschromic effects). These benefits must be considered in comparison with other available surgical techniques such as diathermo-coagulation and traditional surgery, which on the contrary necessitate frequent anesthetics, a longer recovery period, a slower cicatrization, and a high incidence of hypertrophic scars and keloids. Another relevant limitation of these two surgical treatments is its limited usage in many anatomically difficult areas such as the internal corner of the eyes, the ears, the alae of the nose, and the genital areas characterized by a high incidence of cutaneous damage upon using these techniques. The laser CO2 technique is preferred in patients with several or wide lesions, those with a pacemaker, or for patients who cannot be subjected to anesthetics [16-19].
The greater advantage of DermaSCAN is represented by its ability to speed up the ablation/vaporization procedures thanks to the specific emission modes designed for this scanner. This scanner allows to reach both a deep ablation in the tissue (first ablation phase) alternating with a more superficial and gentle vaporization (second ablation phase), which give a final definition of the skin lesion. In fact, the selection of the cue ball scan figure is indicated to perform a fast ablation generally in the initial stages of dermatological procedures when it is necessary to remove larges volumes. The selection of the point scan shape (no scanning movement, the scanner is operative but fixed on one point), instead, allow you to use the freehand handpiece without having to remove the scanner and therefore have a more superficial ablation to better definition of the lesion. Finally, the use of hexagon shape allows homogenization and uniformity of the tissue. This laser system technology actually allows for precise, effective, and targeted action on the lesions treated while simultaneously protecting the surrounding areas, ensuring the best possible re-epithelialization. As a result, it is appropriate for surgical procedures because the reduced inflammatory response promotes faster healing. Due to the application’s extreme accuracy, it is possible to vaporize the epidermis horizontally on its own or to extend the thermal effect even further into the papillary or reticular derma with a control of tissue damage and spare vertically the hair follicles while simultaneously maximizing efficacy.
Indeed, our results demonstrated the effectiveness of the treatment, with clinical photos that documented the complete remission of patient’s scalp SA lesion at 4 weeks’ follow-up. Patient satisfaction was very high, and no side effects were observed.
Our future goal will be to increase the clinical cases involving more patients to reconfirm the effectiveness of treatment.
Learning points
The purpose of the present investigation was to assess the efficacy and safety of a 10,600-nm CO2 laser device in the treatment of large scalp SA using a new scanning system (DermaSCAN) that allows for faster lesion removal. The clinical and aesthetic results observed after laser procedure were excellent, with a complete remission of patient’s scalp SA lesion at 4 weeks’ follow-up. Patient satisfaction was very high, and no side effects were observed. Our future goal will be to increase the clinical cases involving more patients to reconfirm the effectiveness of treatment.
Acknowledgments
None to declare.
Financial Disclosure
No funding was provided for this study.
Conflict of Interest
Authors IF, TZ, FM, GG were employed by El.En. Group. The remaining authors declare that the research was conducted in the absence of any commercial or financial relationship that could be construed as a potential conflict of interest.
Informed Consent
Informed consent was obtained.
Author Contributions
Conceptualization, methodology, software, investigation, project administration, and funding acquisition: PB, GG and TZ. Resources: PB, GG, FM and TZ. Writing-original draft preparation: IF and FM. Validation, formal analysis, data curation, writing-review and editing, visualization, and supervision: PB, GG, IF, FM and TZ. All authors have read and agreed to the published version of the manuscript.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
| References | ▴Top |
- Cohen PR, Kohn SR, Davis DA, Kurzrock R. Muir-Torre syndrome. Dermatol Clin. 1995;13(1):79-89.
pubmed - Rulon DB, Helwig EB. Cutaneous sebaceous neoplasms. Cancer. 1974;33(1):82-102.
doi pubmed - Farci F, Rapini RP. Sebaceous Hyperplasia. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023.
pubmed - Weston J, Apfelberg DB, Maser MR, Lash H, White D. Carbon dioxide laserbrasion for treatment of adenoma sebaceum in tuberous sclerosis. Ann Plast Surg. 1985;15(2):132-137.
doi pubmed - Liu A, Taylor MB, Sotoodian B. Treatment of sebaceous hyperplasia by laser modalities: a review of the literature and presentation of our experience with erbium-doped yttrium aluminium garnet (Er:YAG). J Drugs Dermatol. 2020;19(5):547-552.
pubmed - Campolmi P, Bonan P, Cannarozzo G, Bassi A, Bruscino N, Arunachalam M, Troiano M, et al. Highlights of thirty-year experience of CO2 laser use at the Florence (Italy) department of dermatology. ScientificWorldJournal. 2012;2012:546528.
doi pubmed pmc - Reid R. Physical and surgical principles governing carbon dioxide laser surgery on the skin. Dermatol Clin. 1991;9(2):297-316.
pubmed - Vaderhobli RM, White JM, Le C, Ho S, Jordan R. In vitro study of the soft tissue effects of microsecond-pulsed CO(2) laser parameters during soft tissue incision and sulcular debridement. Lasers Surg Med. 2010;42(3):257-263.
doi pubmed - Kavoussi H, Rezaei M, Azimi M, Kavoussi R. Combination of CO2 laser therapy and curettage for sebaceous gland hyperplasia. Acta Dermatovenerol Alp Pannonica Adriat. 2019;28(1):11-14.
pubmed - Kim KH, Lee YJ, Lew BL, Sim WY. Treatment of nevus sebaceous with carbon dioxide laser treatment combined with isotretinoin. Ann Dermatol. 2020;32(5):430-432.
doi pubmed pmc - Fazia G, Cannarozzo G, Bennardo L, Nistico SP. CO(2) laser in the management of eccrine hidrocystomas: a retrospective study. Lasers Med Sci. 2022;37(2):1365-1369.
doi pubmed - Silvaggio D, Garofalo V, Lombardo P, C DIR, Cannarozzo G, Bianchi L. Treatment of severe Favre-Racouchot Syndrome with carbon dioxide laser. Ital J Dermatol Venerol. 2023;158(3):272-274.
doi pubmed - Campolmi P, Quintarelli L, Fusco I. A multimodal approach to laser treatment of extensive hypertrophic burn scar: a case report. Am J Case Rep. 2023;24:e939022.
doi pubmed pmc - Fiorentini F, Fusco I. Synergistic sequential emission of fractional 1540 nm and 10 600 lasers for abdominal postsurgical scar management: a clinical case report. Am J Case Rep. 2023;24:e938607.
doi pubmed pmc - Andrade GB, Salguero PM, Fusco I, Galimberti DR. Clinical evaluation and experience in treatments performed with fractional CO(2) laser on Latin American skin: an observational retrospective study. Photobiomodul Photomed Laser Surg. 2023;41(7):343-349.
doi pubmed - Fitzpatrick RE. Maximizing benefits and minimizing risk with CO2 laser resurfacing. Dermatol Clin. 2002;20(1):77-86.
doi pubmed - Fitzpatrick RE. CO2 laser resurfacing. Dermatol Clin. 2001;19(3):443-451.
doi pubmed - Goldman MP. CO2 laser resurfacing of the face and neck. Facial Plast Surg Clin North Am. 2001;9(2):283-290.
pubmed - Alster TS. Cutaneous resurfacing with CO2 and erbium: YAG lasers: preoperative, intraoperative, and postoperative considerations. Plast Reconstr Surg. 1999;103(2):619-632; discussion 633-614.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


