| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 13, Number 11, November 2022, pages 545-550
Cervical Radiculopathy as a Hidden Cause of Angina: Cervicogenic Angina
New York Chiropractic and Physiotherapy Center, Hong Kong, China
Manuscript submitted October 14, 2022, accepted November 8, 2022, published online November 27, 2022
Short title: Cervicogenic Angina
doi: https://doi.org/10.14740/jmc4025
| Abstract | ▴Top |
Patients presenting with chest pain to the emergency department constitute a diagnostic challenge as 77% of the patients’ symptoms are not cardiac. Diagnostic uncertainty is a pervasive issue in primary care. A 56-year-old man presented with non-traumatic chest pain and chronic neck pain for 2 years, as well as numbness in his right third and fourth fingers for 6 months. It was not associated with palpitation, orthopnea or pedal edema. Except for hyperglycemia, no abnormal findings were found in diagnostic tests. At that time, he was being treated for type 2 diabetes using glucose-lowering drugs in order to lower his blood glucose and lessen his risk of heart disease. The cause of his chest pain remained unknown. Following a second opinion from an orthopedist, the patient was diagnosed with cervical radiculopathy and was treated with analgesics and physical therapy. Because the treatments had only provided temporary pain relief for the previous 6 months, he sought chiropractic care for pain relief. The patient’s vital signs were stable and within normal limits during the assessment. A restricted neck movement, a positive Spurling test, and hypoesthesia in the right C7 dermatome were seen. Cervical radiographs revealed degenerative spondylosis with right C5/C6 neuroforaminal stenoses and bilateral C6/C7 neuroforaminal stenoses. A provisional diagnosis of cervical spondylotic radiculopathy associated with cervicogenic angina (CA) was made. Chiropractic procedures, including cervical manipulation, instrumented soft tissue mobilization, and motorized intermittent neck traction, were performed two to three times per week. After 3 months, the patient reported that the chest pain, neck pain, and radicular symptoms had completely resolved. Repeated radiographs taken during the 11th month follow-up revealed a comparable improvement in the increased spacing of the restricted neuroforamina, which could signify a beneficial alteration related to cervical function retrieval. CA is an angina-like chest pain caused by cervical spine disorders. This study adds to our understanding of the biomechanical impact of cervical radiculopathy on chest pain, which has largely been overlooked during diagnostic workups. Once cervical radiculopathy has been identified, CA symptoms can be eased by alleviating the noxious input stemming from the pinched nerve roots.
Keywords: Cervicogenic angina; Cervical manipulation; Cervical radiculopathy; Cervical spondylosis; Chiropractic; Neuroforaminal stenosis
| Introduction | ▴Top |
Angina pectoris, or simply angina, is the medical term for chest pain or discomfort due to an inadequate supply of oxygen to the heart muscle. It is a warning symptom of a heart attack. Patients presenting with chest pain should first be evaluated by a cardiologist to rule out serious conditions such as acute coronary syndrome, pulmonary diseases, aortic dissection and spontaneous pneumothorax. If the test results are negative for cardiovascular diseases, a diagnosis of noncardiac chest pain (NCCP) is made [1, 2]. Because the cause of chest pain is poorly understood, most patients with NCCP continue to undergo exhaustive investigations and do not obtain optimal care. NCCP can be caused by esophageal, musculoskeletal, or psychiatric diseases [2]. Given that gastroesophageal reflux disease (GERD) accounts for up to 60% of esophageal causes of patients with NCCP, a proton pump inhibitor therapeutic trial for 2 - 4 weeks is a reasonable first choice approach [3]. If the response is negative, the ruling out of musculoskeletal or psychiatric comorbidity should be considered. Current options for non-GERD-related NCCP include pain modulators, psychotherapy, and cognitive behavior therapy.
Cervicogenic angina (CA) is defined as paroxysmal angina-like pain that originates from the disorders of the cervical spine or other neck structures [4]. Because CA mimics typical cardiac angina, symptoms in the elderly with cervical spondylosis are more frequently misdiagnosed [5]. Patients with CA may have suffered symptoms for longer periods of time and seen several clinicians due to conflicting cardiac exams. Clinicians and patients are unaware that CA symptoms are stemming from cervical spine disorders. However, the mechanism of pain occurrence in patients with CA remains unclear.
Several pathological causes of pain in CA have been hypothesized, including cervical radiculopathy due to nerve root dysfunction [6], cervical myelopathy due to lesions of the dorsal the spinal cord [5, 7], sympathetic fiber distribution [8, 9], and referred pain induced by localized lesions in the neck (such as facet syndrome, disc degeneration, or disease of the longitudinal ligament) [5, 10, 11]. The specific pathogenic mechanisms implicated in a CA case, once identified, can be successfully addressed with conservative interventions or various surgical procedures in refractory cases [12, 13]. Cervical arthroplasty and total disc replacement are well-established alternatives to traditional fusion surgery [12].
Cervical spondylosis is a very common natural wear condition that worsens with age. The masquerading of CA as typical cardiac angina can result in wasteful repeated cardiac workups and a disregard to recognizing the link between cervical pathologies and CA symptoms. In this case, the patient complained of non-traumatic chest pain and neck pain accompanied by numbness in his right third and fourth fingers, and CA was disregarded throughout a 2-year evaluation. This study contributes to a better understanding of the role of pain processing in the development of CA. Compression of the C4-C8 (prefixed brachial plexus) nerve roots, which carry innervation to the pectoralis muscles, can cause pain in the anterior chest wall [5-7]. This example demonstrates that awareness of other sources of pain will reduce unnecessary cardiac investigations and treatment regimens. Radiculopathy-associated CA symptoms can be eased by relieving the noxious input stemming from the pinched cervical nerve roots, as seen by an increase in the spacing of the restricted neuroforamina.
| Case Report | ▴Top |
Investigations
A 56-year-old man presented with 2 years of paroxysmal upper chest pain and chronic neck pain, as well as 6 months of numbness in his right third and fourth fingers. His symptoms were insidious in onset and he had no recent history of trauma or cardiovascular disease. His family has no history of similar illness. The patient began experiencing paroxysmal chest pain and neck pain 2 years before seeking chiropractic care. He denied experiencing palpitations, orthopnea or pedal edema. Stress 12-lead echocardiography, assessment of cardiac enzymes, and computed tomography coronary angiogram were used at the time to rule out serious cardiovascular disorders. Except for hyperglycemia, diagnostic tests revealed no significant findings. His primary care physician diagnosed him with type 2 diabetes and prescribed him glucose-lowering medications to lower his blood glucose and lessen his risk of heart disease. The cause of his chest pain was still unknown. However, his chest pain and neck pain had been worse during the last 6 months, and numbness in his right third and fourth fingers developed. After a second opinion from an orthopedist, based on his clinical presentation and corresponding radiographic findings, the patient was diagnosed with cervical radiculopathy and treated with pain medication (acetaminophen and ibuprofen), cervical traction, and physical therapy. Because the treatments only provided temporary pain relief, he sought chiropractic care for treatment of his pain.
Diagnosis
The patient was in generally good condition at the time of presentation, with stable vital signs. The left sternocleidomastoid, bilateral trapezius, pectoral muscles, and right levator scapulae were all shown to be hypertonic. Neck extension was limited to 30° (normal: > 70°), and bilateral rotation was limited to 50° (normal: > 90°). Chest pain and numbness in the right fingers were both replicated by the Spurling compression test. The patient’s pain severity was reported as 5/10, with 0 representing no pain and 10 signifying the most severe agony. On the neurological evaluation, the motor strength of the right biceps was 4/5, and mild hypoesthesia was noted in the right C7 dermatome. Cervical radiographs showed narrowed interspaces from C4/C5 through C7/T1 levels, anterior osteophytic lipping of the cervical vertebrae, and neuroforaminal stenosis due to posterior osteophyte encroachment at the right C5/C6 and bilateral C6/C7 levels (Figs. 1 and 2). The clinical presentation and concordant radiographic findings were consistent with a diagnosis of cervical radiculopathy and concomitant CA. Chest pain is a symptom with a wide differential diagnosis, which includes potentially fatal conditions such as acute coronary syndrome, aortic dissection, and pulmonary embolism. In the differential diagnosis, no concurrent ECG abnormalities, normal cardiac enzymes, no response to antianginal medications, paraesthesia in the fingers, and unpredictable symptoms are helpful [14]. As a part of diagnostic algorithms, manual evaluation is recommended to assist in ruling in musculoskeletal causes. When a patient exhibits neurological symptoms suggestive of cervical root compression, it is rather easy to identify CA with a strong sense of suspicion [5].
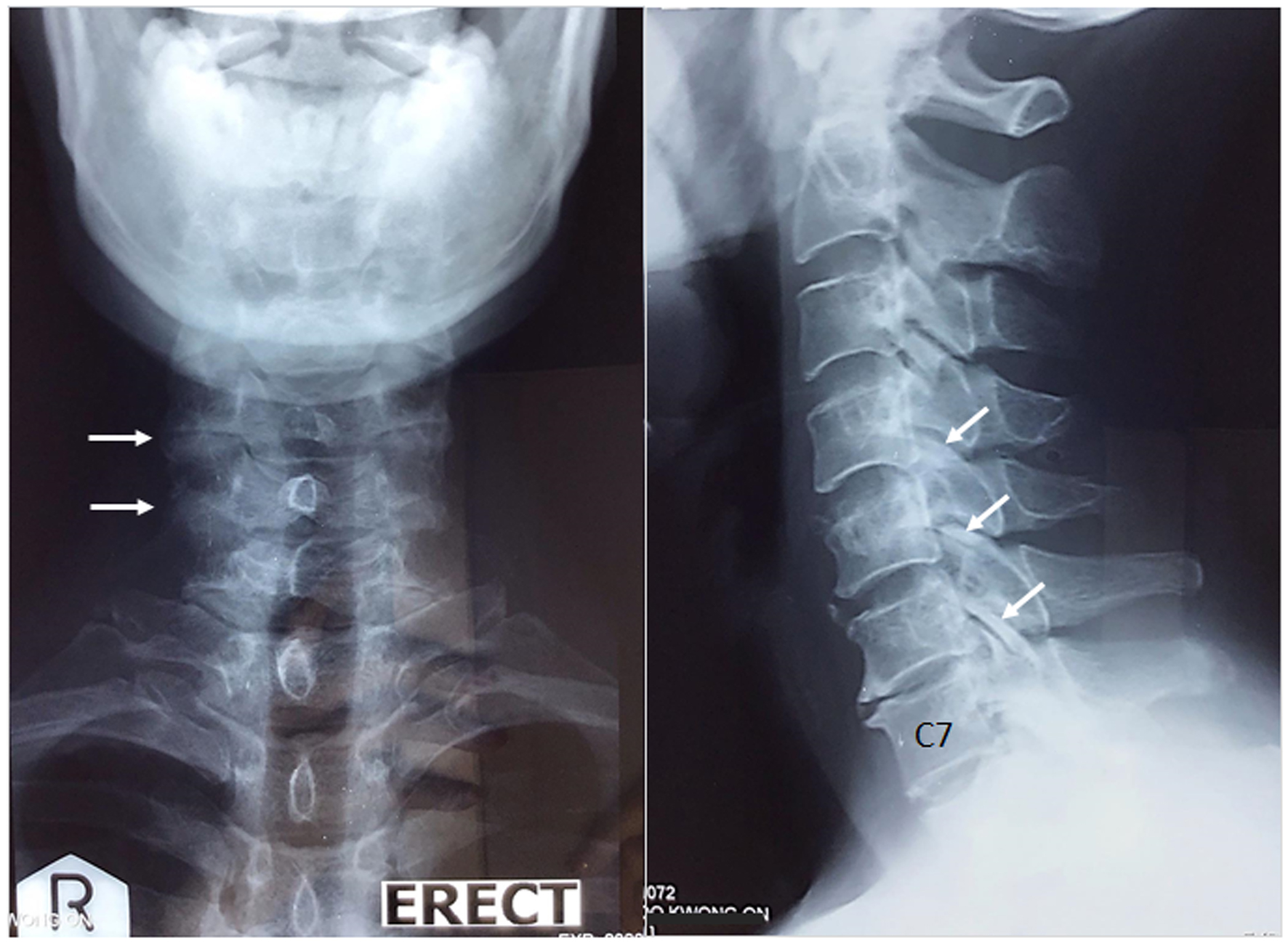 Click for large image | Figure 1. Anterior and lateral views of the cervical spine. Cervical radiographs show narrowed interspaces from C4/C5 to C7/T1 levels, anterior osteophytic lipping of the cervical vertebrae, degenerative hypertrophy of the facet joints (white arrows), and calcified discs of the C2/C3 and C4/C5 spaces. The radiographic findings are consistent with degenerative spondylosis. |
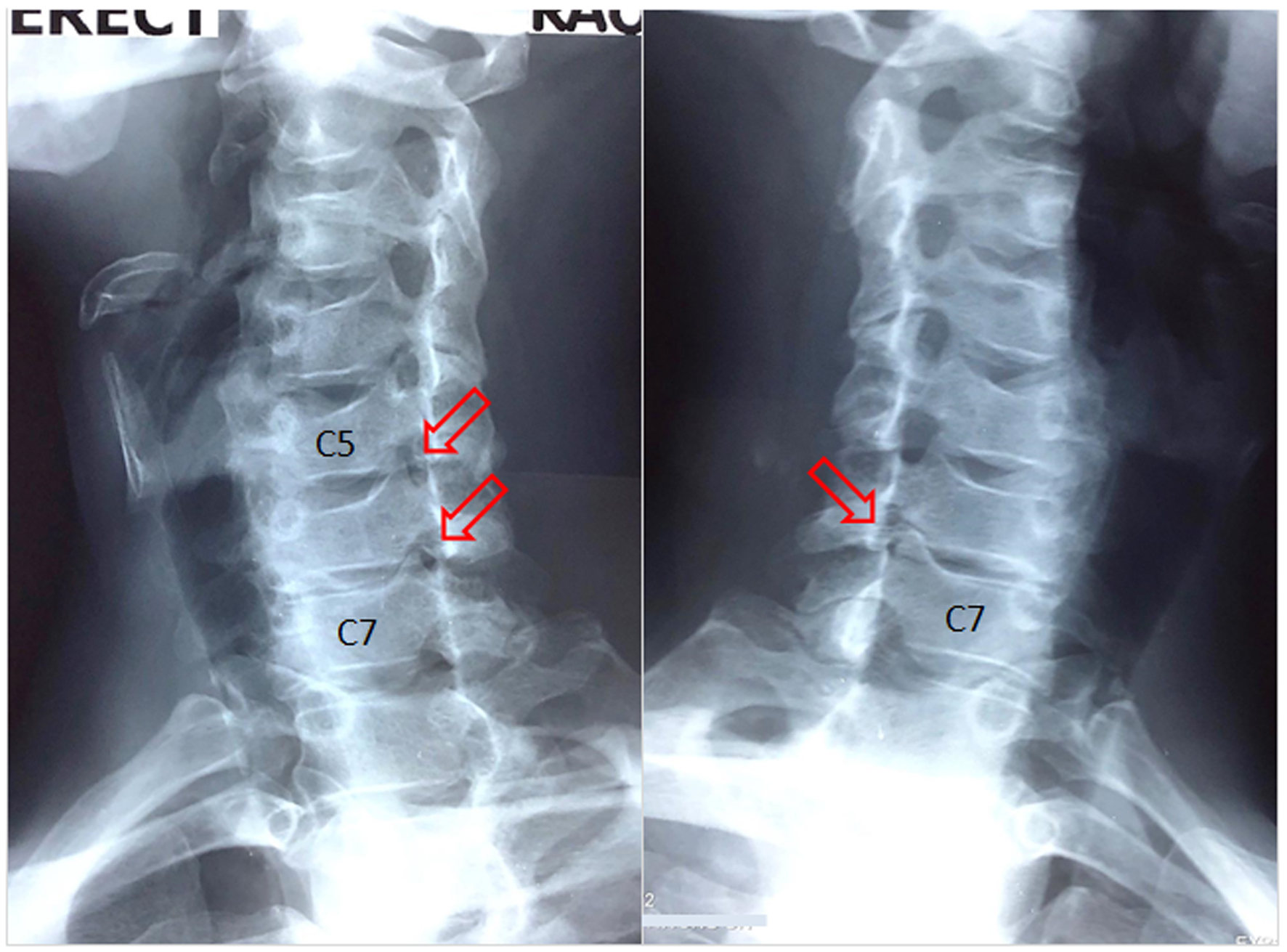 Click for large image | Figure 2. Oblique radiographs of the cervical spine demonstrate neuroforaminal stenosis with posterior osteophyte encroachment at the right C5/C6 and bilateral C6/C7 levels (red arrows), consistent with the impression of cervical radiculopathy. |
Treatment
Chiropractic care aims to alleviate neck pain, improve cervical alignment, restore cervical mobility, and prevent neurological damage. The treatment approach included a high-velocity and low-amplitude spinal manipulation used to treat cervical dysfunction, as well as instrument-assisted soft tissue mobilization to treat the hypertonic muscles. For the first month, treatment sessions were arranged three times each week.
Follow-up and outcomes
The patient reported a 50% improvement in chest pain, neck pain, and radicular symptoms within the first 2 weeks of treatment. His numeric pain scale rating was reduced from 5 to 2 on the 1-10 scale. Motorized intermittent traction was applied 1 month later to decompress the disc space and release the pinched nerve roots. The treatment sessions were reduced to two per week for 2 months. After 3 months, the patient reported complete resolution of neck or chest pain and paraesthesia, and regained neck mobility. Analgesic medicines were discontinued, and the patient received monthly chiropractic maintenance care. During the 11th month follow-up, the radiographs demonstrated that the narrowed neuroforamina had greater spacing than the original findings on visual assessment (Fig. 3). He is currently pain-free. There were no pathological or treatment-related adverse effects observed.
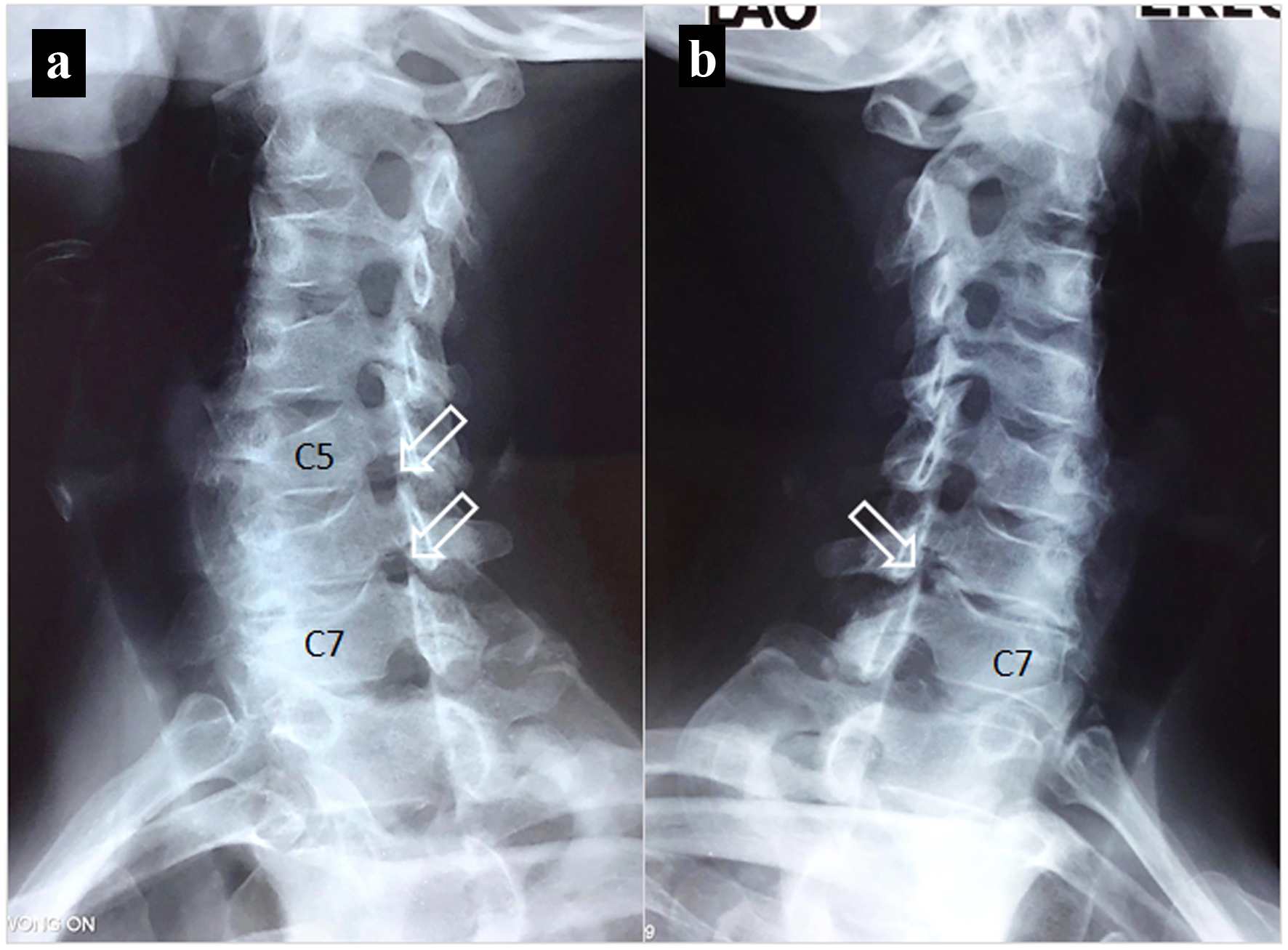 Click for large image | Figure 3. Images obtained 11 months following treatment. (a) The neuroforamina of the right C5/C6 and C6/C7 levels are opened (white arrows). (b) The restricted left C6/C7 opening has greater space than the original finding in Figure 2 on visual assessment. An increase in the spacing of the previously restricted neuroforamina could signify a beneficial alteration related to cervical function improvement. |
| Discussion | ▴Top |
Angina pain is frequently described as a pressure feeling of squeezing, heaviness, tightness, or pain in the chest. It is a frequent symptom that prompts people to seek emergency medical attention [14]. According to the 2021 American Heart Association/American College of Cardiology (AHA/ACC) clinical practice guidelines, people with acute chest pain or symptoms resembling chest pain should seek medical attention right at once. Although most patients will not have a cardiac cause, all patients should be evaluated to ensure the early identification or exclusion of life-threatening causes [14]. The exact mechanism by which myocardial ischemia causes chest pain remains obscure but chemical and mechanical stimulation of sensory afferent nerve endings in the coronary arteries and myocardium is now recognized as a major factor in the progression of cardiac angina [15]. The nociceptive C-fibers of the spinal cardiac afferent fibers arising from dorsal root ganglions are dispersed throughout the ventricle, expressing a variety of ion channels or receptors and contributing to the processing of general cardiac nociception [16]. Typical cardiac angina is mediated by the spinal cardiac afferents via pathways from the spinal cord to the thalamus and, ultimately, the cerebral cortex [17].
CA is an uncommon and sometimes overlooked cause of non-cardiac chest pain that mimics true angina pectoris but is caused by cervical spine disease [12]. CA has been described as sharp, aching, or crushing and it may be accompanied by neck pain, stiffness, headache, shoulder, and arm pain. Due to delays in appropriate diagnostic evaluation during thorough cardiac checkups, the prevalence of CA remains unknown [12]. Cervical imaging can be used to discover anatomical abnormalities once coronary artery disease has properly been ruled out. Plain radiographs or magnetic resonance imaging displaying degenerative changes in the spine, such as narrowing of the disc space, formation of osteophytes, and neuroforaminal encroachment, are crucial in establishing a diagnosis of CA [12]. In addition to cervical radiculopathy [6], other cervical pathologies can also cause chest pain, such as myelopathic [5, 7], sympathetic [8, 9], and referred pain [5, 10, 11]. Electromyography can be used to corroborate image findings [7].
CA is under recognized and appears to be neglected in ordinary clinical practice [5]. CA has been described as most commonly associated with radicular pain in the lower cervical spine [7]. It is reported that between 70% [6] and 72.6% [13] of cases with CA can be attributed to compression of the cervical nerve root. The anterior branches of the C5-C8 and T1 nerves, which are typical plexus structures, come together to form the intricate neural network known as the brachial plexus. The brachial plexus arises from the cervical spinal cord and passes over the first rib into the axillae via the cervicoaxillary canal, supplying somatic motor and sensory innervation to the upper limbs and pectoral girdle [18]. There are several anatomical variations of the plexus, including the prefix (C4-C8) and postfix (C6-T2) variations. The prefixed brachial plexus occurs in 26-48% of the population, while the postfixed brachial plexus is present in up to 4% [19]. A correlation study of 438 patients with CA reported that compression of the C4-C8 (prefixed brachial plexus) nerve roots, which transmit sensory and motor innervation through the medial and lateral pectoral nerves to the pectoralis muscles, results in radicular pain in the anterior chest wall [6]. The C6 and C7 nerve roots are the most commonly involved, accounting for 67% of CA patients with spondylotic radiculopathy [7]. Case series have reached similar conclusions regarding chest pain caused by cervicothoracic nerve root compression [5, 7]. In turn, the efficacy of cervical discectomy and fusion in relieving symptoms supports the notion that cervical nerve root compression is one of the causes of cervical angina [4].
Conservative regimen and symptom management are effective options for cervical spondylotic radiculopathy [20]. The majority of CA patients responded satisfactorily to the usual nonsurgical treatment [7]. Nonsurgical treatments include neck braces, physiotherapy or manual therapy for muscle strengthening, cervical traction and stretching for stabilization, and pharmacological treatments, such as nonsteroidal anti-inflammatory drugs and muscle relaxants. The hazards of surgery can be avoided with nonsurgical treatments [20]. When conservative treatments fail to improve patients’ neurological compromise, surgical intervention may be required [4, 5].
A growing body of evidence supports the application of manual therapy and exercise to treat mechanical neck pain like cervical radiculopathy [21, 22]. Cervical manipulation, instrument-assisted soft tissue mobilization, and motorized intermittent neck traction were used in this patient. After 3 months of treatment, the patient reported total remission of chest and neck pain and paraesthesia, as well as restoration of cervical mobility. On follow-up radiographs, there was a comparable improvement in the increased spacing of the previously restricted neuroforamina on visual assessment (Fig. 3), which could signify a beneficial alteration related to cervical function retrieval. In general, chiropractic therapy is regarded to be helpful in alleviating radiculopathy symptoms because it breaks up tissue adhesions, releases pinched nerve roots, and increases muscle strength and neck function [21].
The following limitations of this study should be addressed. First, it was limited by the incompleteness inherent in a retrospective chart review. The results of the cardiac workup were simply obtained from referral records. Second, CA was diagnosed mostly on the basis of the patient’s medical history and the exclusion of other disorders that could explain the symptoms. There is a lack of scientific testing to determine the presence of pain and CA symptoms. However, radiography is an ancillary technique that primarily relies on visual inspection to recognize and assess anatomical changes in medical images. Visual assessment of neuroforaminal stenosis is limited by its subjectivity and insufficient sensitivity. Furthermore, multimodal interventions were used to treat this patient. As a result, determining the precise efficacy of chiropractic techniques, massage, and strengthening exercises is impossible. Further investigation into the mechanisms of symptom alleviation and function retrieval is needed. The strength of this study is that it provides evidence that non-cardiac angina can be caused by cervical painful stimuli such as cervical spondylotic radiculopathy, and that the symptoms of CA can be eliminated by reducing the noxious input coming from the cervical pain sources.
Learning points
Cervical spondylosis and chest pain are both very common among the elderly. Clinicians and patients alike are frustrated and concerned when a serious condition goes undiagnosed due to inadequately explained chest pain. Patients are often evaluated to rule out cardiac causes first, and their cervical spine disorders are likely to be overlooked. A strong sense of suspicion and awareness of other sources of pain will reduce unnecessary cardiac investigations and treatment regimens used throughout health care delivery.
This study supports the relationship between cervical nerve root compression and CA. Therapeutic approaches should target the sources of pain that have been identified.
In this example, the decompression of the disc space and release of the pinched nerve roots with neck manipulation alleviated chest pain, neck pain, and radicular symptoms. The comparable radiographic changes in the restricted neuroforamina that correspond to symptom improvement were illustrated.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Informed consent was obtained from the patient for case publication.
Author Contributions
EC conceived the study, reviewed literature, and wrote the manuscript.
Data Availability
The author declares that data supporting the findings of this study are available within the article.
Abbreviations
ACC: American College of Cardiology; AHA: American Heart Association; CA: cervicogenic angina; ED: emergency department
| References | ▴Top |
- Meresh E, Piletz J, Halaris A. Noncardiac chest pain: systematic review of the literature on prognosis. Res Rep Clin Cardiol. 2018;9:1-9.
doi - Wertli MM, Dangma TD, Muller SE, Gort LM, Klauser BS, Melzer L, Held U, et al. Non-cardiac chest pain patients in the emergency department: Do physicians have a plan how to diagnose and treat them? A retrospective study. PLoS One. 2019;14(2):e0211615.
doi pubmed - Kim JH, Rhee PL. Recent advances in noncardiac chest pain in Korea. Gut Liver. 2012;6(1):1-9.
doi pubmed - Feng F, Chen X, Shen H. Cervical angina: a literature review on its diagnosis, mechanism, and management. Asian Spine J. 2021;15(4):550-556.
doi pubmed - Nakajima H, Uchida K, Kobayashi S, Kokubo Y, Yayama T, Sato R, Inukai T, et al. Cervical angina: a seemingly still neglected symptom of cervical spine disorder? Spinal Cord. 2006;44(8):509-513.
doi pubmed - Brodsky AE. Cervical angina. A correlative study with emphasis on the use of coronary arteriography. Spine (Phila Pa 1976). 1985;10(8):699-709.
doi - Sussman WI, Makovitch SA, Merchant SH, Phadke J. Cervical angina: an overlooked source of noncardiac chest pain. Neurohospitalist. 2015;5(1):22-27.
doi pubmed - Cloward RB. Cervical diskography. A contribution to the etiology and mechanism of neck, shoulder and arm pain. Ann Surg. 1959;150:1052-1064.
doi pubmed - Nakae Y, Johkura K, Kudo Y, Kuroiwa Y. Spinal cord infarction with cervical angina. J Neurol Sci. 2013;324(1-2):195-196.
doi pubmed - Sudo H, Goto R. Cervical angina because of ossification of the posterior longitudinal ligament. Spine J. 2012;12(2):169.
doi pubmed - Chien JT, Hsieh MH, Yang CC, Chen IH, Lee RP. Anterior cervical discectomy and fusion versus conservative treatment for cervical angina conservative treatment. Clin Spine Surg. 2021;34(9):E514-E521.
doi pubmed - Jammal OMA, Diaz-Aguilar LD, Srinivas S, Plonsker J, Sahyouni R, Pham MH. Cervical arthroplasty in the treatment of cervical angina: case report and review of the literature. Neurospine. 2020;17(4):929-938.
doi pubmed - Brown NJ, Shahrestani S, Lien BV, Ransom SC, Tafreshi AR, Ransom RC, Sahyouni R. Spinal pathologies and management strategies associated with cervical angina (pseudoangina): a systematic review. J Neurosurg Spine. 2020;34(3):506-513.
doi pubmed - Gulati M, Levy PD, Mukherjee D, Amsterdam E, Bhatt DL, Birtcher KK, Blankstein R, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR guideline for the evaluation and diagnosis of chest pain: executive summary: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021;144(22):e368-e454.
doi - Dusi V, Ardell JL. Brain-heart afferent-efferent traffic. In: Govoni S, Politi P, Vanoli E editors. Brain and heart dynamics. Cham: Springer International Publishing 2020. p. 3-24.
doi - Wang X, Kanda H, Tsujino T, Kogure Y, Zhu F, Yamamoto S, Sakaguchi T, et al. Reactive oxygen species cause exercise-induced angina in a myocardial ischaemia-reperfusion injury model. Int J Mol Sci. 2022;23(5):2820.
doi pubmed - Foreman RD. Mechanisms of cardiac pain. Annu Rev Physiol. 1999;61:143-167.
doi pubmed - Knipe H, Hacking C. Brachial plexus. Reference article, Radiopaedia.org. (Accessed on Jul 16, 2022).
doi pubmed - Kuzma SA, Doberstein ST, Rushlow DR. Postfixed brachial plexus radiculopathy due to thoracic disc herniation in a collegiate wrestler: a case report. J Athl Train. 2013;48(5):710-715.
doi pubmed - Luyao H, Xiaoxiao Y, Tianxiao F, Yuandong L, Ping W. Management of cervical spondylotic radiculopathy: a systematic review. Global Spine J. 2022;12(8):1912-1924.
doi pubmed - Chu ECP. Alleviating cervical radiculopathy by manipulative correction of reversed cervical lordosis: 4 years follow-up. J Family Med Prim Care. 2021;10(11):4303-4306.
doi pubmed - Sterling M, de Zoete RMJ, Coppieters I, Farrell SF. Best evidence rehabilitation for chronic pain part 4: Neck Pain. J Clin Med. 2019;8(8):1219.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


