| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 13, Number 7, July 2022, pages 359-364
Reducing Cervical Retrolisthesis With Long-Term Monthly Chiropractic Maintenance Care: A Case Report
New York Chiropractic and Physiotherapy Centre, Hong Kong, China
Manuscript submitted May 24, 2022, accepted July 1, 2022, published online July 20, 2022
Short title: Reduction of Cervical Retrolisthesis
doi: https://doi.org/10.14740/jmc3960
| Abstract | ▴Top |
The present case study aimed to demonstrate the subtle effectiveness of 13-year chiropractic maintenance care (MC) in a patient with cervical radiculopathy associated with retrolisthesis. Retrolisthesis is the backward slippage of one vertebral body with respect to the subjacent vertebra. This slippage can lead to spinal nerve root compression or irritation (radiculopathy). A 44-year-old woman presented with relapsing episodes of pain in her neck radiating down her right arm and hand for 12 months. Neurological examination revealed sensory deficits in the right C5 dermatome. Cervical radiography showed grade 1 retrolisthesis of C3 on C4 and of C4 on C5, and sclerosis over the upper endplate of the C4, C5, and C6 vertebrae. The patient was diagnosed with right C5 radiculopathy associated with vertebral retrolisthesis. She was conservatively treated with multimodal chiropractic care comprising cervical manipulation applied to the affected segments, axial distraction, and isometric stretching. After 20 sessions over 3 months of therapy, the patient experienced complete relief of neck pain and radicular symptoms, and full cervical mobility. Because her complaints were characterized by relapsing episodes, she was enrolled in a monthly MC program to monitor and ensure the spine was functioning at its highest capacity. The MC program included disease monitoring, manipulation of dysfunctional segments, cervical strengthening exercises, and ergonomics coaching. Monthly care was shown to be successful in maintaining an asymptomatic status. Moreover, a gradual reduction in cervical retrolisthesis was observed during the 13-year MC period, and the ongoing MC ensured optimal spine functioning.
Keywords: Cervical alignment; Maintenance care; Radiculopathy; Retrolisthesis; Spinal manipulation; Spondylolisthesis
| Introduction | ▴Top |
The spine consists of 33 individual vertebrae stacked one on top of the other. Spondylolisthesis is a Latin-derived term for slipped vertebra, which is diagnosed by a vertebral slippage of ≥ 2 mm in relation to the adjacent vertebra on a neutral lateral radiograph [1]. Anterolisthesis refers to forward slippage of the upper vertebra, whereas retrolisthesis is backward slippage. The direction of slippage depends on the surrounding structures and biomechanics impacted. Spondylolisthesis is commonly classified as dysplastic, isthmic, degenerative, traumatic, and pathologic by etiology. In the neck, trauma and degeneration are the most common causes of cervical spondylolisthesis [2, 3]. When the degenerative process occurs, cervical biomechanics and stability alter, allowing spondylolisthesis to occur [3]. Patients may present with neck stiffness and pain radiating into the shoulders.
Degenerative spondylolisthesis can be managed conservatively or surgically depending on the grade of the slippage and its associated neurological deficits. Muscle imbalance is associated with functional disability in patients suffering from degenerative spondylolisthesis. Neck pain and muscle spasms can be temporarily relieved in most patients during the initial phase of manipulative therapy [4, 5], so the spinal function can return to a balanced state [6]. Notably, manual interventions are not aimed at correcting the slippage. Even if the slippage has been adjusted directly, normal load-bearing structures of the manipulated segment will be unable to sustain the effect in the long term [7]. To this point, degenerative spondylolisthesis is characterized by relapsing episodes of an ongoing nature that often require long-term rehabilitation.
Maintenance care (MC) is a lengthy approach delivered in regularly spaced visits, assuring patients continue to retain maximal spinal function after completing a prescribed course of manipulative therapy [8, 9]. A favorable early treatment response is an indication for MC in patients with recurrent and persistent spinal pain [9]. The core elements of chiropractic MC are periodic examinations and manual therapy. Stability exercises and general lifestyle coaching are also often included in MC [10]. The effectiveness of chiropractic care is presumably related to core strengthening and spinal stability [6, 7]. Stabilization of the spine may alleviate symptoms and prevent progression of the slippage [2]. Chiropractic is a popular form of health care to treat musculoskeletal ailments. Approximately 22-41% of patients in Nordic countries visit a chiropractor for MC [8].
The purpose of this case report is to describe the effectiveness of long-term MC adjuvant to the initial manipulative therapy. This report demonstrates prompt alleviation of neck pain and radicular symptoms attributed to degenerative cervical retrolisthesis by multimodal chiropractic intervention, and the gradual regression of cervical retrolisthesis during 13 years of subsequent MC. The positive results recounted in this paper are consistent with those of recent reports that found symptom relief in the initial phase and regression of cervical slippage (anterolisthesis/retrolisthesis) after months of chiropractic care [4, 5]. The MC strategy requires only a slightly higher number of planned visits and should be considered as an adjuvant treatment for selected patients with persistent spinal pain who respond well to an initial course of manipulative therapy [9].
This article does not involve any studies with humans or animals performed by the author. The author presents the following article in accordance with the CARE reporting checklist.
| Case Report | ▴Top |
Investigations
A 44-year-old woman sought chiropractic attention in 2008 for relapsing episodes of neck pain, numbness, and tingling radiating down her right lateral forearm and hand. She often experienced shoulder stiffness, especially at the end of the day. The above issues had plagued her for more than 1 year and were likely linked to workplace stress, poor ergonomics, and poor sleeping postures. Short periods of rest could provide her with short-term relief. There was no history of antecedent trauma or relevant family information. Twelve months prior to the chiropractic presentation, the patient visited her orthopedist for similar symptoms. Previous magnetic resonance imaging revealed negative results. She was diagnosed with right C5 radiculopathy associated with degenerative spondylolisthesis. She was treated with cervical axial traction, exercise therapy, and pain medications. However, these treatments were not effectively curative. As such, she sought chiropractic attention for her neck pain and neurological symptoms.
Diagnosis
At the initial presentation, the patient presented with a guarded neck posture. She reported relapsing episodes of neck pain and neurological deficits in the right upper extremity. Symptoms also included a decrease in work performance and sleeping difficulties. The neck motion was restricted at 40°/70° extension, 60°/80° flexion, and 60°/90° rotation. Hypertonicity of the bilateral trapezius, right splenius capitis, and right sternocleidomastoid muscles were present. World Health Organization Quality of Life (WHOQOL) scoring was performed, and the scores were linearly transformed to a 0 - 100 scale. The patient’s score was 64. The Valsalva and neutral cervical compression tests were negative, whereas the Spurling compression test was positive on the right side. Symptoms of the right upper extremity were provoked by upper limb tension tests and alleviated by the arm abduction test. Manual muscle tests and deep tendon reflexes were normal in the upper and lower limbs bilaterally.
Dynamometry hand-grip strength measurement revealed 40/38/40 (left) vs. 60/58/60 (right), which was considered as a reasonable difference with greater grip strength in the dominant hand. Neurological examination revealed sensory deficits in the territory of the right C5 dermatome and motor weakness in the right deltoid and biceps.
Cervical radiography revealed posterior slippage of C3 on C4 and C4 on C5, with sclerosis over the upper endplate of the C4, C5, and C6 vertebrae (Fig. 1a). Disc space narrowing was not significant in the cervical spine. Other pathologies (e.g., fracture, cancer, and infection) were excluded on radiography. The patient was diagnosed with right C5 radiculopathy associated with degenerative spondylolisthesis.
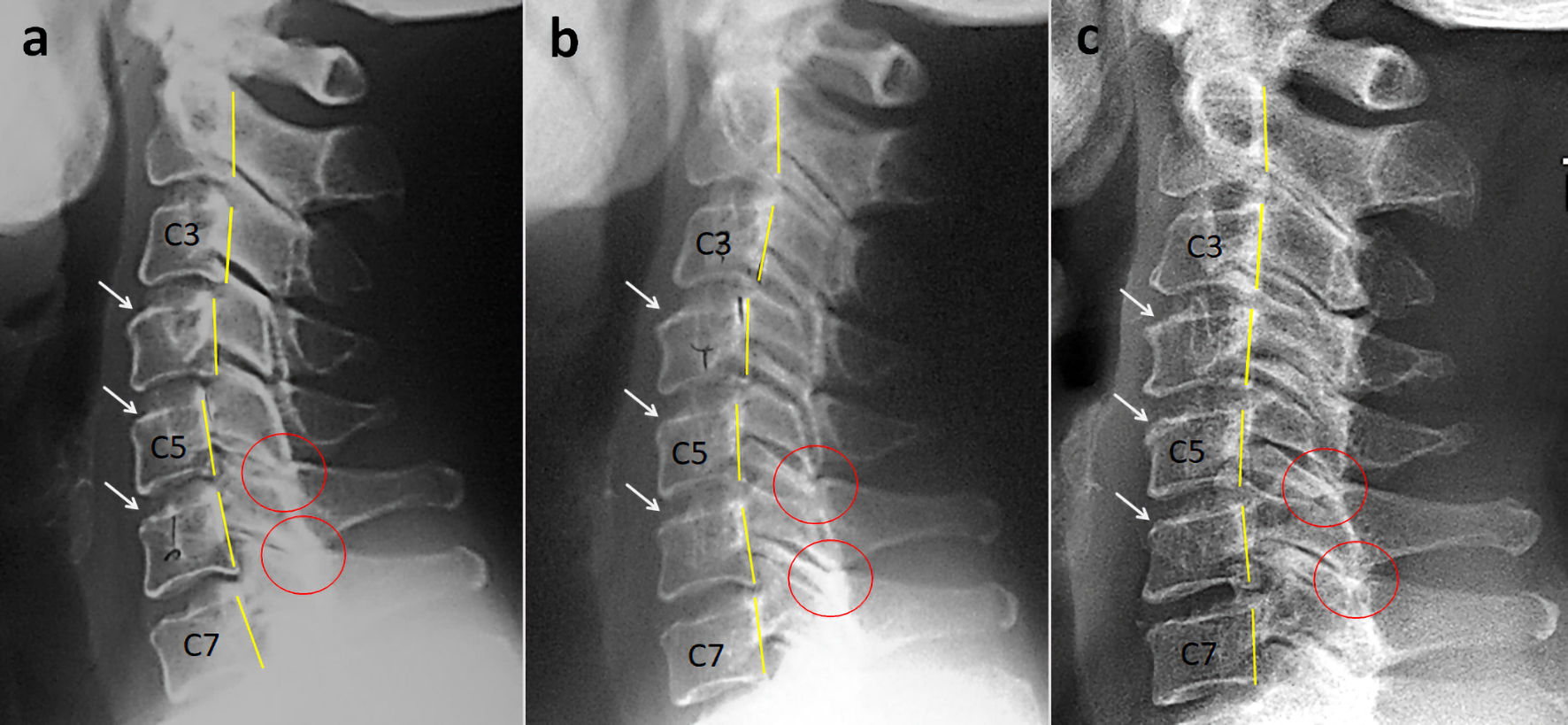 Click for large image | Figure 1. Radiography of a 44-year-old woman comparing the cervical alignment on the lateral view. (a) Lateral radiograph of the cervical spine at initial presentation shows grade 1 retrolisthesis with less than 25% posterior translation of C3 on C4 and C4 on C5 vertebrae (yellow lines highlight the posterior vertebral body margins). The inferior articular processes of C5 and C6 are lying on top of the superior articular processes of the below vertebrae (known as perched facets, highlighted by red circles). In addition, there is upper endplate sclerosis over the C4, C5, and C6 vertebrae (white arrows). (b) The radiograph obtained at the 4-year follow-up in 2013 demonstrates reduction of cervical retrolisthesis at all levels. (c) On the cervical radiograph taken in 2022, restoration of cervical alignment is observed after 13 years of manual maintenance care. |
Treatment
Chiropractic intervention aims to reduce neck pain and instability, restore cervical mobility, and prevent neurological loss. The approach included high-velocity, low-amplitude cervical manipulation applied to the restricted levels, long axial distraction of the cervical segments above the C5, and post-isometric stretching to lengthen the hypertonic muscles. Treatment sessions were scheduled thrice a week for the first phase. After 4 weeks of treatment, the patient reported a 50% reduction in neck discomfort and neurological symptoms. She was able to hold the neck in an upright posture. The frequency of treatment sessions was then reduced to once a week for 2 months. Strength training exercise focused on releasing muscular tightness and joint restriction was added to help reduce pain and radicular symptoms. Three months after initiating treatment, she reported total remission of symptoms and full cervical mobility. Therefore, the pain medications were stopped. The WHOQOL score improved from 64 to 98 that indicated a better quality of life. The patient was then enrolled in an elective MC program.
Follow-up and outcomes
The patient in this study underwent monthly scheduled MC visits. MC included disease monitoring, cervical manipulation, home exercise programs, ergonomics, and lifestyle advice [9, 10]. The main tools for relapse prevention are close monitoring for early warning signs of a worsening condition and modified treatment care until the patient is once again suitable to continue the MC plan. A two-component personalized exercise program (comprising cervical and scapular strengthening) was assigned, and the patient was asked to record adherence to her program on an exercise log. Supine craniocervical flexion was performed as a cervical strengthening exercise to recruit the deep neck flexors without engaging the superficial neck muscles [11]. The patient performed three sets of ten contractions (holding for 10 s each) to obtain optimal muscle activation. Craniocervical flexion contractions in a seated position were also conducted with 30 repetitions of 10 s holds serving as the objective. Her scapular strengthening exercises comprised prone horizontal abduction, forward flexion in the side-lying position, prone shoulder extension, and push-ups with an emphasis on shoulder protraction. Each exercise consisted of three sets of ten repetitions [12].
The patient occasionally experienced episodes of mild neck pain, which subsided promptly after additional manual care. The radiographs obtained at the 4-year follow-up in 2013 demonstrated improvement in cervical slippage at all levels (Fig. 1b). Following 13 years of chiropractic MC, cervical radiographs taken in 2022 revealed restoration of cervical alignment (Fig. 1c). The rate of missed appointment was less than 10%. Regarding the home exercise, an approximate rate of 45% patient adherence was achieved across the entire MC program based on patient self-monitoring. Additional effects of the succeeding home exercises might also potentially have a role to play in better rehabilitation outcomes of her neck complaints. No other pathological conditions or treatment-related adverse events were reported. For a summary timeline events, please see Figure 2.
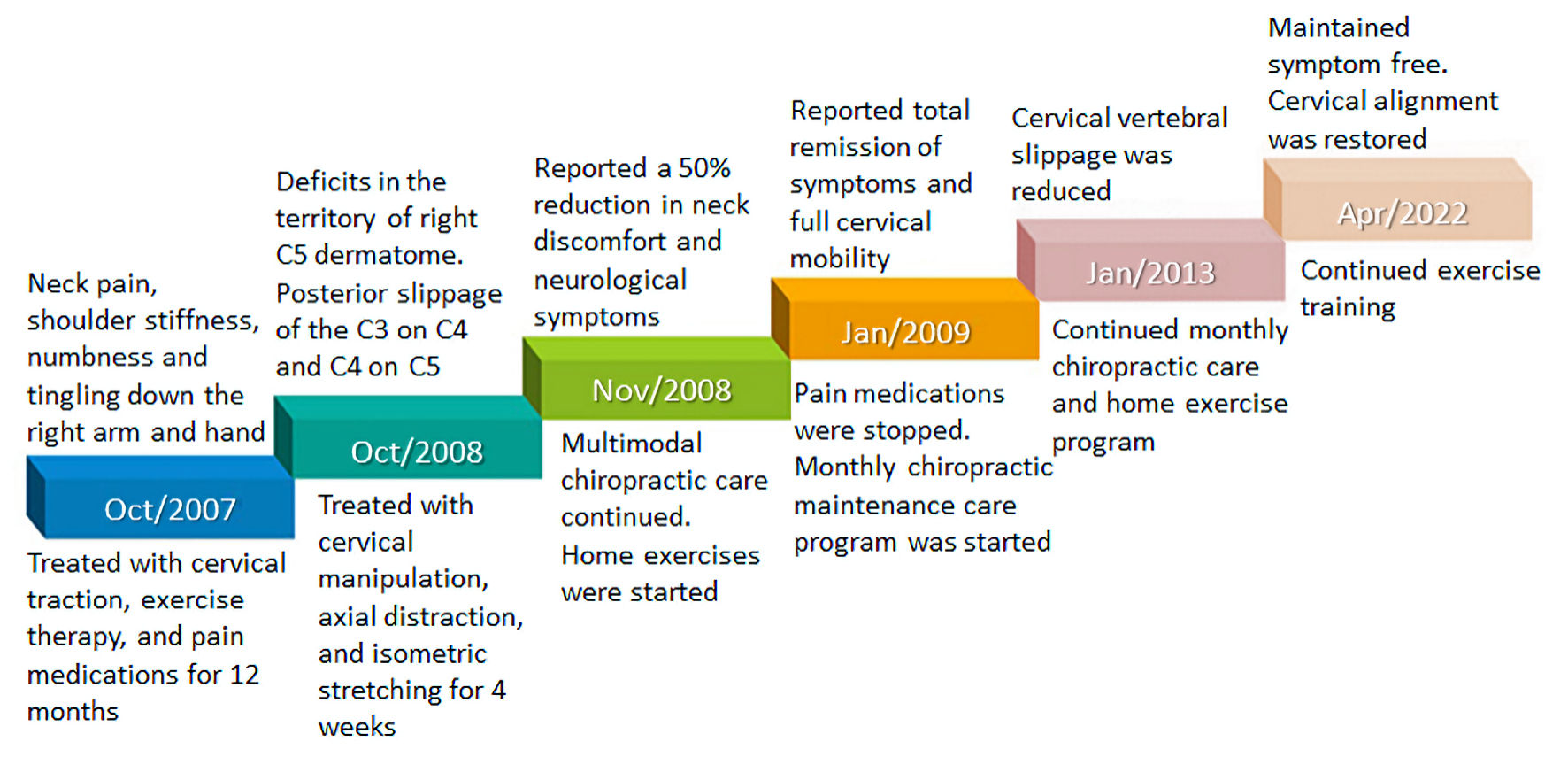 Click for large image | Figure 2. Clinical timeline of the presenting case. |
| Discussion | ▴Top |
Spondylolisthesis is derived from the Greek roots spondylos and listhesis, meaning slipped vertebra. Spondylolisthesis is defined as the slippage of ≥ 2 mm of the vertebra over the adjacent vertebra either forward (anterolisthesis) or backward (retrolisthesis) direction [1]. Of the two, anterolisthesis is more common in the lumbar spine, and retrolisthesis is more common in the cervical spine [13]. The direction of slippage is significantly related to stabilizing mechanisms, such as weakness of soft tissues, height of C2 - C7, global sagittal curvature, and working load [14]. The extent of slippage is graded on a scale from 1 to 4. Grade 1 is mild (less than 25% slippage), while grade 4 is severe (greater than 75% slippage). The main etiologies are disc degeneration and facet joint arthrosis [2]. Knowledge of the characteristic findings of neck pain on plain radiographs, such as disc height loss, endplate sclerosis, osteophyte formation, and misalignment, would be helpful for assessing the relationship between clinical symptoms and spinal kinematics. The symptoms can vary greatly and depend on the grade of slippage or the degree to which the adjacent tissues are affected by the spondylolisthesis.
Degenerative spondylolisthesis has been considered relatively rare in the cervical spine, in contrast to the lumbar spine [2]. Actually, degenerative cervical spondylolisthesis is more common than previously thought. In particular, the new overuse injury of modern life, known as “text neck syndrome”, distinctly increases the prevalence of cervical spondylolisthesis among smartphone users and office workers [4, 5]. Degenerative cervical spondylolisthesis is most common in C3/4 and C4/5 [1, 3], occurring in 46% (81 of 176) of patients at C3/4 and 49.4% (87 of 176) of patients at C4/5 [3]. The preference for spondylolisthesis in the middle cervical spine may be explained by the relative hypermobility and mobile patterns of the neck. It has been assumed that degeneration of the disc and the facet joints firstly occurs in association with instability and neck pain. The patient will generally have a guarded neck posture in order to relieve pressure off of the affected tissues. If instability proceeds faster than restoration, spondylolisthesis may become visible on radiographs at this early stage [2].
There is no guideline for the treatment of degenerative cervical spondylolisthesis. Surgical treatment for restoring a balanced spine is indicated in those with radiologically proven cervical spondylolisthesis complicated by instability and/or spinal cord compression [2, 3]. Patients with grade 1 or 2 spondylolisthesis and no accompanying quality-of-life impairments can be managed conservatively [15]. Non-surgical management of spondylolisthesis includes pain control, collar bracing, physiotherapy, and chiropractic treatment [15, 16]. Restoration of spinal stability using conservative approaches may prevent progression of the disease and various forms of deformity [4, 5]. In non-surgical management of low-grade spondylolisthesis, treatment efficacy more often relates to improvement of symptoms and not to repositioning of the slipped vertebra [16].
Emerging evidence has suggested that manipulative therapy is safe and beneficial for patients with degenerative cervical spondylolysis [6, 7, 16, 17]. Unstable (high-grade) spondylolisthesis should avoid forceful manipulation that might cause more stress to the spine. However, cautious manipulation is not contraindicated for a patient with low-grade spondylolisthesis without neurological deficits [17]. Regarding the present case, a multimodal intervention along with 13-year MC was implemented. The interventions were not aiming at adjusting slippage. High-velocity, low amplitude techniques employ rapid thrusts over restricted joints to restore a normal range of motion in the joint [18]. Axial cervical distraction is a traction-based therapy performed with a manual contact over the cervical region, producing rhythmic, localized distractive movement while patients are in the prone position [19]. Post-isometric cervical stretching involves bringing a muscle to a stretched position, then contracting the muscle without allowing it to move for three to five slow breaths. The stretching technique is used to improve flexibility of postural muscles [20]. Finally, exercises assigned to the home environment provide daily training for targeted muscle groups. The periodic MC program has accumulated mixed results, including resolution of symptoms and regression of retrolisthesis.
With regard to this case, the patient underwent monthly MC for 13 years. As her cervical alignment continued to improve during the maintenance period (Fig. 1), the MC prominently exhibited a potential effectiveness for this patient. A personalized MC can be viewed as a form of preventive visit after the initial treatment for recurrent or episodic pain and musculoskeletal dysfunction [9]. The prevention of further episodes (secondary prevention) and associated sequelae (tertiary prevention) is equally important [21]. The MC strategy required only a slightly higher number of chiropractor visits and should be considered an adjuvant treatment option for patients with recurrent or persistent spinal pain who respond well to the initial course of chiropractic care [9].
This study has potential limitations. First, as this was a retrospective single case study, it was not controlled. Second, spinal radiographs are often categorized as “standard of care” on an initial chiropractic evaluation. There was a lack of magnetic resonance imaging and electromyography for a complete investigation of soft tissue changes in cervical retrolisthesis. Radiological vertebral slippage is not always clinically symptomatic. Furthermore, the multimodal treatment approach could not clarify the exact role of chiropractic intervention. It has been assumed that patients with spinal pain do not always achieve full effectiveness from the initial manual treatment [9]. The continuing rehabilitation by means of strengthening home exercises might also contribute to improved clinical results of physical performance and function. Consequently, patient attendance at scheduled appointments [22] and adherence to assigned home exercises [23] might have affected the treatment outcomes in this case. The mechanisms of symptom relief and alignment retrieval warrant scrutiny. The strength of this study is that it provides evidence to show the subtle benefits of continuing MC.
Learning points
MC is a lengthy approach delivered in regularly spaced visits, whereby patients continue to maintain optimal body function after completing a prescribed course of manipulative therapy. The core elements of MC are disease monitoring, manual therapy, home exercise program, and general lifestyle coaching. It is assumed that patients do not always achieve full effectiveness from the initial phase of manipulative treatment. A maintenance program provides continuing chiropractic care, subsequent disease monitoring, and prolonged exercise rehabilitation to facilitate better clinical outcomes.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Informed consent was obtained from the patient for case publication.
Author Contributions
EC conceived the study, reviewed literature, and wrote the manuscript.
Data Availability
The author declares that data supporting the findings of this study are available within the article.
Abbreviations
MC: maintenance care; WHOQOL: World Health Organization Quality of Life
| References | ▴Top |
- Tao Y, Galbusera F, Niemeyer F, Samartzis D, Vogele D, Wilke HJ. Radiographic cervical spine degenerative findings: a study on a large population from age 18 to 97 years. Eur Spine J. 2021;30(2):431-443.
doi pubmed - Woiciechowsky C, Thomale UW, Kroppenstedt SN. Degenerative spondylolisthesis of the cervical spine—symptoms and surgical strategies depending on disease progress. Eur Spine J. 2004;13(8):680-684.
doi pubmed - Jiang SD, Jiang LS, Dai LY. Degenerative cervical spondylolisthesis: a systematic review. Int Orthop. 2011;35(6):869-875.
doi pubmed - Chu EC, Wong AY. Cervicogenic dizziness in an 11-year-old girl: a case report. Adolesc Health Med Ther. 2021;12:111-116.
doi pubmed - Chu EC. Preventing the progression of text neck in a young man: A case report. Radiol Case Rep. 2022;17(3):978-982.
doi pubmed - Liu Z, Qin X, Sun K, Yin H, Chen X, Yang B, Wang X, et al. Manipulation for degenerative lumbar spondylolisthesis: A systematic review of randomized controlled trials. J Trad Chin Med Sci. 2022;9(2):121-127.
doi - Wong LC. Rehabilitation of a patient with a rare multi-level isthmic spondylolisthesis: a case report. J Can Chiropr Assoc. 2004;48(2):142-151.
- Iben A, Lise H, Charlotte LY. Chiropractic maintenance care - what's new? A systematic review of the literature. Chiropr Man Therap. 2019;27:63.
doi pubmed - Eklund A, Hagberg J, Jensen I, Leboeuf-Yde C, Kongsted A, Lovgren P, Jonsson M, et al. The Nordic maintenance care program: maintenance care reduces the number of days with pain in acute episodes and increases the length of pain free periods for dysfunctional patients with recurrent and persistent low back pain - a secondary analysis of a pragmatic randomized controlled trial. Chiropr Man Therap. 2020;28(1):19.
doi pubmed - Myburgh C, Brandborg-Olsen D, Albert H, Hestbaek L. The Nordic maintenance care program: what is maintenance care? Interview based survey of Danish chiropractors. Chiropr Man Therap. 2013;21(1):27.
doi pubmed - Falla D, Lindstrom R, Rechter L, Boudreau S, Petzke F. Effectiveness of an 8-week exercise programme on pain and specificity of neck muscle activity in patients with chronic neck pain: a randomized controlled study. Eur J Pain. 2013;17(10):1517-1528.
doi pubmed - Fritz JM, Thackeray A, Brennan GP, Childs JD. Exercise only, exercise with mechanical traction, or exercise with over-door traction for patients with cervical radiculopathy, with or without consideration of status on a previously described subgrouping rule: a randomized clinical trial. J Orthop Sports Phys Ther. 2014;44(2):45-57.
doi pubmed - Park MS, Hwang JH, Kim TH, Oh JK, Chang HG, Kim HJ, Park KT, et al. Concurrent degenerative cervical and lumbar spondylolisthesis. J Korean Soc Spine Surg. 2018;25(4):154-159.
doi - Ninomiya K, Yamane J, Aoyama R, Suzuki S, Shiono Y, Takahashi Y, Fujita N, et al. Clinical effects of anterior cervical spondylolisthesis on cervical spondylotic myelopathy after posterior decompression surgery: a retrospective multicenter study of 732 cases. Global Spine J. 2022;12(5):820-828.
doi pubmed - Gagnet P, Kern K, Andrews K, Elgafy H, Ebraheim N. Spondylolysis and spondylolisthesis: A review of the literature. J Orthop. 2018;15(2):404-407.
doi pubmed - Fedorchuk CA, Lightstone DF, Oakley PA, Harrison DE. Correction of a double spondylolisthesis of the lumbar spine utilizing Chiropractic BioPhysics((R)) technique: a case report with 1 year follow-up. J Phys Ther Sci. 2021;33(1):89-93.
doi pubmed - Cassidy JD, Potter GE, Kirkaldy-Willis WH. Manipulative management of back pain in patients with spondyloisthesis. J Can Chirop Assoc. 1978;22(1):15-20.
- LaPelusa A, Bordoni B. High Velocity Low Amplitude Manipulation Techniques. In: StatPearls. Treasure Island (FL), 2022.
- Gudavalli MR, Salsbury SA, Vining RD, Long CR, Corber L, Patwardhan AG, Goertz CM. Development of an attention-touch control for manual cervical distraction: a pilot randomized clinical trial for patients with neck pain. Trials. 2015;16:259.
doi pubmed - Emary P. Use of post-isometric relaxation in the chiropractic management of a 55-year-old man with cervical radiculopathy. J Can Chiropr Assoc. 2012;56(1):9-17.
- Senna MK, Machaly SA. Does maintained spinal manipulation therapy for chronic nonspecific low back pain result in better long-term outcome? Spine (Phila Pa 1976). 2011;36(18):1427-1437.
doi pubmed - Alkomos MF, Mendez D, Mazzei-Pifano D, Shafeek F, Rodriguez C, Ali F, Banks C, et al. Patients' reasons for missing scheduled clinic appointments and their solutions at a major urban-based academic medical center. J Community Hosp Intern Med Perspect. 2020;10(5):426-430.
doi pubmed - Yalew ES, Melese AZ, Guadie YG, Gashaw M. Adherence to home-based exercise program and its predictors among patients treated in physiotherapy outpatient department in Amhara Region Hospitals in Ethiopia: A prospective cross-sectional study. Patient Prefer Adherence. 2022;16:561-572.
doi
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


