| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 13, Number 6, June 2022, pages 281-289
ST-Elevation Acute Myocardial Infarction in a Young Man
Daisuke Usudaa, c , Risa Tanakaa
, Makoto Suzukia
, Hayabusa Takanoa
, Yuta Hotchia
, Shintaro Shimozawaa
, Shungo Tokunagaa
, Ippei Osugia
, Risa Katoua
, Sakurako Itoa
, Kentaro Mishimaa
, Akihiko Kondoa
, Keiko Mizunoa
, Hiroki Takamia
, Takayuki Komatsua, b
, Jiro Obaa
, Tomohisa Nomuraa
, Manabu Sugitaa
aDepartment of Emergency and Critical Care Medicine, Juntendo University Nerima Hospital, 3-1-10, Takanodai, Nerima-ku, Tokyo 177-8521, Japan
bFaculty of Medicine, Juntendo University, 2-1-1, Hongo, Bunkyo-ku, Tokyo 113-8421, Japan
cCorresponding Author: Daisuke Usuda, Department of Emergency and Critical Care Medicine, Juntendo University Nerima Hospital, 3-1-10, Takanodai, Nerima-ku, Tokyo 177-8521, Japan
Manuscript submitted March 28, 2022, accepted May 6, 2022, published online June 2, 2022
Short title: AMI in a Young Man
doi: https://doi.org/10.14740/jmc3939
| Abstract | ▴Top |
Acute myocardial infarction (AMI) in young patients is very rare, but the incidence has increased over years past at younger ages, likely due to the presence of multiple risk factors. We present the first known case of ST-elevation AMI (STEMI) in a young man. A 22-year-old Japanese man was transferred to our hospital due to suddenly occurred anterior chest pain. An electrocardiogram revealed ST elevation in anteroseptal leads together with reciprocal ST depression in inferior leads. An emergency coronary angiogram was performed, revealing a 100% occlusion at segment 6 of the coronary artery and we established a diagnosis of STEMI. The lesion was expanded to 0% stenosis through plain old balloon angioplasty, after which a third-generation drug-eluting stent was installed there. Afterwards, the patient was discharged on day 17. In this case, a combination of mild six risk factors plus family history of hypertension might lead to this atypical event.
Keywords: ST-elevation acute myocardial infarction; Acute myocardial infarction; Male; Young; Risk factor
| Introduction | ▴Top |
Acute myocardial infarction (AMI) is the leading worldwide cause of cardiovascular events, and angina is commonly seen before AMI [1, 2]. AMI is extremely rare in young patients: in one study in Poland, individuals under age 40 represented only 1-6% of all AMI patients [2-5]. The rate of incidence has increased over years past in younger patients (< 35 years old) compared to older patients, and the age of onset is gradually falling, likely due to the following multiple risk factors such as smoking, obese, hypertension, diabetes, hyperlipidemia (higher level of low-density lipoprotein-cholesterol (LDL-C)), higher level of uric acid, history of coronary artery disease, family history of premature AMI, non-obstructive coronary artery disease (CAD), and genetic polymorphisms related to blood coagulation, fibrinogen, homocysteine, being present [3, 6-9]. Among previous reports, current age of onset was 19 years old [3, 6-9]. Age range between 19 and 29 years, and female sex were the only categories in which the number of patients with angiographically normal coronary arteries was higher than those with atherosclerotic CAD [3]. This could mean that patients with normal coronary anatomy may not be having an acute coronary syndrome (ACS) and could be presenting with symptoms due to other conditions, or out of fear that they may be experiencing an ACS [3].
Etiological factors among the younger population are less studied and in patients under age 35 who have AMI, the atherosclerotic burden is very low [2, 5, 9]. Of these, young ST-elevation AMI (STEMI) patients aged 18 - 35 were characterized as being male, obese, smokers, and having a family history of ischemic heart disease, though there is also a prevalence of cardiometabolic risk factors [10-12]. To date, there have been no reports of STEMI in a young man with no previous clinical history of angina nor hereditary disease; therefore, we report the first such case, together with a brief review of literature.
| Case Report | ▴Top |
Investigations
A 22-year-old Japanese man was transferred to our emergency department (ED) due to anterior chest pain. This symptom suddenly occurred at rest in the afternoon, and it was degree 10/10 (0: no pain, 10: worst pain imaginable), oppressive, persistent, and without cold sweat. He had never experienced this symptom, and it persisted at our ED for 50 min after the onset of symptoms. On the other hand, it was not accompanied by cold sweat, nor respiratory fluctuation. Furthermore, he had not caught a cold in the days before.
The patient’s medical history included an operation for a left inguinal hernia when he was 5 years old, essential hypertension, and grade 1 right hydronephrosis when he was 22 years old. He was given 80 mg of nifedipine and 4 mg of doxazosin mesylate for essential hypertension on a regular basis, and his blood pressure was well controlled.
The patient had no history of smoking nor drinking alcohol. No abnormal findings had been found on his regular medical exams. The patient worked part-time at a coffee shop, three times a week, and was allergic to dust and cedar pollen. He did not need any assistance for everyday life activities. His older brother, father, and grandfather all suffered from hypertension, and they took antihypertensive drugs. On the other hand, the patient had no family history of malignant disease. None of his family members had been diagnosed with familial hypercholesterolemia (FH).
The patient was 173 cm tall and weighed 77 kg (body mass index (BMI): 25.7). At our ED, his vital signs were normal other than hypertension, with blood pressure of 147/87 mm Hg, heart rate of 69 regular beats/min, body temperature of 36.5 °C, oxygen saturation of 100% in ambient air, and respiratory rate of 16/min; his Glasgow Coma Scale score was 15 points (E4V5M6). A 3 cm surgical scar was confirmed in the left inguinal region, but nothing else abnormal was detected upon physical examination, including skin and neurological findings.
Diagnosis
A routine laboratory examination, taken 60 min after the onset of symptoms, revealed increased values of alkaline phosphatase, urea nitrogen, creatinine, uric acid, C-reactive protein, LDL-C, plasma glucose, N-terminal prohormone of brain natriuretic peptide, high-sensitivity troponin T, and deceased values of potassium and high-density lipoprotein cholesterol (HDL-C). On the other hand, other values, including complete blood count and biochemistry, were normal (Table 1).
 Click to view | Table 1. Routine Emergency Department Laboratory Examination of the Patient |
An electrocardiogram (ECG) taken 60 min after the onset of symptoms revealed ST elevation in anteroseptal leads (V1-V4), together with reciprocal ST depression in inferior leads (II, III, and aVF), and these findings were new compared to a previous ECG at the time of medical checkup taken a month ago (Fig. 1a and b, respectively). A transthoracic echocardiography confirmed severe hypokinesis of anteroseptal motion, and the left ventricular ejection fraction (LVEF) was about 20-30%; however, other findings were normal. A plain computed tomography (CT) of the chest had normal results, with no evidence of a pulmonary embolism.
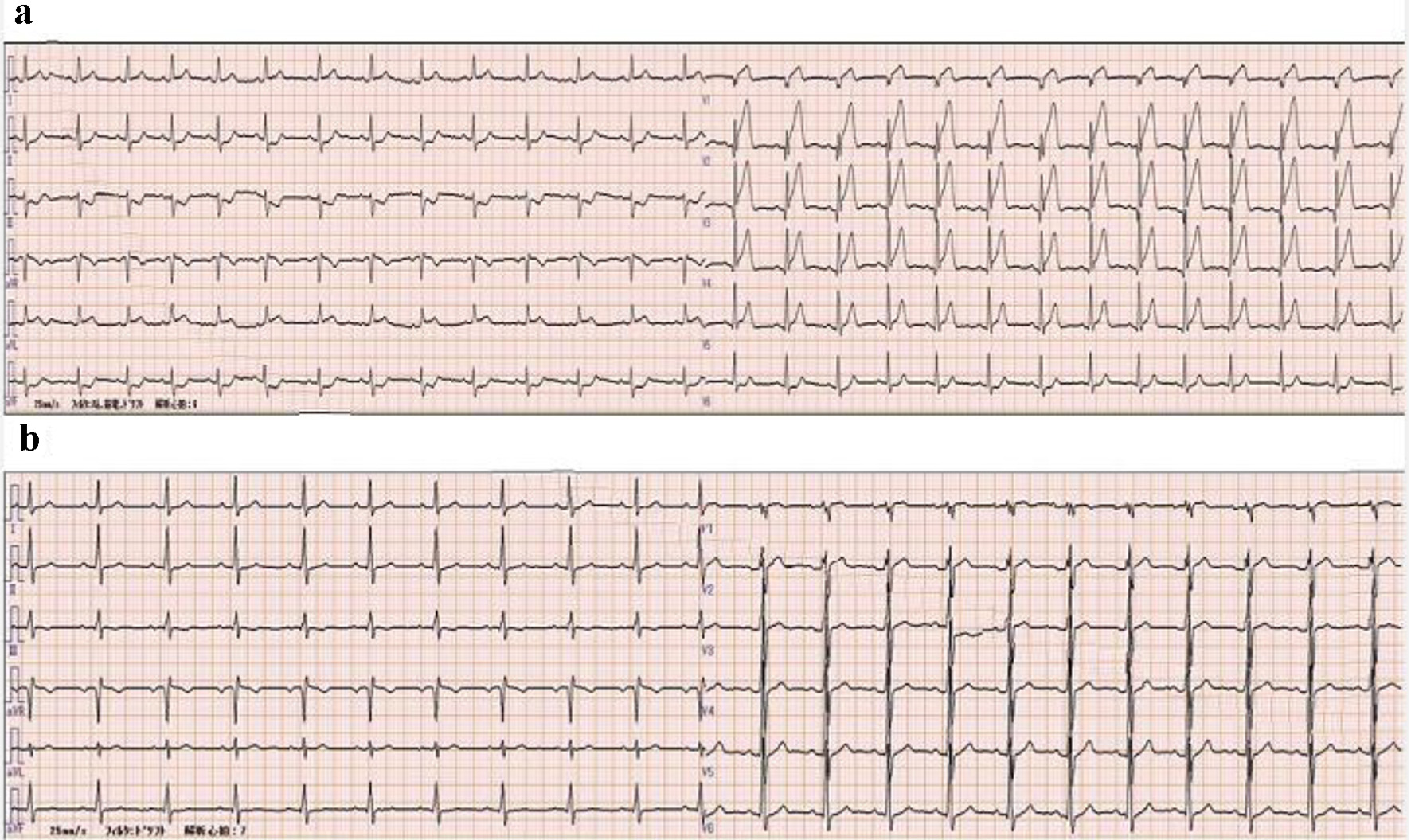 Click for large image | Figure 1. Electrocardiogram findings. (a) In emergency room. ST elevation in anteroseptal leads (V1-V4) is confirmed together with reciprocal ST depression in inferior leads (II, III, and aVF). (b) One month prior to admission. Normal findings. |
At this point, the patient was referred to cardiologists, with a suspected diagnosis of STEMI in the anteroseptal region. An emergency coronary angiogram (CAG) was carried out, using the left radial artery approach with a 6 French sheath, and it revealed an occlusion in the left anterior descending coronary artery (LAD): 100% occlusion at segment 6 (Fig. 2a). In addition, no abnormal findings, such as coronary artery aneurysm, were confirmed through the CAG. An intravascular ultrasound confirmed rich unstable plaque at the lesion. Raman spectroscopy revealed that the coronary plaque consisted of particularly lipid and calcium. On the other hand, the patient did not meet the criteria for FH. In addition, secondary hypertension was excluded by laboratory and imaging test including CT and magnetic resonance imaging.
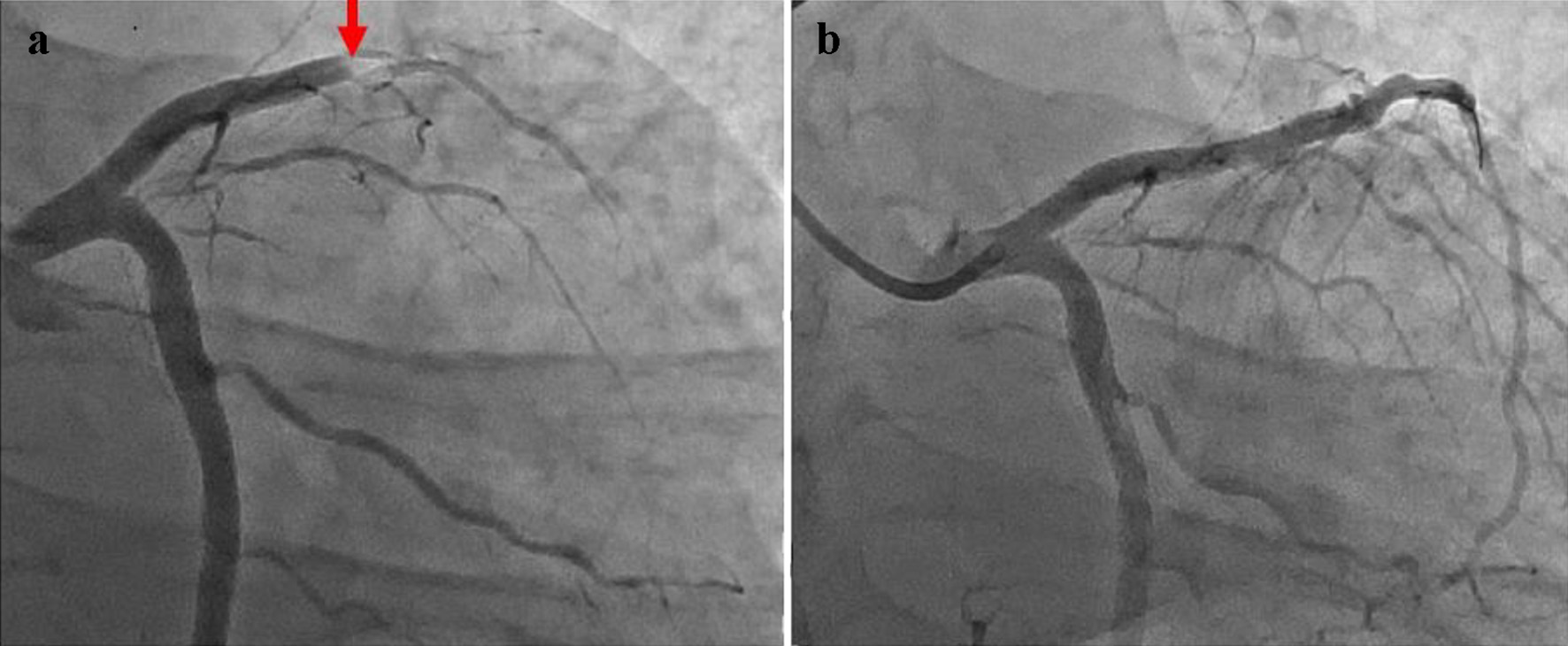 Click for large image | Figure 2. Coronary angiogram findings, caudal view. (a) Pre-PCI. A 100% occlusion at segment 6 is confirmed. (b) Post-PCI. Removal of the vascular obstruction together with recanalization, namely 0% stenosis is confirmed. PCI: percutaneous coronary intervention. |
We established a diagnosis of STEMI in the anteroseptal region (100% occlusion at segment 6).
Treatment
The lesion was expanded to 0% stenosis through plain old balloon angioplasty (Fig. 2b), after which a third-generation drug-eluting stent (the Ultimaster® 3.5 mm diameter/24 mm length sirolimus eluting coronary stent) was installed there. The duration from arrival at our ED to coronary artery recanalization, or “door to balloon time”, was 2 h, and the duration from the onset of symptoms to coronary artery recanalization was 2 h and 50 min. The patient was stable after percutaneous coronary intervention (PCI), and started a routine of 100 mg of aspirin, 75 mg of clopidogrel, 40 mg of telmisartan, 2.5 mg of bisoprolol fumarate, 4 mg of pitavastatin calcium, and 10 mg of ezetimibe, 1 day after PCI.
Follow-up and outcomes
The maximum value of creatine kinase was 5,815 U/L, at 4 h and 30 min after PCI, and it gradually decreased after that point. The patient was discharged from the intensive care unit on the third hospital day without post ventricular arrhythmia or heart failure, and was stable afterward during his hospitalization. He was discharged on day 17. Afterwards, we confirmed that his post-PCI progress was satisfactory 14 days later. At that time, we performed ECG and it did not reveal atrial fibrillation. Therefore, paroxysmal atrial fibrillation that may cause coronary embolic obstruction might have been ruled out. The clinical course of the patient is shown in Figure 3.
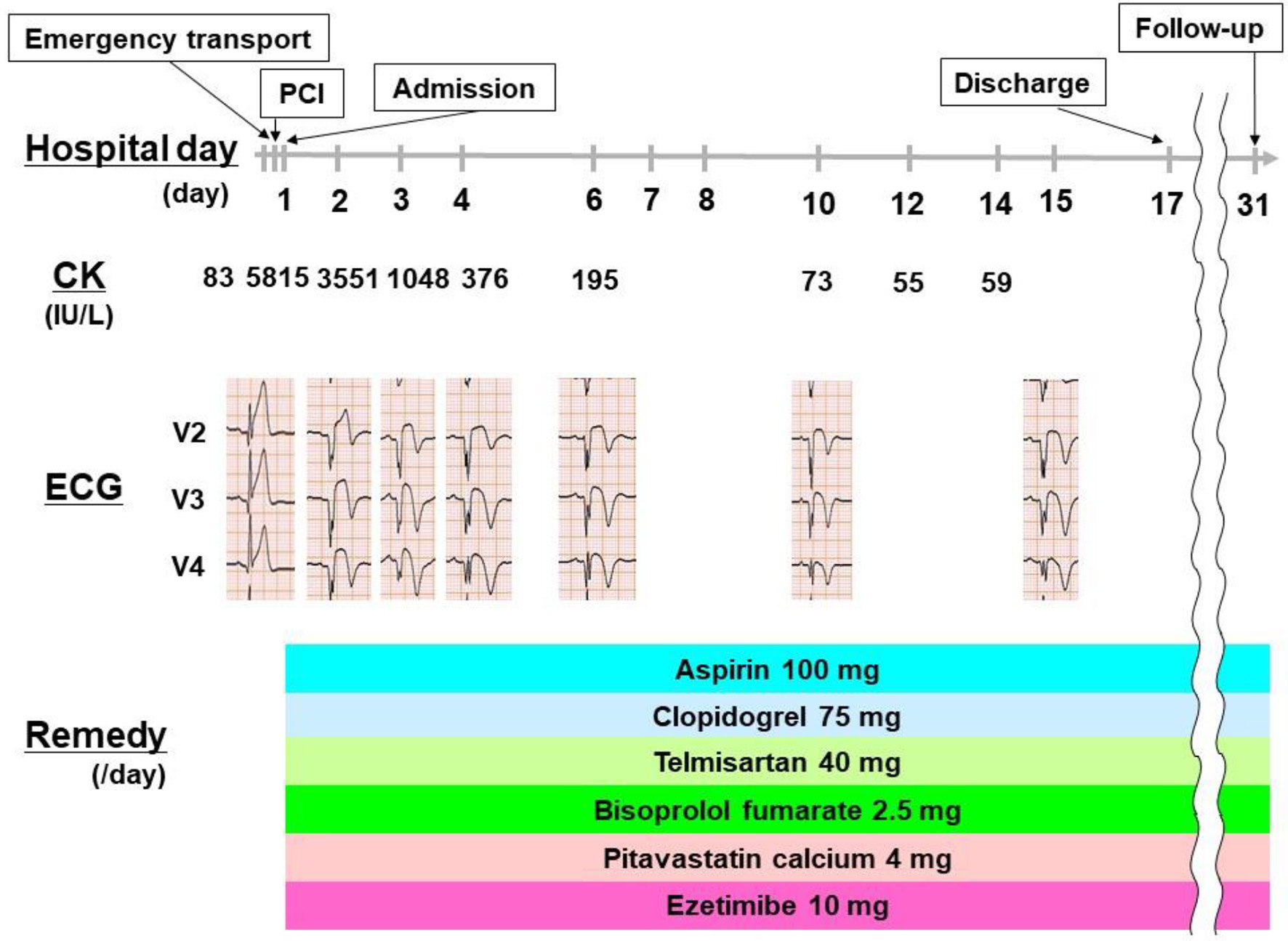 Click for large image | Figure 3. Clinical course of the patient. The patient was transported to our hospital and diagnosed as STEMI, afterwards he was performed PCI and admitted on day 1. Afterwards, he was stable during his hospitalization. He was discharged on day 17 and we confirmed that his post-PCI progress was satisfactory on day 31. PCI: percutaneous coronary intervention; CK: creatine kinase; ECG: electrocardiogram. |
| Discussion | ▴Top |
We present the first known case of STEMI in a young man with no previous clinical history of angina, who did not have hereditary disease. The most important discussion point is why this 22-year-old man with well-controlled hypertension had an STEMI. STEMI cases in young population are very rare and the patients were all female [13, 14]. Furthermore, this patient suffered from neither hereditary diseases, including FH, nor cardiovascular diseases, including previous anginal attack or Kawasaki diseases. In this case, suspected STEMI risk factors include obesity, hypertension, renal dysfunction, hyperuricemia, dyslipidemia, and abnormal glucose tolerance. In addition, he had a family history of hypertension and it also may be a risk factor of STEMI. We cannot declare mention clear reason why he had STEMI, but suspected reason is as follows. Though these were all mild, a combination of these six risk factors plus family history of hypertension might lead to this type of event. On the other hand, thrombogenesity examination using routine blood sample before heparinization was normal, therefore it could not lead to this atypical event. We suspect it is unique among young age and there is value in reporting this event.
Among these risk factors, patients with FH have a tendency to develop AMI at earlier ages, and patients with FH have double risk of cardiovascular events compared to non-FH patients, even for patients undergoing high-intensity lipid-lowering therapy [15, 16]. High LDL-C levels since birth are known to have a correlation with early atherosclerotic disease onset [15]. Approximately one subject in 250 carries a genetic mutation that determines FH; there should be more representation of FH among subjects who have a documented CAD diagnosis [15]. Therefore, identifying these subjects earlier could lead to improved management of their high cardiovascular risk, and identify possible FH relatives through cascade screening [15]. On the other hand, despite broad warnings and public information campaigns, smoking is still the most common modifiable risk factor in young adult STEMI patients [17, 18]. A significant decrease was seen in age-standardized AMI hospitalizations after a smoking ban was introduced, in a long-term follow-up in both younger and older patients, both male and female, though with differences regarding place of residence [19]. In addition, young patients have a low proportion of hypertension and diabetes, but these patients have high levels of LDL-C, uric acid, and homocysteine [12]. There was a 3-4‰ postnatal risk of Kawasaki disease, increasing with every birth year; patients with the disease face a significant risk of major cardiac events during childhood, such as AMI [20]. There was more frequent recurrence in younger patients, with a 1.9% probability of a major cardiac event (infarction, undergoing PCI or coronary artery bypass grafting, or death) by the time patients reach adolescence [20]. In addition, in younger women, spontaneous coronary artery dissection (SCAD) has come to be increasingly recognized as a cause of myocardial infarction (MI), but treatment is often conservative because of revascularization risks [21, 22]. STEMI-SCAD is an important subset of STEMI, particularly among younger women, and generally brings a significantly higher frequency of left main or LAD culprit and cardiogenic shock compared to STEMI atherosclerosis [22]. Long-term exposure to air pollution and traffic noise has also been variably associated with the incidence of acute vascular events, including AMI [23]. Notably, in this case, emergency service workers did not suspect AMI, despite the symptoms, due to the young age of the patient. In consideration of this, clinicians should include AMI as a differential diagnosis when they see patients suffering from chest pain, regardless of risk factors and age.
Similarly, even when traditional risk factors are not present, it is crucial to test aggressively for procoagulant markers in young patients who present with chest pain at high altitudes [24]. Introducing various highly sensitive cardiac troponin assays, as a part of clinical practice, has provided a new tool to help clinicians diagnose AMI [25]. In addition, compared to older age groups, young ACS patients had higher rates of STEMI, less extensive CAD, and more favorable prognoses [26, 27]. However, implementing sex-specific cutoffs for ACS diagnosis and management still has unclear clinical utility [25]. On the other hand, a study from China of young STEMI patients (< 35 years old) found that coronary artery stenosis was common, with stenosis more likely to occur in the LAD branch [12]. In another report on young MI (< 35 years old), patients were found to have increased whole blood viscosity compared to the healthy control group [28]. When comparing the ECG characteristics of men versus women (≤ 55 years old) with AMI, it was found that women did not have a different frequency of sinus rhythm from men, but that women did have shorter PR and QRS intervals and longer QTc intervals [29]. There was no difference between genders in intraventricular conduction disturbances [29]. Women showed a greater tendency to have abnormal anterior lead Q waves, and lower Q wave frequency in other territories, compared to men [29]. Among STEMI patients, women had lesser magnitude and extent of ST-segment elevation than men, causing STEMI diagnosis to be less common in women than in men [29]. In summary, significant differences were found among young patients by gender in ECG presentations of AMI [29].
The readmission risk trends with age vary by specific cause [30]. Age-targeted initiatives are therefore warranted in order to reduce the incidence of preventable readmissions in AMI patients who are undergoing PCI [30]. While younger patients (18 - 54 years old) had the lowest readmission rate (7.27%), younger patients had a greater risk of readmission than patients aged 55 - 64, both for all causes and for specific causes, such as AMI or chest pain (both cardiac and non-specific) [30, 31]. Among young patients with AMI, the likelihood of readmission was higher for women and for patients who had a prior AMI, increased depressive symptoms, longer inpatient length of stay, or diabetes [31]. Patients aged 65 - 74 had a lower risk of readmission for all causes [30]. Older patients (≥ 75 years old) had a lower risk of readmission for chest pain, but a greater risk of readmission caused by heart failure or infection [30]. On the other hand, notably, in young AMI patients, several readmission predictors were psychosocial characteristics, rather than AMI severity markers [31].
The clinical outcomes of patients with plaque erosion may be affected by the distinct variance, by age, in demographic, clinical, angiographic, and plaque phenotypes [24]. Worldwide cardiovascular disease mortality is increasing, and onset age is gradually dropping [9]. STEMI is associated with significant mortality, which leads to a loss of productive years of life, particularly in younger patients [11]. In younger patients with STEMI, the mortality rate is lower, but not negligible [11]. Young patients also experience higher rates of cardiogenic shock, out-of-hospital cardiac arrest, and STEMI [27]. The risk factors associated with worse outcomes need to be investigated as soon as possible [26]. Shock, contrast-induced nephropathy, HF with Killip class 2, and decreased LVEF served as particularly potent predictors of both adverse outcomes and long-term mortality [26]. STEMI patients were found to have larger infarct sizes, correlating to higher peak high-sensitivity cardiac troponin I, and to have worse Killip scores [26]. Unsurprisingly, patients who had normal coronary angiography were found to have better prognoses than those with stenosis [12]. Furthermore, a high BMI value was found to be an independent predictor of all-cause AMI mortality in the younger age group [32]. For these reasons, public health efforts are necessary, with the goal of reducing prevalence of these risk factors among the segments of the population that are constitutionally susceptible [11]. Short-term mortality outcomes favored younger women over older women, though in-hospital management was similar for both groups [33]. Compared to younger men, younger women (≤ 65 years old) with STEMI were less likely to receive guideline-recommended pharmacotherapy and revascularization during hospitalization, and these younger women also had greater 1-year and in-hospital mortality rates [10, 13, 29, 34-37]. Among adults with AMI, there was a higher risk of in-hospital mortality for younger adults with BMIs of 35.0 - 39.9 or ≥ 40, compared to non-obese patients [38]. Existing work suggests that the differences in outcome are likely multifactorial in cause, but they may be at least partially explained by factors such as atypical presentation, delayed presentation, under-recognition of STEMI at initial medical contact, and underuse of medications due to concern regarding increased bleeding risk [34]. A stepwise increase was seen in long-term mortality from young to middle-age and older; compared to older age groups, young patients (< 45 years old) with STEMI have a more favorable prognosis [5, 8, 26, 27, 39-40]. More specifically, patients aged ≥ 65 have an in-hospital mortality that is three times higher [39]. There has been a more pronounced and persistent decline in emergent condition ED visits among older adults compared to younger patients, with fewer ED deaths [27]. This is cause for concern, given that this age group faces a greater prevalence and risk of poor outcomes for emergent conditions that are amenable to time-sensitive ED diagnosis and treatment; this may explain, in part, the excess mortality seen among older adults during the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) era [27]. It is additionally clear that there is great potential for improvements to AMI care without serious sequelae among the younger patient age group [5, 39].
One important strategy for preventing CAD in the younger population is preventing or treating modifiable risk factors to reduce cardiovascular risk, such as smoking cessation, and aggressive lipid and weight control [9, 26, 33]. For smoking in particular, it is very important to better understand the harms of smoking, and there is a need to enhance tobacco control education and guidance for quitting smoking, targeting young women [17]. Additionally, studies in many countries have documented correlations between reduced AMI hospitalizations and anti-smoking policies [41]. Specifically, cigarette tax policy and anti-smoking laws were associated with reductions in young adult hospitalizations for AMI [41]. To ensure the effectiveness of these policies, anti-smoking laws need to be strictly enforced, and tobacco taxes need to be high enough to increase cigarette prices above and beyond the rate of inflation, to discourage cigarette purchases [41]. On the other hand, particularly among the youngest age group, AMI survivors remain a high-risk group, reinforcing the need for both primary and secondary prevention, including effective patient education, to help improve long-term AMI patient prognoses [5, 40].
When comparing STEMI and non-STEMI (NSTEMI) among younger patients, the young STEMI group had, as its most prominent young-population risk factors: male sex, smoking, dyslipidemia with lower HDL-C level and hypertriglyceridemia, obesity, and a positive family history [26, 27]. On the other hand, in young adults, particularly the NSTEMI group, diabetes mellitus and hypertension remain potent CAD contributors [26]. In addition, across the whole group, and in both the STEMI and NSTEMI patient subgroups, no correlation was found between LVEF and protein carbonyl [42]. Both the STEMI and NSTEMI groups had significantly higher plasma-soluble extracellular matrix metalloproteinase inducer levels, compared to both the stable CAD and healthy control groups [43]. Furthermore, another study confirmed a hemorheological pattern impairment in young MI patients, which was partially influenced by infarction type (STEMI or NSTEMI); whole blood viscosity was higher in STEMI patients than NSTEMI patients, and persisted for long term [28]. In NSTEMI patients, the frequency, magnitude, and extent of ST-segment depression were consistent across genders, but women were less likely to have anterior ST-segment depression and more likely to have anterior negative T waves than men [29]. Prognoses were worse for younger patients presenting with STEMI than for those presenting with NSTEMI [27]. In addition, younger-age hospitalization was reported to have no differences by gender between STEMI; on the other hand, the similar result was not reported between NSTEMI [44]. There was also no long-term mortality difference between STEMI and NSTEMI, though short-term mortality and morbidity were greater in STEMI than NSTEMI patients [26, 27].
This case study has a limitation: it only reviews a single case report and case series of STEMI in young person with no previous clinical history of angina nor hereditary disease. Therefore, the actual situation and nature of the disease may differ from the results of the literature review, as a result of reporting bias. Additional studies are needed to further evaluate the impact of gender on clinical presentation, treatment patterns, and outcomes of AMI in young patients. In addition, to better understand this rare case, a biopsy of the occlusion would help; however, it was not performed. The measured level of LDL-C was relatively high for his age and we should have ruled out sitostorolemia.
In conclusion, we present the first case of STEMI in a young man with no previous clinical history of angina nor hereditary disease. Like our case, STEMI could occur in a young man who has risk factors.
Learning points
Physicians should control all coronary risk factors favorably, even if in a young case. In addition, this case also suggests the need for urgent and careful examinations when encountering patients presenting with chest pain, in order not to miss diseases for which immediate diagnosis and treatment would be necessary.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Author Contributions
DU wrote the manuscript. RT, MS, HT, YH, SS, ST, IO, RK, SI, KM, AK, KM, HT, TK, JO, TN, and MS proofread and revised the manuscript. All authors approved the final version to be published.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
Abbreviations
AMI: acute myocardial infarction; LDL-C: low-density lipoprotein cholesterol; CAD: coronary artery disease; ACS: acute coronary syndrome; STEMI: ST-elevation acute myocardial infarction; ED: emergency department; BMI: body mass index; FH: familial hypercholesterolemia; HDL-C: high-density lipoprotein cholesterol; ECG: electrocardiogram; LVEF: left ventricular ejection fraction; CT: computed tomography; CAG: coronary angiogram; LAD: left anterior descending; PCI: percutaneous coronary intervention; SCAD: spontaneous coronary artery dissection; MI: myocardial infarction; NSTEMI: non-ST-elevation acute myocardial infarction
| References | ▴Top |
- Grodzinsky A, Arnold SV, Gosch K, Spertus JA, Foody JM, Beltrame J, Maddox TM, et al. Angina frequency after acute myocardial infarction in patients without obstructive coronary artery disease. Eur Heart J Qual Care Clin Outcomes. 2015;1(2):92-99.
doi pubmed - Mansour H, Rayan M, Shnoda M, Kamal D. Cannabis and tramadol addiction: Do they imply additive risk for acute myocardial infarction in adults younger than 45 years? Anatol J Cardiol. 2020;24(5):316-325.
doi pubmed - Jamil S, Jamil G, Mesameh H, Qureshi A, AlKaabi J, Sharma C, Aziz F, et al. Risk factor comparison in young patients presenting with acute coronary syndrome with atherosclerotic coronary artery disease vs. angiographically normal coronaries. Int J Med Sci. 2021;18(15):3526-3532.
doi pubmed - Trzeciak P, Gierlotka M, Polonski L, Gasior M. Treatment and outcomes of patients under 40 years of age with acute myocardial infarction in Poland in 2009-2013: an analysis from the PLACS registry. Pol Arch Intern Med. 2017;127(10):666-673.
doi pubmed - Wittlinger T, Seifert C, Simonis G, Gerlach M, Strasser RH. Prognosis in myocardial infarction of young patients: Results of a prospective registry. Int J Cardiol. 2020;300:1-6.
doi pubmed - Nazzal C, Lefian A, Alonso F. [Incidence of acute myocardial infarction in Chile between 2008 and 2016]. Rev Med Chil. 2021;149(3):323-329.
doi pubmed - Marroush TS, Sharma AV, Botros B, Szpunar S, Rosman HS, Mehta RH. Differences in baseline characteristics and outcomes in young Caucasians and African Americans with acute myocardial infarction. Am J Med Sci. 2021;361(2):238-243.
doi pubmed - Jortveit J, Pripp AH, Langorgen J, Halvorsen S. Incidence, risk factors and outcome of young patients with myocardial infarction. Heart. 2020;106(18):1420-1426.
doi pubmed - Liu X, Luo Y. Progress in the studies on the risk factors of acute myocardial infarction in patients under 35 years old. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2020;45(7):856-861.
- Alkhouli M, Alqahtani F, Jneid H, Al Hajji M, Boubas W, Lerman A. Age-stratified sex-related differences in the incidence, management, and outcomes of acute myocardial infarction. Mayo Clin Proc. 2021;96(2):332-341.
doi pubmed - Tung BW, Ng ZY, Kristanto W, Saw KW, Chan SP, Sia W, Chan KH, et al. Characteristics and outcomes of young patients with ST segment elevation myocardial infarction undergoing primary percutaneous coronary intervention: retrospective analysis in a multiethnic Asian population. Open Heart. 2021;8(1):e001437.
doi pubmed - Li XR, Zuo HJ, Yang HX, Zhang DF, Ma Z, An ZY, Song XT. [Clinical characteristics and prognosis of young (<35 years) patients with acute ST-segment elevation myocardial infarction]. Zhonghua Xin Xue Guan Bing Za Zhi. 2021;49(11):1124-1129.
- Lu Y, Zhou S, Dreyer RP, Spatz ES, Geda M, Lorenze NP, D'Onofrio G, et al. Sex differences in inflammatory markers and health status among young adults with acute myocardial infarction: results from the VIRGO (variation in recovery: role of gender on outcomes of young acute myocardial infarction patients) study. Circ Cardiovasc Qual Outcomes. 2017;10(2):e003470.
doi - Kawaguchi S, Hasebe T, Ohta H, Kikuchi A, Asanome A, Nishiura T, Sakamoto N, et al. Acute Myocardial Infarction in a 17-year-old High-school Girl. Intern Med. 2021;60(2):259-263.
doi pubmed - Gulizia MM, Maggioni AP, Abrignani MG, Bilato C, Mangiacapra F, Sanchez FA, Piovaccari G, et al. Prevalence Of familial hypercholeSTerolaemia (FH) in Italian Patients with coronary artERy disease: The POSTER study. Atherosclerosis. 2020;308:32-38.
doi pubmed - Danchin N, Farnier M, Zeller M, Puymirat E, Cottin Y, Belle L, Lemesle G, et al. Long-term outcomes after acute myocardial infarction in patients with familial hypercholesterolemia: The French registry of Acute ST-elevation and non-ST-elevation Myocardial Infarction program. J Clin Lipidol. 2020;14(3):352-360.e356.
doi pubmed - Hu GL, Liu J, Liu J, Hao YC, Yang N, Zhou MG, Zeng YY, et al. [Association between smoking and the severity of coronary lesions among young and middle-aged female patients with acute coronary syndrome]. Zhonghua Xin Xue Guan Bing Za Zhi. 2020;48(5):378-385.
- Gleerup HB, Dahm CC, Thim T, Jensen SE, Jensen LO, Kristensen SD, Botker HE, et al. Smoking is the dominating modifiable risk factor in younger patients with STEMI. Eur Heart J Acute Cardiovasc Care. 2020;9(1):70-75.
doi pubmed - Ozieranski K, Witkowska A, Wojtyniak B, Gierlotka M, Zdrojewski T, Stokwiszewski J, Gasior M, et al. Smoking ban in public places and myocardial infarction hospitalizations in a European country with high cardiovascular risk: insights from the Polish nationwide AMI-PL database. Pol Arch Intern Med. 2019;129(6):386-391.
doi pubmed - Wu MH, Lin MT, Chen HC, Kao FY, Huang SK. Postnatal risk of acquiring Kawasaki disease: a nationwide birth cohort database study. J Pediatr. 2017;180:80-86.e82.
doi pubmed - Cheung CC, Starovoytov A, Parsa A, Andrade JG, Krahn AD, Bennett M, Saw J. In-hospital and long-term outcomes among patients with spontaneous coronary artery dissection presenting with ventricular tachycardia/fibrillation. Heart Rhythm. 2020;17(11):1864-1869.
doi pubmed - Lobo AS, Cantu SM, Sharkey SW, Grey EZ, Storey K, Witt D, Benson G, et al. Revascularization in patients with spontaneous coronary artery dissection and ST-segment elevation myocardial infarction. J Am Coll Cardiol. 2019;74(10):1290-1300.
doi pubmed - Magnoni P, Murtas R, Russo AG. Residential exposure to traffic-borne pollution as a risk factor for acute cardiocerebrovascular events: a population-based retrospective cohort study in a highly urbanized area. Int J Epidemiol. 2021;50(4):1160-1171.
doi pubmed - Yogesh Kumar YS, Sud S, Bhardwaj S, Pareek TK. Acute coronary syndrome in young males after a prolonged stay at high altitude. Med J Armed Forces India. 2021;77(4):490-493.
doi pubmed - Bhatia PM, Daniels LB. Highly sensitive cardiac troponins: the evidence behind sex-specific cutoffs. J Am Heart Assoc. 2020;9(10):e015272.
doi pubmed - Yilmaz S, Cosansu K. Prognostic factors and outcomes in young patients with presented of different types acute coronary syndrome. Angiology. 2020;71(10):894-902.
doi pubmed - Noaman S, Dinh D, Reid CM, Brennan AL, Clark D, Shaw J, Freeman M, et al. Comparison of outcomes of coronary artery disease treated by percutaneous coronary intervention in 3 different age groups (<45, 46-65, and >65 years). Am J Cardiol. 2021;152:19-26.
doi pubmed - Caimi G, Hopps E, Montana M, Andolina G, Urso C, Canino B, Lo Presti R. Analysis of the blood viscosity behavior in the Sicilian study on juvenile myocardial infarction. Clin Appl Thromb Hemost. 2018;24(8):1276-1281.
doi pubmed - Barrabes JA, Gupta A, Porta-Sanchez A, Strait KM, Acosta-Velez JG, D'Onofrio G, Lidon RM, et al. Comparison of electrocardiographic characteristics in men versus women </= 55 years with acute myocardial infarction (a variation in recovery: role of gender on outcomes of young acute myocardial infarction patients substudy). Am J Cardiol. 2017;120(10):1727-1733.
doi pubmed - Qin Y, Wei X, Han H, Wen Y, Gu K, Ruan Y, Lucas CH, et al. Association between age and readmission after percutaneous coronary intervention for acute myocardial infarction. Heart. 2020;106(20):1595-1603.
doi pubmed - Dreyer RP, Raparelli V, Tsang SW, D'Onofrio G, Lorenze N, Xie CF, Geda M, et al. Development and validation of a risk prediction model for 1-year readmission among young adults hospitalized for acute myocardial infarction. J Am Heart Assoc. 2021;10(18):e021047.
doi pubmed - Fukuoka S, Kurita T, Dohi K, Masuda J, Seko T, Tanigawa T, Saito Y, et al. Untangling the obesity paradox in patients with acute myocardial infarction after primary percutaneous coronary intervention (detail analysis by age). Int J Cardiol. 2019;289:12-18.
doi pubmed - Venkatason P, Zubairi YZ, Zaharan NL, Wan Ahmad WA, Hafidz MI, Ismail MD, Hadi MF, et al. Characteristics and short-term outcomes of young women with acute myocardial infarction in Malaysia: a retrospective analysis from the Malaysian National Cardiovascular Database registry. BMJ Open. 2019;9(11):e030159.
doi pubmed - Bugiardini R, Manfrini O, Cenko E. Female sex as a biological variable: A review on younger patients with acute coronary syndrome. Trends Cardiovasc Med. 2019;29(1):50-55.
doi pubmed - Zhang Z, Fang J, Gillespie C, Wang G, Hong Y, Yoon PW. Age-specific gender differences in in-hospital mortality by type of acute myocardial infarction. Am J Cardiol. 2012;109(8):1097-1103.
doi pubmed - Liu J, Elbadawi A, Elgendy IY, Megaly M, Ogunbayo GO, Krittanawong C, Tamis-Holland JE, et al. Age-stratified sex disparities in care and outcomes in patients with ST-elevation myocardial infarction. Am J Med. 2020;133(11):1293-1301.e1291.
doi pubmed - Shehab A, Bhagavathula AS, Alhabib KF, Ullah A, Suwaidi JA, Almahmeed W, AlFaleh H, et al. Age-related sex differences in clinical presentation, management, and outcomes in ST-segment-elevation myocardial infarction: pooled analysis of 15 532 patients from 7 Arabian Gulf Registries. J Am Heart Assoc. 2020;9(4):e013880.
doi pubmed - Sreenivasan J, Khan MS, Sharedalal P, Hooda U, Fudim M, Demmer RT, Yuzefpolskaya M, et al. Obesity and outcomes following cardiogenic shock requiring acute mechanical circulatory support. Circ Heart Fail. 2021;14(3):e007937.
doi pubmed - Caruntu F, Bordejevic DA, Tomescu MC, Citu IM. Clinical characteristics and outcomes in acute myocardial infarction patients aged >/=65 years in Western Romania. Rev Cardiovasc Med. 2021;22(3):911-918.
doi pubmed - Radisauskas R, Kirvaitiene J, Bernotiene G, Virviciute D, Ustinaviciene R, Tamosiunas A. Long-term survival after acute myocardial infarction in Lithuania during Transitional Period (1996-2015): data from population-based Kaunas ischemic heart disease register. Medicina (Kaunas). 2019;55(7):357.
doi pubmed - Patanavanich R, Glantz SA. Association between tobacco control policies and hospital admissions for acute myocardial infarction in Thailand, 2006-2017: A time series analysis. PLoS One. 2020;15(12):e0242570.
doi pubmed - Caimi G, Canino B, Incalcaterra E, Ferrera E, Montana M, Lo Presti R. Behaviour of protein carbonyl groups in juvenile myocardial infarction. Clin Hemorheol Microcirc. 2013;53(4):297-302.
doi pubmed - Akkus MN, Ormam A, Seyis S, Baran C, Gorur A, Bilen MN. Plasma EMMPRIN levels in acute myocardial infarction and stable coronary artery disease. Clin Invest Med. 2016;39(3):E79-87.
doi pubmed - Klugar M, Huncovsky M, Pokorna A, Dolanova D, Benesova K, Jarkovsky J, Muzik J, et al. Epidemiological analyses for preparation of Clinical Practice Guidelines related to acute coronary syndromes in the Czech Republic. Int J Evid Based Healthc. 2019;17(Suppl 1):S43-S47.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


