| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 12, Number 8, August 2021, pages 328-331
Ogilvie Syndrome and COVID-19 Infection
Jing Wanga, c, Georgiana Maruscaa, Tooba Tariqb, Bashar Mohamadb
aDepartment of Internal Medicine, Detroit Medical Center/Wayne State University, Detroit, MI 48201, USA
bDepartment of Gastroenterology, Detroit Medical Center/Wayne State University, Detroit, MI 48201, USA
cCorresponding Author: Jing Wang, Department of Internal Medicine, Detroit Medical Center/Wayne State University, 4201 St. Antoine, Ste. 2E, Detroit, MI 48201, USA
Manuscript submitted May 28, 2021, accepted June 15, 2021, published online July 3, 2021
Short title: Ogilvie Syndrome and COVID-19
doi: https://doi.org/10.14740/jmc3728
| Abstract | ▴Top |
Coronavirus disease 2019 (COVID-19) is an airborne infection transmitted via respiratory droplets and aerosolized material; however, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) uses the same angiotensin-converting enzyme type 2 receptor present in the respiratory epithelial cells to bind surface epithelial cells in the gastrointestinal tract. Here we report a case of Ogilvie syndrome in a patient who tested positive for SARS-CoV-2 a month prior to hospital admission. Quick recognition of Ogilvie syndrome as a potential complication of COVID-19 infection, prompt treatment with conservative measures, and prevention of possible fecal-oral transmission of the virus are crucial steps.
Keywords: Ogilvie syndrome; COVID-19; SARS-CoV-2; Fecal-oral transmission
| Introduction | ▴Top |
Coronavirus disease 2019 (COVID-19) is a viral infection with airborne transmission [1]. Common respiratory symptoms include fever, fatigue, and dry cough. However, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) uses the same angiotensin-converting enzyme type 2 (ACE-2) receptor present in the respiratory epithelial cells to bind epithelial cells in the stomach, small intestine and colon [2]. Up to 26% of patients present with gastrointestinal (GI) symptoms [1]. Most common GI symptoms include diarrhea, nausea, vomiting and abdominal pain. Other symptoms include anorexia, anosmia, and dysgeusia. Notably, the GI symptoms in patients with COVID-19 appear early and may progressively worsen. Sometimes, GI symptoms can even be the sole presentation [1]. Ogilvie syndrome presents as colonic distension without signs of mechanical obstruction, in the context of autonomic nervous system dysfunction [3]. Very few cases of Ogilvie syndrome in patients with COVID-19 have been reported. We are aware of only one other case in the literature. Here we report a case of Ogilvie syndrome in a patient with longstanding multiple sclerosis (MS) who tested positive for SARS-CoV-2 4 weeks prior to hospital admission.
| Case Report | ▴Top |
A 60-year-old female with history of relapsing remitting MS on ocrelizumab, chronic obstructive pulmonary disease (COPD), and recent COVID-19 infection presented to the emergency department as a medical code for worsening dyspnea from a long-term care facility. On admission, she was hypotensive 109/80 mmHg, tachycardic 135 beats/min, tachypneic 29 breaths/min, with oxygen saturation of 85% on room air. She was put on a non-rebreather, changed to biphasic intermittent positive airway pressure (BiPAP) before ultimately escalating to intubation. Chest X-ray (CXR) (Fig. 1) showed bilateral mid to lower lung opacities concerning for multifocal viral pneumonia. COVID-19 nasopharyngeal polymerase chain reaction (PCR) was negative, while SARS-CoV-2 immunoglobulin G (IgG) antibody was positive at 4.67, in line with a recent COVID-19 infection confirmed by nasopharyngeal PCR 4 weeks prior to admission. Fecal PCR is not standard protocol at our institution.
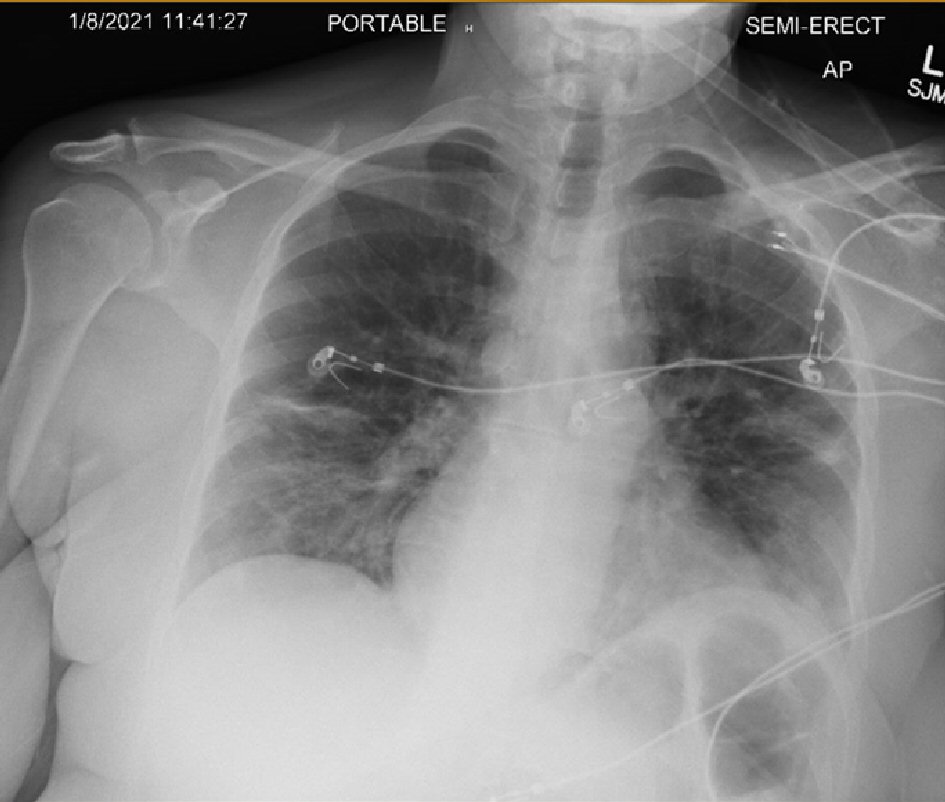 Click for large image | Figure 1. Chest X-ray (single view) showing bilateral ill-defined low-density opacities of mid and lower lung concerning for multifocal viral pneumonia, suggestive of COVID-19 pneumonia. COVID-19: coronavirus disease 2019. |
Inflammatory markers were elevated (C-reactive protein (CRP) > 1,800 mg/L (< 5.0 mg/L), D-dimer 15.59 mg/L (< 0.5 mg/L), fibrinogen 686 mg/dL (186 - 466 mg/dL), ferritin 662.5 ng/mL (11 - 306.8 ng/mL), lactate dehydrogenase (LDH) 476 U/L (140 - 271 U/L)) with a leukocytosis of 27.4 × 103/µL (3.5 - 10.6 × 103/µL) and lactic acidosis of 3.1 mMol/L (0.4 - 2.0 mMol/L). Alanine aminotransferase (ALT) and aspartate aminotransferase (AST) were within normal range. Intravenous (IV) fluid boluses and anticoagulation with heparin were started for concerns of a possible massive pulmonary embolism (PE). A computerized axial tomography (CT) scan of the thorax (Fig. 2) showed extensive pulmonary emboli and right heart strain, for which she underwent urgent thrombectomy on admission. She only took a one-time 650 mg acetaminophen tablet after the procedure and was started on lifelong anticoagulation.
 Click for large image | Figure 2. CT thorax for PE with contrast: positive for extensive pulmonary emboli. CT: computerized axial tomography; PE: pulmonary embolism. |
A CT abdomen/pelvis with contrast was done 3 days after admission due to persistent leukocytosis and new onset abdominal tenderness. Imaging showed significant dilatation of the sigmoid colon, consistent with Ogilvie syndrome (Fig. 3). Despite having no previous history of constipation, the patient had no bowel movements for the past week during admission but was able to pass gas. She denied bloating, nausea, and vomiting. No recent surgeries or medication regimens could account for the new-onset constipation, except for a recent COVID-19 infection.
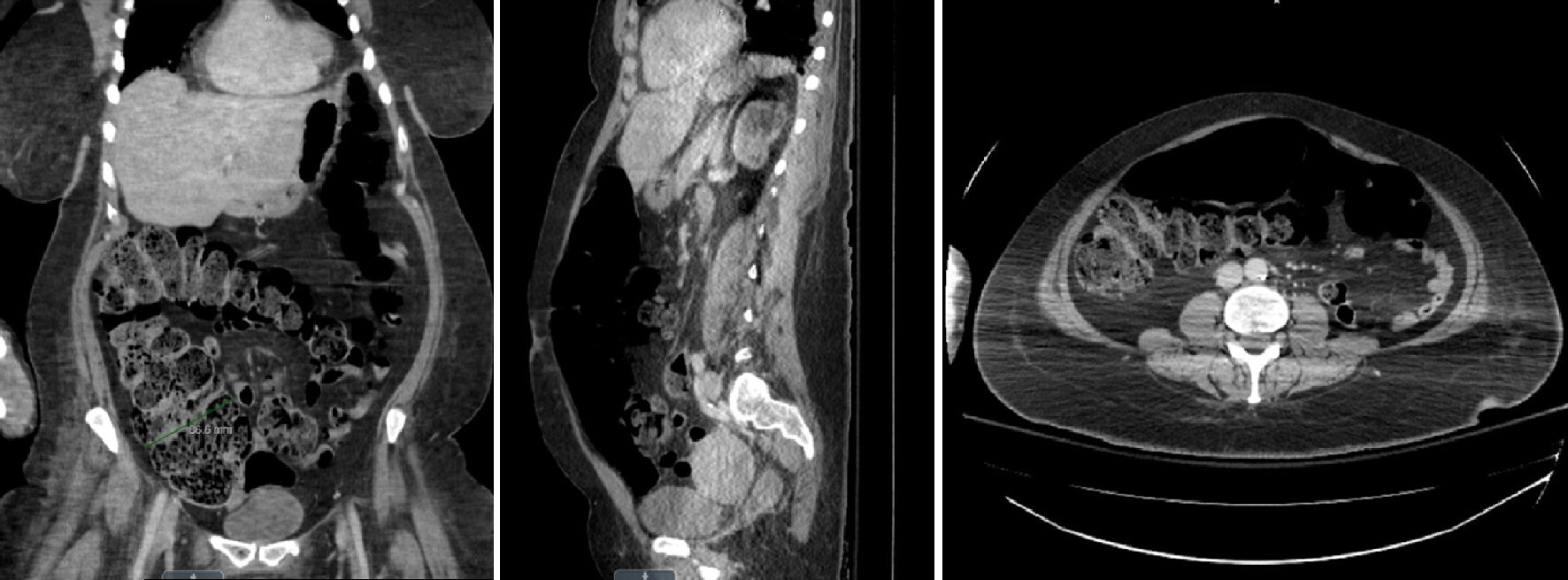 Click for large image | Figure 3. CT abdomen/pelvis with contrast: coronal, sagittal and axial views showing dilatation of the colon. CT: computerized axial tomography. |
Initial management included two tap water enemas 2 h apart, followed by neostigmine administration (2 mg IV over 3 - 5 min) and electrolyte replacement. One large liquid bowel movement was achieved after one dose of neostigmine. A follow-up abdominal X-ray showed moderate fecal stasis throughout the colon. A bowel regimen with polyethylene glycol 3350 and Senna twice daily was started, and the pseudo-obstruction resolved 12 days after admission with continuation of this regimen. On discharge, patient had persistent CXR findings of bilateral multifocal pneumonia consistent with COVID-19 infection, but her dyspnea had resolved.
| Discussion | ▴Top |
Several cases of paralytic ileus are among the myriad of GI complications reported already. SARS-CoV-2 binds to ACE-2 receptors on type 2 alveolar cells of the lungs and the GI tract in cholangiocytes, colonocytes, esophageal keratinocytes, and gastric/ileal/rectal epithelium cells [4] leading to side effects such as nausea, vomiting, diarrhea, and abdominal pain [5].
A systematic review and meta-analysis from researchers in Hong Kong explored the GI manifestations of SARS-CoV-2 infection and viral load in fecal samples. Cheung et al found that in 60 studies, comprising 4,243 patients, the prevalence of GI symptoms was 17.6% (95% confidence interval (CI): 12 - 24.5). Additionally, viral ribonucleic acid (RNA) was detected in the stool samples of 48.1% (95% CI: 38.3 - 57.9) of these patients; 70.3% of stool samples collected came back positive even though respiratory samples showed no infection [6]. Implications of this research include potential viral transmission through fecal samples, exercising caution when handling fecal waste in patients with recent COVID-19 infection with a negative nasopharyngeal swab PCR test, and potentially using fecal PCR as a means of assessing infectivity in patients with GI symptoms. Xiao et al also examined testing for viral RNA in feces with PCR as a method of monitoring the viral load and recommended continued precautions due to the potential fecal-oral transmission of this virus [7]. This is especially important to consider in individuals who have GI symptoms, like our patient.
There is currently only one other case linking COVID-19 infection as a cause of Ogilvie syndrome. The patient involved was a younger male with an active COVID-19 infection [3]; while in our case, our patient was a middle-aged female with a recent COVID-19 infection. It is important to note that not only could Ogilvie syndrome be present in a patient with active COVID-19 infection but could also be in a patient with recent COVID-19 infection. In both cases, first-line treatments included enemas and neostigmine.
In patients with both Ogilvie syndrome and recent/active COVID-19 infection, it is important to try conservative management with a variety of different medications first (standard bowel regimens, enemas, neostigmine) and use colonic decompression only as a last resort given the potential nature of transmission through fecal matter. Management of Ogilvie includes serial physical examinations and plain abdominal radiographs every 12 - 24 h to evaluate the colonic diameter. In patients who fail this initial conservative management after 48 - 72 h and who have a cecal diameter > 12 cm, pharmacologic therapy with neostigmine can be used if there are no contraindications. Neostigmine, an acetylcholinesterase inhibitor, has shown resolution of acute colonic pseudo-obstruction after only one dose compared to placebo [8].
Critically ill patients with COVID-19 often develop extrapulmonary complications during their hospital course including transaminitis, severe ileus, GI bleeding, pancreatitis, bowel ischemia, and Ogilvie syndrome [9]. COVID-19 is an evolving viral infection with growing literature and data. It is important to quickly recognize Ogilvie syndrome as a potential complication of COVID-19 infection, promptly treat with conservative measures to prevent bowel perforation and ischemia and avoid the possible fecal-oral transmission of the virus.
Acknowledgments
We would like to thank our family and friends for their support.
Financial Disclosure
There are no financial interests to disclose.
Conflict of Interest
There is no conflict of interest in the manuscript.
Informed Consent
Informed consent was obtained from the patient for case publication.
Author Contributions
Jing Wang M.D. wrote the abstract, patient’s case, discussion, and added figures and references. Georgiana Marusca M.D. wrote introduction and neostigmine paragraph of discussion, added to references. Tooba Tariq M.D., Gastroenterology fellow, took care of patient, reviewed and edited manuscript, added to references. Bashar Mohamad M.D., GI attending, took care of patient, reviewed and edited manuscript.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
Abbreviations
COVID-19: coronavirus disease 2019; ACE-2 receptor: angiotensin-converting enzyme type 2 receptor; GI: gastrointestinal; SARS-CoV-2: severe acute respiratory syndrome coronavirus 2; MS: multiple sclerosis; COPD: chronic obstructive pulmonary disease; BiPAP: biphasic intermittent positive airway pressure; IgG: immunoglobulin G; CXR: chest X-ray; CRP: C- reactive protein; LDH: lactate dehydrogenase; ALT: alanine transaminase; AST: aspartate aminotransferase; PE: pulmonary embolism; CT: computerized axial tomography; IV: intravenous; RNA: ribonucleic acid; PCR: polymerase chain reaction
| References | ▴Top |
- Cha MH, Regueiro M, Sandhu DS. Gastrointestinal and hepatic manifestations of COVID-19: A comprehensive review. World J Gastroenterol. 2020;26(19):2323-2332.
doi pubmed - Galanopoulos M, Gkeros F, Doukatas A, Karianakis G, Pontas C, Tsoukalas N, Viazis N, et al. COVID-19 pandemic: Pathophysiology and manifestations from the gastrointestinal tract. World J Gastroenterol. 2020;26(31):4579-4588.
doi pubmed - Khan Z, Mukhtar K, Roman G, Shah AR, Hassan M, Ahmed M, et al. S1678 Ogilvie syndrome in a patient with COVID-19 infection. Am J Gastroenterol. 2020;115(1):S862-S863.
doi - Smyk W, Janik MK, Portincasa P, Milkiewicz P, Lammert F, Krawczyk M. COVID-19: Focus on the lungs but do not forget the gastrointestinal tract. Eur J Clin Invest. 2020;50(9):e13276.
doi - Redd WD, Zhou JC, Hathorn KE, McCarty TR, Bazarbashi AN, Thompson CC, Shen L, et al. Prevalence and characteristics of gastrointestinal symptoms in patients with severe acute respiratory syndrome coronavirus 2 infection in the United States: a multicenter cohort study. Gastroenterology. 2020;159(2):765-767 e762.
doi pubmed - Cheung KS, Hung IFN, Chan PPY, Lung KC, Tso E, Liu R, Ng YY, et al. Gastrointestinal manifestations of SARS-CoV-2 infection and virus load in fecal samples from a Hong Kong cohort: systematic review and meta-analysis. Gastroenterology. 2020;159(1):81-95.
doi pubmed - Xiao F, Tang M, Zheng X, Liu Y, Li X, Shan H. Evidence for gastrointestinal infection of SARS-CoV-2. Gastroenterology. 2020;158(6):1831-1833 e1833.
doi pubmed - Valle RG, Godoy FL. Neostigmine for acute colonic pseudo-obstruction: A meta-analysis. Ann Med Surg (Lond). 2014;3(3):60-64.
doi pubmed - Kaafarani HMA, El Moheb M, Hwabejire JO, Naar L, Christensen MA, Breen K, Gaitanidis A, et al. Gastrointestinal complications in critically ill patients with COVID-19. Ann Surg. 2020;272(2):e61-e62.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


