| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 11, Number 5, May 2020, pages 142-144
An Unusual Presentation of Insulinoma: Confusion With Psychiatric Symptoms
Basma Ataallaha, d, Mustafa Abdulrahmanb, Gregory Haggertyc
aDepartment of Internal Medicine, Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, Mather Hospital, Port Jefferson, NY 11777, USA
bDepartment of Internal Medicine, Flushing Medical Center, Flushing, NY, USA
cGraduate Medical Education, Mather Hospital/Northwell, Port Jefferson, NY 11777, USA
dCorresponding Author: Basma Ataallah, Department of Internal Medicine, Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, Mather Hospital, Port Jefferson, NY 11777, USA
Manuscript submitted April 18, 2020, accepted April 24, 2020
Short title: Unusual Presentation of Insulinoma
doi: https://doi.org/10.14740/jmc3477
| Abstract | ▴Top |
Insulinoma is a rare but common functional neuroendocrine tumor that secretes an excess amount of insulin resulting in mostly fasting hypoglycemia but can also cause postprandial hypoglycemia. It usually presents with neuroglycopenic and autonomic sympathetic symptoms that resolve following the administration of dextrose. The patients may remain symptomatic from 1 week to as long as several decades before diagnosis. Insulinoma presenting with psychiatric symptoms has been documented in case/case series reports. Laboratory findings of elevated insulin and C-peptide level in the presence of hypoglycemia and absence of plasma sulfonylurea are suggestive of the diagnosis. Localization of the tumor is essential preoperatively. Surgery usually cures most of the patients, but a minority will have a recurrence especially with malignant insulinoma. The manuscript presents a case of insulinoma presenting with psychiatric symptoms without sympathetic symptoms that led to the delay of the diagnosis for 3 months as initially thought to be related to psychiatric problems. Pancreatic insulinoma was localized by computed tomography (CT) scan and confirmed with endoscopic ultrasound (EUS). The patient underwent successful resection of the tumor, and her symptoms were completely resolved.
Keywords: Endocrinology; Neuroendocrine tumors; Insulinoma; Hypoglycemia; Psychiatric disorder; Hallucinations
| Introduction | ▴Top |
Insulinoma is the most common neuroendocrine tumor causing hypoglycemic episodes. Its annual incidence is approximately 1 in 100,000 of the population, representing 1-2% of all pancreatic neoplasms [1]. The symptoms of hypoglycemia include sympathetic overactivity symptoms, as expressed by fatigue, weakness, tremor, sweating and tachycardia, and neuroglycopenic symptoms that causes central nervous system (CNS) disturbances like confusion, disorientation, blurring of vision, delirium, stupor, coma or convulsions. The diagnostic criterion for insulinoma is the Whipple triad which includes having symptoms of hypoglycemia, documented low blood glucose (40 - 50 mg/dL) and relief of symptoms after the intravenous administration of glucose. Normal to inappropriately high levels of serum insulin during symptomatic hypoglycemia are suggestive of the diagnosis. If high insulin level is suspected to be due to exogenous insulin use, C-peptide levels will be helpful in diagnosis. Imaging will help to localize the tumor with abdominal ultrasound (US), computed tomography (CT) scan, magnetic resonance imaging and endoscopic US (EUS). The main treatment of insulinoma is surgical resection of the tumor and is done either through open or laparoscopic approaches. Surgical options include simple enucleation, distal pancreatectomy or pancreaticoduodenectomy. We present the case of a young woman with history of recurrent episodes of hallucinations and behavioral symptoms, initially thought to be related to psychiatric disorder but, after thorough investigation, she was diagnosed with pancreatic insulinoma. The patient underwent successful resection of the tumor and her symptoms showed complete resolution.
| Case Report | ▴Top |
A 27-year-old woman presented to the hospital with a 3-month history of hallucinations and behavioral symptoms. These symptoms occurred mostly in the morning and occasionally during the day. Her boyfriend noticed these symptoms and reported that she was unresponsive during these episodes often screaming, crying and not responding to questions. These episodes were relieved after eating. The patient also had no memory of the events afterwards. Her medical history included irritable bowel syndrome. Her family, surgical and social histories were noncontributory. She was not taking any medications.
Upon presentation, she was afebrile, and her blood pressure, pulse rate, and respiratory rate were observed to be 110/68 mm Hg, 80 beats/min, and 17 breaths/min, respectively. Her physical examination, including a neurological exam, was normal. Routine laboratory investigations were all within the normal limits except her blood sugar on biochemical values was found to be 31 mg/dL. The patient was given dextrose intravenously in the Emergency Department and started on fluids with dextrose. She was admitted for further evaluation of her symptoms. The 72-h fasting test was notable for a serum glucose of 45 mg/dL associated with inappropriately normal levels of insulin of 8.3 µIU/mL (normal level 2.5 - 25.0), C-peptide level of 2.4 ng/mL (1.5 - 5.0), and elevated level of pro-insulin level of 25.7 (0.0 - 10.0 pmol/L). Laboratory data also were remarkable for a negative sulfonylurea screen and negative for insulin antibodies. The symptoms quickly resolved following the administration of intravenous dextrose.
Patient was initially thought to have a psychiatric disorder given her behavioral symptoms and absence of sympathetic symptoms like tremor, palpitations and sweating. Given her symptoms and laboratory findings, abdominal and pelvis CT scan with intravenous contrast was performed which demonstrated suspicious lesion in the body of the pancreas measuring 1.6 cm where insulinoma was suspected. Patient underwent magnetic resonance cholangiopancreatography (MRCP) and EUS for confirming the diagnosis with biopsy of the lesion that revealed a solitary neuroendocrine tumor (Figs. 1-3). Patient underwent pancreatic enucleation of the tumor with complete resolution of her symptoms without further evidence of hypoglycemic episodes.
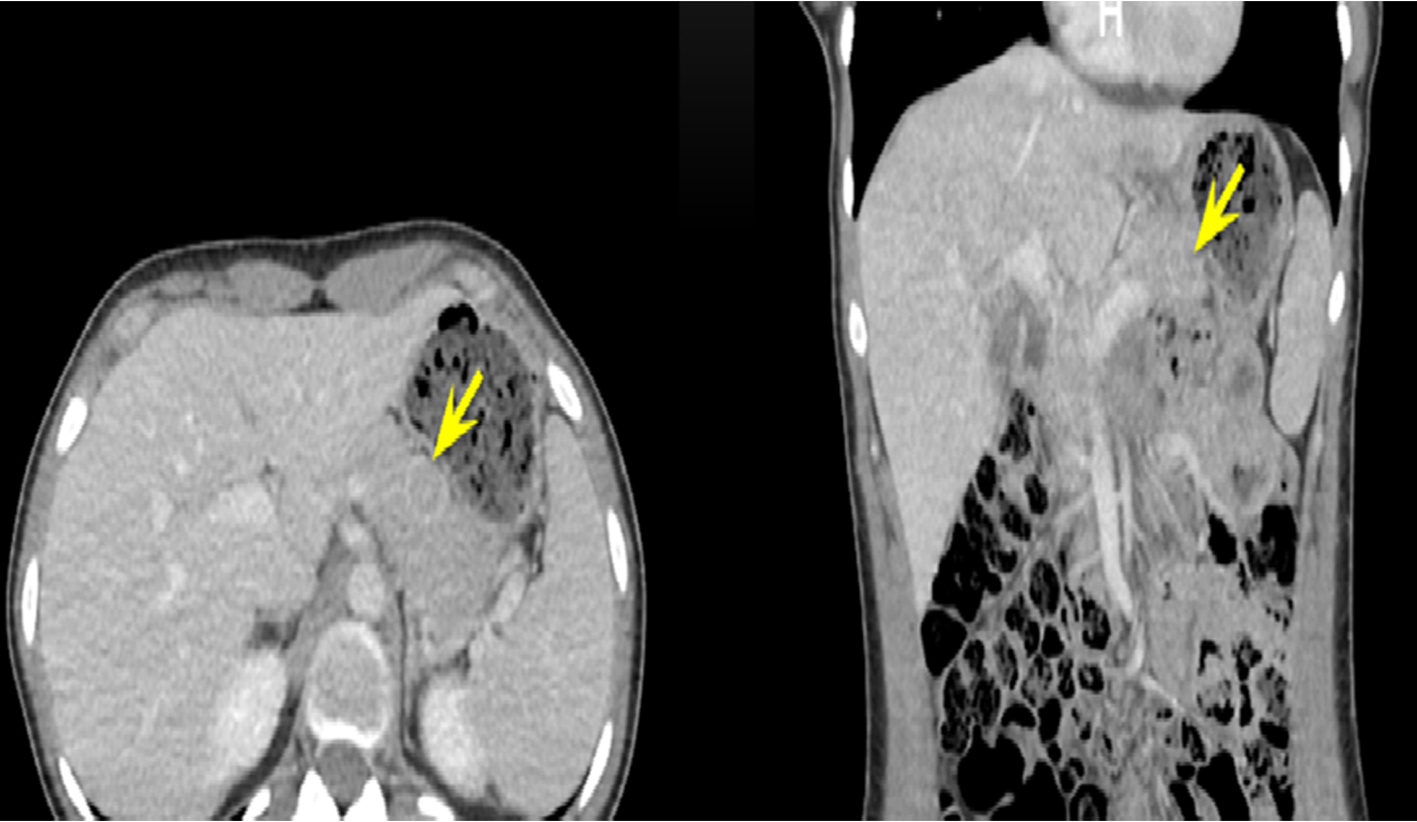 Click for large image | Figure 1. Abdomen/pelvis CT with intravenous contrast done on admission showed 1.6-cm lesion involving the pancreatic body. CT: computed tomography. |
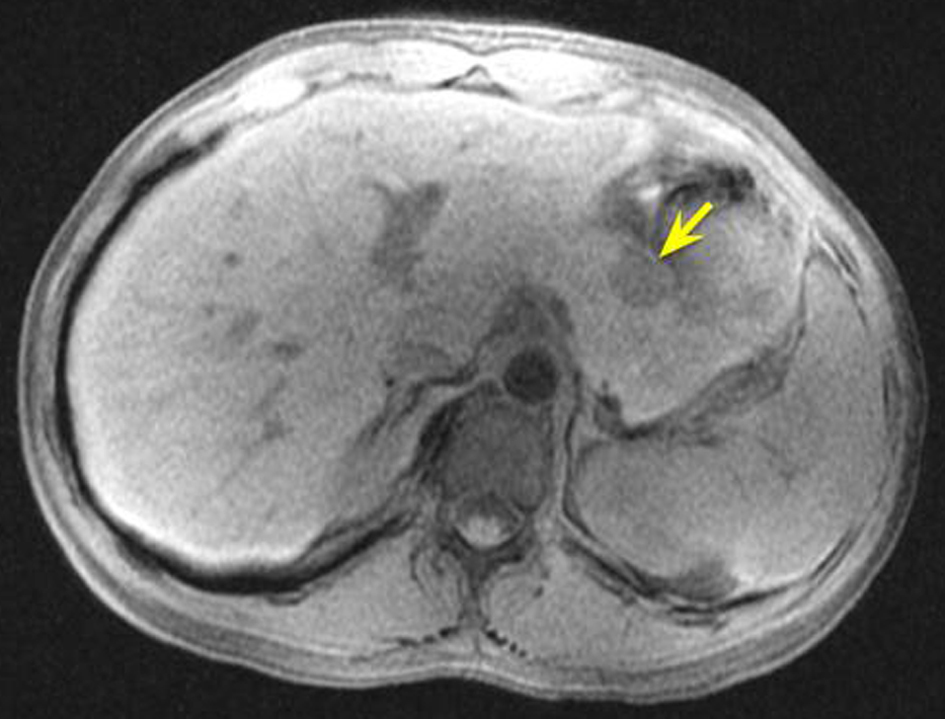 Click for large image | Figure 2. MRCP (pre-contrast, T1-weighted) confirmed a 1.9 × 1.6 cm lesion in the pancreatic body. MRCP: magnetic resonance cholangiopancreatography. |
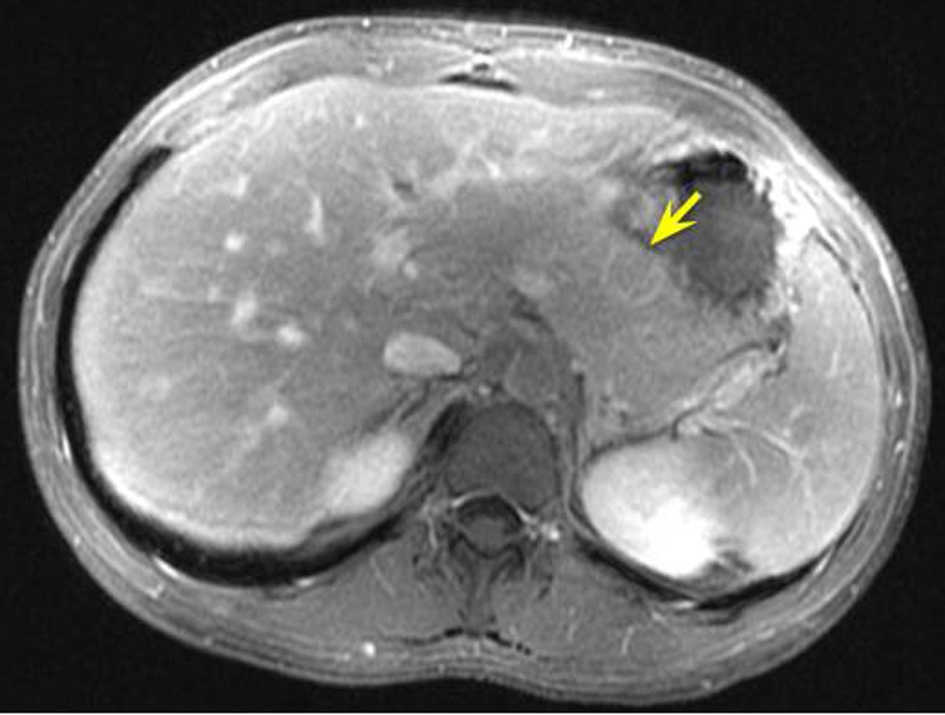 Click for large image | Figure 3. MRCP (post-contrast, T1-weighted). MRCP: magnetic resonance cholangiopancreatography. |
| Discussion | ▴Top |
The diagnosis of insulinoma is challenging and usually requires the presence of Whipple triad which consists of neuroglycopenic symptoms (e.g. confusion, change in behavior) and autonomic symptoms (e.g. tremor, sweating and palpitation) in the presence of low serum glucose level (less than 50 mg/dL) that resolves following the administration of glucose [2]. Insulinoma might be misdiagnosed as a seizure or psychiatric disorder like our patient here who was misdiagnosed initially as having psychotic disorder [2]. The 72-h supervised fasting test is the classic diagnostic test for insulinoma which demonstrates inappropriate normal to high level of insulin (≥ 6 µIU/mL) and C-peptide (≥ 2 ng/mL) levels in the presence of hypoglycemia and absence of sulfonylurea in the plasma [2].
Insulinoma is usually a benign and solitary tumor in 90% of the cases [2]. In only 10% of the cases, it occurs in conjunction of multiple endocrine neoplasia type 1 (MEN1 syndrome) [2, 3]. The diagnosis can be very challenging as patients with insulinoma usually remain undiagnosed for at least 1.5 years before developing symptoms [4]. MEN1 syndrome is an autosomal dominant disorder caused by a mutation in the MEN1 gene in the chromosome 11. Insulinomas associated with MEN1 syndrome are often multicentric and develop earlier compared to sporadic insulinomas [3].
After confirming the diagnosis with laboratory workup, imaging modalities are used to localize the tumor to determine the type of the surgery required. The noninvasive imaging tests include CT scan, magnetic resonance imaging, transabdominal ultrasonography, somatostatin receptor scintigraphy, and positron emission tomography. The diagnosis of an insulinoma is often delayed in some cases which have negative imaging scans. Invasive modalities are needed to localize the tumor such as EUS which is considered as the test of choice in most Western centers and selective arterial calcium stimulation test [2, 3].
Surgical resection is the treatment of choice of insulinoma [3]. Complete enucleation is performed in most cases as insulinoma is a solitary and benign tumor in more than 90% of cases [3]. If enucleation is not an option, distal or total pancreatectomy or Whipple procedure can be performed. After surgical treatment, the majority of patients are cured of the disease. For patients who are not a candidate for surgical resection or awaiting surgery, medical treatment can be used such as diazoxide and octreotide for symptomatic relief [3].
Conclusions
Despite the improvement in imaging modalities, the diagnosis of an insulinoma is often delayed. A detailed history about neuroglycopenic symptoms from patients and family is necessary with the episodes of hypoglycemia due to endogenous hyperinsulinemia. A history of neuroglycopenic symptoms should suggest the diagnosis of hypoglycemia associated with a hyperinsulinemic state.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
The authors report no conflict of interest.
Informed Consent
Not applicable.
Author Contributions
BA was the first author, collected data, guided the literature search, and wrote the manuscript. MA helped collecting data and writing the article. GH reviewed and supervised the study.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Oberg K, Eriksson B. Endocrine tumours of the pancreas. Best Pract Res Clin Gastroenterol. 2005;19(5):753-781.
doi pubmed - Okabayashi T, Shima Y, Sumiyoshi T, Kozuki A, Ito S, Ogawa Y, Kobayashi M, et al. Diagnosis and management of insulinoma. World J Gastroenterol. 2013;19(6):829-837.
doi pubmed - Taye A, Libutti S. Diagnosis and management of insulinoma: current best practice and ongoing developments. Dove press. 2015;5:125-133.
doi - Armbruster S, Dorrance C, Voorhees P, Pingpank JF, Kurland JE. Malignant insulinoma: a rare presentation of a rare tumor. Gastrointest Endosc. 2007;66(6):1228-1229; discussion 1229.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


