| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 11, Number 1, January 2020, pages 22-25
Recurrence of Paget-Schroetter Syndrome: A Rare Case Report and Review of Literature
Arda Akoluka, Steven Douedia, b, Jaraad Dattadeena, Ishan Patela, Arman Mushtaqa, Michael Levitta, Arif Asifa, Mohammad Hossaina
aDepartment of Medicine, Jersey Shore University Medical Center, Hackensack Meridian Health, Neptune, NJ 07753, USA
bCorresponding Author: Steven Douedi, Internal Medicine Residency Program, Department of Medicine, Jersey Shore University Medical Center, Hackensack Meridian Health, Neptune, NJ 07753, USA
Manuscript submitted January 5, 2020, accepted January 15, 2020
Short title: Paget-Schroetter Syndrome: A Case Report
doi: https://doi.org/10.14740/jmc3416
| Abstract | ▴Top |
Paget-Schroetter syndrome (PSS) is a primary upper extremity deep vein thrombosis (DVT) that occurs with no significant risk factors, mostly in a young and healthy patient. Treatment of this disease is discussed heavily in the literature and the optimal treatment method is still being debated. Here, we present a patient with PSS treated with balloon angioplasty, thrombolysis and treatment with an oral thrombin inhibitor (apixaban) who developed recurrence of PSS. A 38-year-old white male with no past medical history, presented to an urgent care center with sudden onset axillary pain and an axillary lump that was treated with outpatient antibiotics. Extensive deep venous thrombosis was diagnosed with computed tomography (CT) and ultrasound. He underwent percutaneous pharmacomechanical thrombectomy. Postprocedural angiogram showed significant improvement in the caliber of the axillary and subclavian veins where they crossed the first rib. He was discharged on apixaban and underwent removal of his first rib 1 month later. He returned 3 weeks later with recurrence of right arm pain and swelling. Repeat ultrasound showed thrombus in the right arm and venogram confirmed 80% stenosis at the subclavian vein as it enters the innominate vein. He was again treated with placement of a thrombolytic catheter and overnight thrombolysis of the central venous circulation on the right-side upper extremity balloon angioplasty of the subclavian vein, axillary vein, and basilic vein. He is disease-free for 6 months. Recurrence of PSS after surgical removal of rib, thrombectomy, thrombolysis while using apixaban is very rare. This is the first case to our knowledge presented with recurrent PSS treated with apixaban, early rib resection, balloon angioplasty and thrombectomy.
Keywords: Paget-Schroetter syndrome; Deep vein thrombosis; Recurrence
| Introduction | ▴Top |
Deep venous thrombosis (DVT) occurs rarely in axillo-subclavian vein. Common risk factors to have this rare type of DVT include prolonged immobility, previous thrombosis and hypercoagulable states [1]. In the absence of known risk factors, axillo-subclavian thrombosis is called Paget-Schroetter syndrome (PSS) [2]. PSS is a primary upper extremity DVT that occurs with no significant risk factors, mostly in a young and healthy patient. Treatment of this disease is discussed heavily in the literature, and optimal treatment method is still being debated. Here, we present a patient with PSS treated with balloon angioplasty, thrombolysis and treatment with an oral thrombin inhibitor (apixaban) who developed recurrence of PSS. This is the first case to our knowledge presented with recurrent PSS treated with apixaban, early rib resection, balloon angioplasty and thrombectomy.
| Case Report | ▴Top |
A 38-year-old white male with no past medical history, presented to an urgent care center with sudden onset axillary pain and an axillary lump, that was treated with outpatient antibiotics suspected possible infection. The patient’s condition did not improve. After 4 - 5 days, patient came to the emergency room (ER) with the same complaints. His vital signs were stable. On physical exam, he had 2 × 3 tender, palpable mass in the right axillary area with local warmth. Distal extremity and remaining physical exam were unremarkable. Initial laboratory investigation was unremarkable except for elevated C-reactive protein (CRP) level of 5.05 (reference value: 0 - 0.744 mg/dL). Ultrasound (US) of upper extremities revealed an extensive DVT involving the right axillary, subclavian, basilic, and jugular vein, but sparing the superior vena cava. He did not admit any usage of intravenous drugs. Vascular surgery and hematology/oncology were consulted. He underwent percutaneous pharmacomechanical thrombectomy. This technique involves mechanical dispersion of the clot with a single bolus of thrombolytic agent, using a continuous aspiration mechanical thrombectomy catheters device. Postprocedural angiogram showed significant improvement in the caliber of the axillary and subclavian veins where they crossed the first rib (Fig. 1). Intravascular ultrasound showed normal diameter of innominate and axillary veins with nearly complete compression/occlusion of the subclavian vein confirming the diagnosis of PSS (Fig. 1). Additional thrombectomy was performed. All hypercoagulable workup was negative which included computed tomography (CT) for chest/abdomen/pelvis for malignancy, factor 5 Leiden mutation, circulating lupus anticoagulant, protein C and S levels. He was discharged on apixaban and underwent removal of his first rib 1 month later. He remained on apixaban after the surgery. However, he returned 3 weeks later with recurrence of right arm pain and swelling. Repeat ultrasound showed thrombus in the right arm and venogram confirmed 80% stenosis at the subclavian vein as it enters the innominate vein. He was again treated with placement of a thrombolytic catheter and overnight thrombolysis of the central venous circulation on the right-side upper extremity balloon angioplasty of the subclavian vein, axillary vein, and basilic vein. He remains disease-free for 6 months on follow-up.
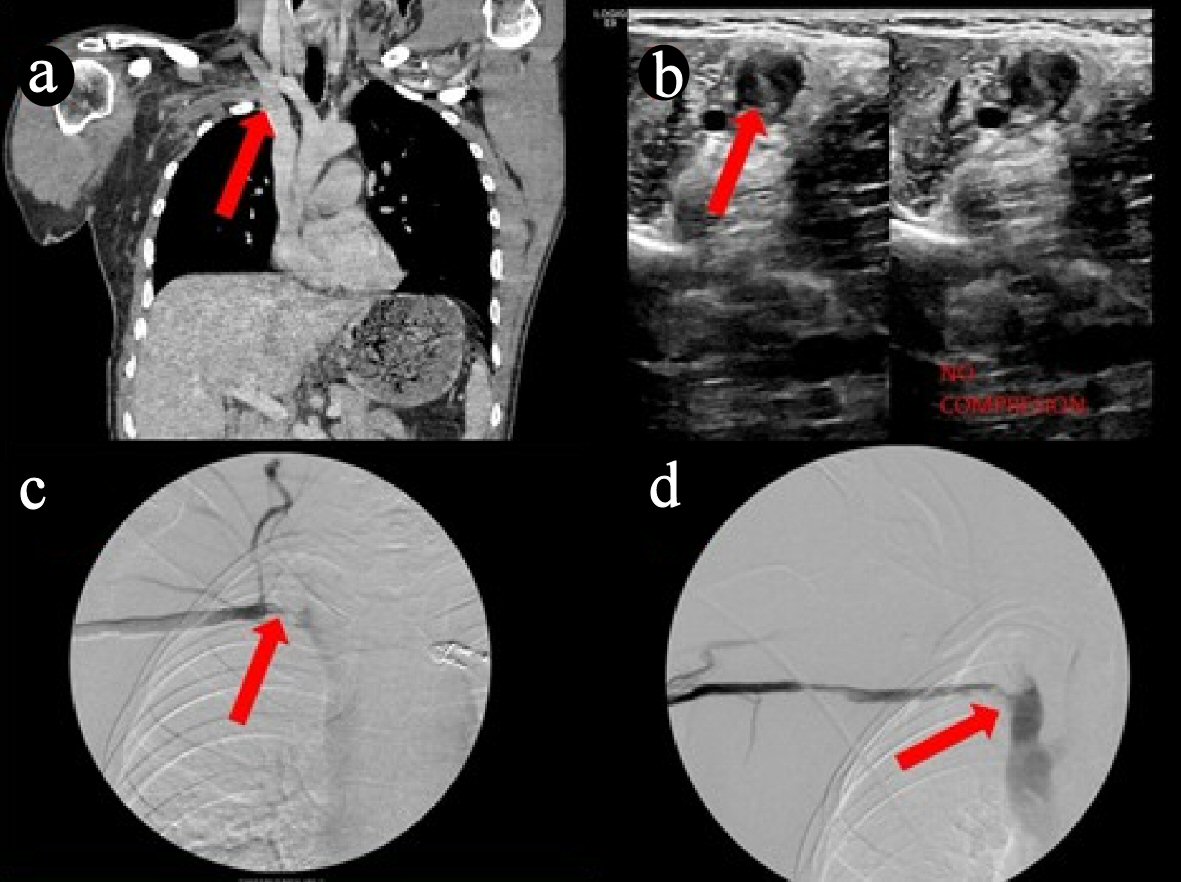 Click for large image | Figure 1. (a) Top-left: coronal computer tomography angiography (CTA) showing deep venous thrombosis (DVT) involving the entire right subclavian and axillary veins. The clot extends partially into the jugular vein. (b) Top-right: Doppler studies showing thrombus present in right subclavian vein. (c, d) Bottom-left and right: angiography showing thrombus extending into right subclavian and axillary veins. |
| Discussion | ▴Top |
To the best of our knowledge, this is the first patient diagnosed with PSS with recurrence after treatment with thrombolysis and rib resection while on apixaban. His vague presentation with only axillary lump made the diagnosis difficult; however, what made this case very challenging for our multidisciplinary team was his failure of treatment even on apixaban for his second admission. PSS is a rare condition with incidence of around 1 per 100,000 patients per year [1, 3]. It is more common on the right, likely because of right-hand dominance [4]. Although it is rare, this disease should be considered in the differential diagnosis as treatment approach can significantly change within 6 weeks of presentation. The pathogenesis is still debated and its connection with sporting activities such as wrestling and vigorous upper extremity movements made scientist believe that hyperabduction and microtrauma to upper extremity venous system plays role in PSS [5]. There is also significant evidence pointing towards anatomical structures like hypertrophy of scalenus tendons and abnormal insertion of costoclavicular ligament and congenital bands leading to this disease [6]. The low incidence does not allow enrollment in clinical trials, so treatment for PSS is still debated and is at the discretion of the treating physicians [6]. Despite the lack of substantial randomized controlled evidence, standard of care is anticoagulation, thrombolysis, first rib removal or correction of any anatomical factor, and venoplasty/angioplasty [2, 7-9]. Post-operative anticoagulation is still debated but most recommend 3 months of anticoagulation [4, 8, 10].
In one article reporting 50 years of experience, Urschel et al highlight the benefit of anticoagulation in patients with good surgical outcome. In this retrospective study of 608 patients, four groups were created and divided according to treatment and/or time of thrombosis. Comparison of the number of extremities and recurrence along with outcomes of functional status and resolution of symptoms were observed [6]. Group 1 consisted of 36 extremities of patients who were treated before 1975 seen before 6 weeks of thrombosis and treated with anticoagulant therapy, defined as heparin followed by warfarin. Recurrence or persistent symptoms was noted in 26 of the extremities and 21 of those required re-hospitalization and resection of the first rib and scalenus anticus muscle. Ten of the 36 extremities had significant improvement of symptoms with anticoagulation. Group 2 consisted of 45 extremities treated after 1975 in which thrombolytic agents were used. Twenty-five of the 45 extremities in this group underwent first rib resection with excellent outcomes. These patients were mostly able to return to work within 6 weeks without the need for anticoagulation. Group 3 patients consisting of 506 extremities seen within 6 weeks of the thrombosis were also treated with thrombolytic agents followed by immediate reception of the first rib. Four hundred eighty-six extremities in this group had significant improvement of symptoms. Group 4 consisted of 42 extremities seen 6 weeks after thrombosis with similar treatment as group 2 and 3. Twenty-four extremities in this group had improved outcomes while the remainder had fair/poor outcomes, and some required additional Roto-rooter treatment and surgery.
While Roto-rooter treatment was found to be effective in some patients, dense and hard fibrotic lesions were unable to be recanalized leading to failure of treatment. In some cases, surgeons decided to use stenting as well but Urschel et al recommends against it, as in their experience they tend to bend and brake making the re-operation if needed extremely difficult [6, 8]. However, this aspect also lacks high quality data. The retrospective study by Urschel et al suggests early thrombolytic therapy with urokinase followed by first rib resection leads to significantly improved patient outcomes, especially in those managed within 6 weeks of the thrombosis [6]. In our case, we used early aggressive surgical treatment with prompt rib resection; however, even when the patient was on apixaban he had recurrence of symptoms.
Finally, the duration and type of anticoagulation remain unclear in PSS patients, especially when there is recurrence [2-4]. Use of direct oral anticoagulants (DOAC) is increasing due to their convenience and less bleeding in those requiring long-term anticoagulation [11]. Owing to the fact that PSS is very rare, there are no studies comparing DOACs and warfarin in complex scenarios of recurrence, but given the data regarding their efficacy and safety treating acute venous thromboembolism, DOAC are a reasonable choice for anticoagulation [4, 10].
Conclusions
Recurrence of PSS after surgical removal of rib, thrombectomy, and thrombolysis while using apixaban is very rare. While some studies recommend early thrombolytic therapy followed by first rib resection, there is no high-quality data to guide management when there is failure of aggressive surgical resection and anticoagulation. Further studies and prospective trials are required to develop an optimal treatment method for PSS, however, are limited due to PSS rarity.
Acknowledgments
None to declare.
Financial Disclosure
The authors have not obtained funding to disclose for this publication.
Conflict of Interest
The authors declare that there is no conflict of interest regarding the publication of this paper.
Informed Consent
The patient described in the case report had given informed consent for the case report to be published.
Author Contributions
Arda Akoluk, Steven Douedi, and Jaraad Dattadeen: article authors; Michael Levitt: consultant during patient care; Ishan Patel, Arman Mushtaq, Arif Asif, and Mohammad Hossain: article editors.
Data Availability
Data supporting the findings of this study are available within the article.
| References | ▴Top |
- Hangge P, Rotellini-Coltvet L, Deipolyi AR, Albadawi H, Oklu R. Paget-Schroetter syndrome: treatment of venous thrombosis and outcomes. Cardiovasc Diagn Ther. 2017;7(Suppl 3):S285-S290.
doi pubmed - Urschel HC, Jr., Razzuk MA. Paget-Schroetter syndrome: what is the best management? Ann Thorac Surg. 2000;69(6):1663-1668; discussion 1668-1669.
doi - Machleder HI. Evaluation of a new treatment strategy for Paget-Schroetter syndrome: spontaneous thrombosis of the axillary-subclavian vein. J Vasc Surg. 1993;17(2):305-315; discussion 316-307.
doi - Illig KA, Doyle AJ. A comprehensive review of Paget-Schroetter syndrome. J Vasc Surg. 2010;51(6):1538-1547.
doi pubmed - Melby SJ, Vedantham S, Narra VR, Paletta GA, Jr., Khoo-Summers L, Driskill M, Thompson RW. Comprehensive surgical management of the competitive athlete with effort thrombosis of the subclavian vein (Paget-Schroetter syndrome). J Vasc Surg. 2008;47(4):809-820; discussion 821.
doi pubmed - Urschel HC, Jr., Patel AN. Surgery remains the most effective treatment for Paget-Schroetter syndrome: 50 years' experience. Ann Thorac Surg. 2008;86(1):254-260; discussion 260.
doi pubmed - Molina JE. Subclavian vein thrombosis paget-schroetter syndrome. Cardiothoracic Surgical Procedures and Techniques. Springer. 2018;117-126.
doi - Kreienberg PB, Chang BB, Darling RC, 3rd, Roddy SP, Paty PS, Lloyd WE, Cohen D, et al. Long-term results in patients treated with thrombolysis, thoracic inlet decompression, and subclavian vein stenting for Paget-Schroetter syndrome. J Vasc Surg. 2001;33(2 Suppl):S100-105.
doi pubmed - Angle N, Gelabert HA, Farooq MM, Ahn SS, Caswell DR, Freischlag JA, Machleder HI. Safety and efficacy of early surgical decompression of the thoracic outlet for Paget-Schroetter syndrome. Ann Vasc Surg. 2001;15(1):37-42.
doi pubmed - Haley JC, Bock C. Direct oral anticoagulants for venous thromboembolism: a pharmacological review. AACN Adv Crit Care. 2017;28(1):5-11.
doi pubmed - Lopez-Lopez JA, Sterne JAC, Thom HHZ, Higgins JPT, Hingorani AD, Okoli GN, Davies PA, et al. Oral anticoagulants for prevention of stroke in atrial fibrillation: systematic review, network meta-analysis, and cost effectiveness analysis. BMJ. 2017;359:j5058.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


