| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 9, Number 3, March 2018, pages 98-102
A Case of Recurrent Takotsubo Cardiomyopathy: Not a Benign Entity
Anthony H. Kashoua, b, Adam Custera, b, Nabil Braiteha, Pranava Ganesha, Keyoor Patela, Hisham E. Kashoua, c
aDepartment of Cardiology at United Health Services Hospitals, Wilson Regional Medical Center, Johnson City, NY 13790, USA
bThese authors contributed equally to this work.
cCorresponding Author: Hisham E. Kashou, Department of Cardiology, United Health Services Hospitals, Wilson Regional Medical Center, 30 Harrison St #250, Johnson City, NY 13790, USA
Manuscript submitted January 28, 2018, accepted February 8, 2018
Short title: Recurrent Takotsubo Cardiomyopathy
doi: https://doi.org/10.14740/jmc3011w
| Abstract | ▴Top |
Takotsubo cardiomyopathy is a relatively uncommon condition triggered by severe physical and/or emotional stress. It is characterized by transient ventricular wall dysfunction in the absence of coronary artery disease (CAD). Herein, we report a case of a 59-year-old female who had three episodes of recurrent Takotsubo cardiomyopathy. On each occasion, she presented with symptoms of acute coronary syndrome accompanied by left ventricular wall motion abnormalities; however, repeat cardiac catheterization failed to show CAD. Each recurrence resulted in resolution of her symptoms and recovery of left ventricular function. While emotional triggers were identified, on two occasions, the patient presented with ventricular fibrillation for which an implantable cardioverter defibrillator (ICD) was ultimately placed. We encourage clinicians to no longer look at Takotsubo cardiomyopathy as a benign, reversible disease process, but rather as a pathological entity with real, life-threatening complications that may be managed with ICD placement.
Keywords: Takotsubo cardiomyopathy; Stress-induced cardiomyopathy; Acute coronary syndrome; Coronary angiography; Ventricular arrhythmia
| Introduction | ▴Top |
Taktosubo, or stress-induced, cardiomyopathy is a syndrome characterized by transient ventricular wall dysfunction in the absence of coronary artery disease (CAD). The term “Takotsubo” was first described in 1990 and is taken from the Japanese word for an octopus trap, as it resembles the appearance of the heart with systolic apical ballooning. Taktosubo cardiomyopathy often mimics acute coronary syndrome (ACS) and occurs in approximately 2% of patients presenting with suspected ACS or ST elevation myocardial infarction (STEMI) [1, 2]. Recurrence is relatively uncommon and has been reported in only 5-6% of cases [3, 4]. Herein, we report a case of recurrent Takotsubo cardiomyopathy with emotional triggers in the setting of recurrent ventricular arrhythmias as well as shed light on this pathological entity with real, life-threatening complications that may be managed with implantable cardioverter defibrillator (ICD) placement.
| Case Report | ▴Top |
A 59-year-old female with a history of hypertension, dyslipidemia, recurrent ventricular fibrillation, tobacco abuse, and two prior admissions for Takotsubo cardiomyopathy presented to the hospital with chest pain. The patient reports she has been stressed recently as she is the primary caretaker for her niece who is handicapped. The chest pain was intermittent, substernal, and radiated to her left arm. It was similar to previous episodes when she was diagnosed with Takotsubo cardiomyopathy.
The patient was first diagnosed with Takotsubo cardiomyopathy 3 years prior to this admission. Electrocardiogram (ECG) at that time showed evidence of an acute anteroseptal STEMI. This was complicated by an episode of ventricular fibrillation for which she was defibrillated and received compressions for 20 min. The patient was stable with return of spontaneous circulation when she arrived to the hospital with resolution of the ST elevation. Her troponin level peaked at 4.32. The patient underwent cardiac catheterization, which revealed mild disease of the junction of the proximal and mild left anterior descending artery with evidence of apical and distal anterolateral and distal inferolateral akinesia consistent with Takotsubo cardiomyopathy (Fig. 1). The recommendation at that time was to be discharged on simvastatin, amlodipine, spironolactone-hydrochlorothiazide, ramipril, and aspirin.
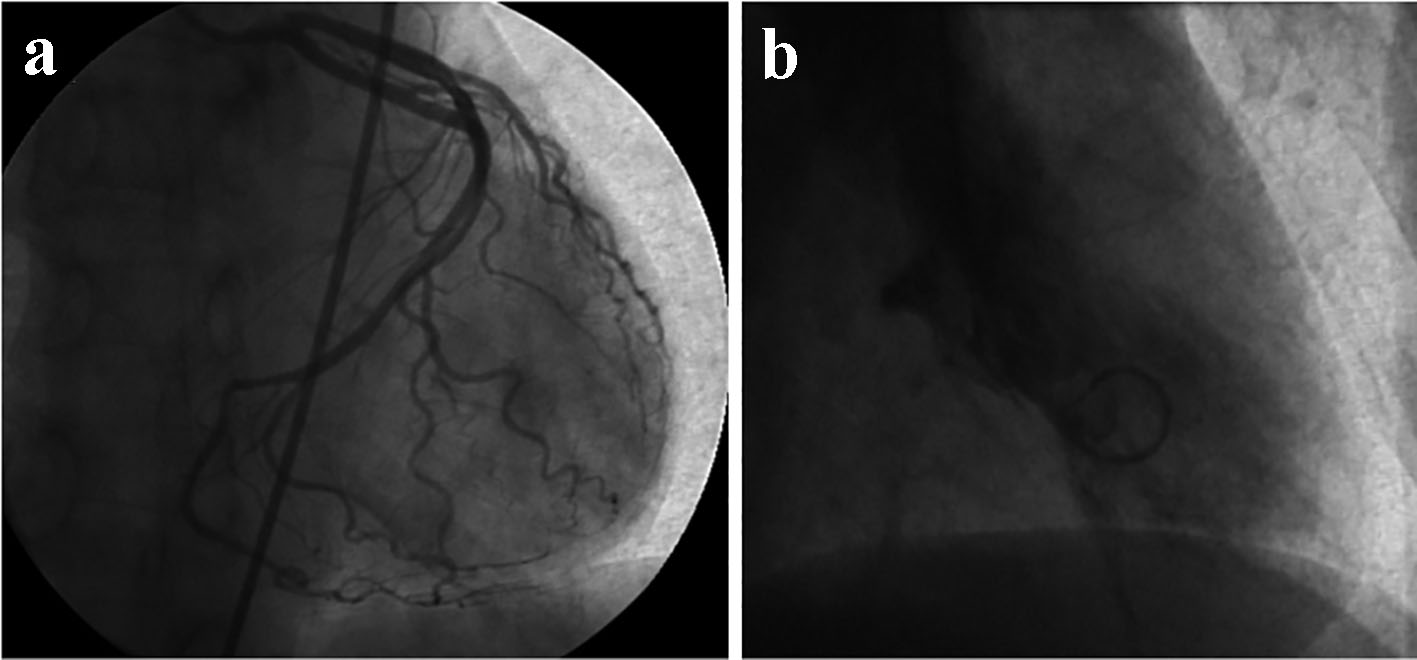 Click for large image | Figure 1. Cardiac catheterization showing mild disease of the junction of the proximal and mid left anterior descending artery (a). Evidence of apical and distal anterolateral and distal inferolateral akinesis consistent with Takotsubo cardiomyopathy (b). |
Three years later, the patient presented with similar chest pain that was complicated with ventricular fibrillation cardiac arrest that required resuscitation. ECG at that time showed evidence of acute anterior and inferior myocardial infarction. Troponin levels peaked at 6.720. Echocardiogram at that time showed a reduced ejection fraction of 25-30%, mild-moderate mitral valve regurgitation, as well as anteroseptal and apical/high-lateral hypokinesis. Cardiac catheterization revealed normal coronary arteries, a reduced ejection fraction of about 40%, mid-to-distal anterior-apical and inferoapical hypokinesis, and significant (4+) mitral regurgitation (Fig. 2). The patient was discharged 4 days later with plans for placement of an ICD the following week.
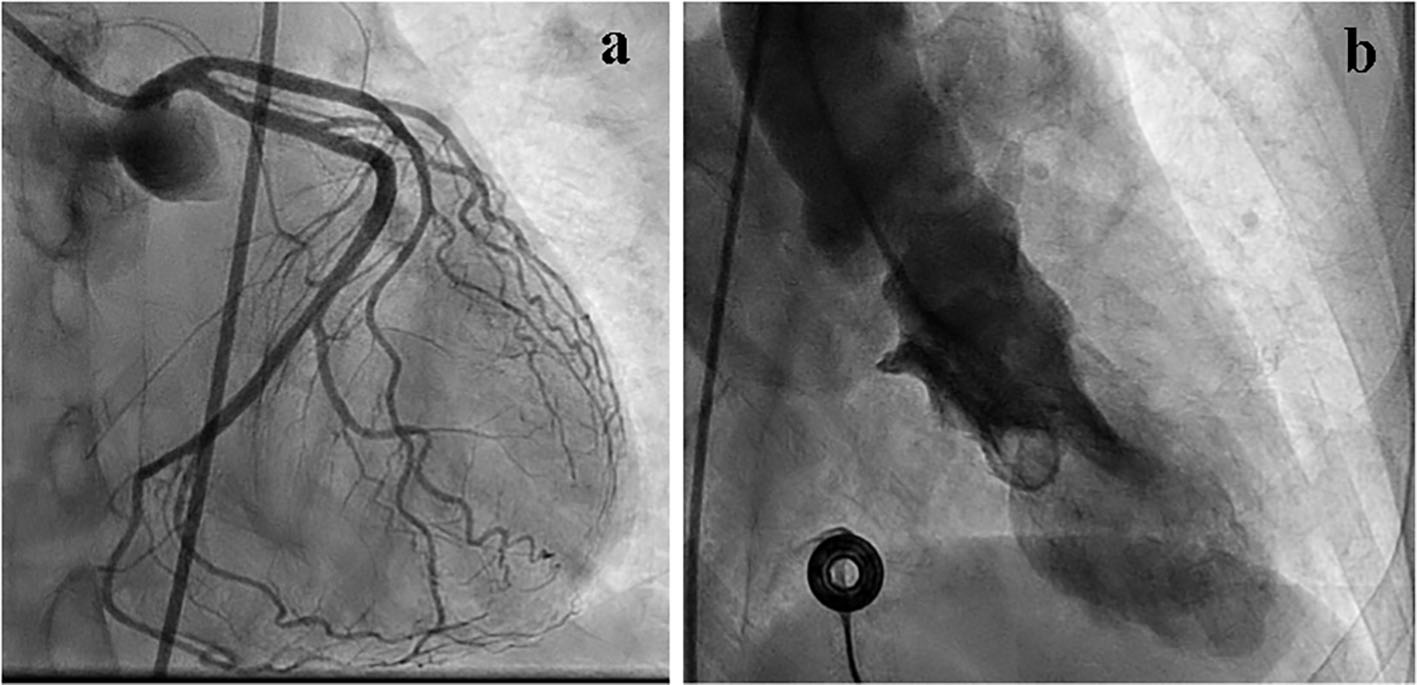 Click for large image | Figure 2. Cardiac catheterization showing normal coronary arteries (a). Evidence of mid-to-distal anterior apical and inferoapical hypokinesis consistent with Takotsubo cardiomyopathy (b). |
However, the next day, the patient returned to the hospital with worsening chest pain and a blood pressure of 166/86 mm Hg. Pulmonary and cardiovascular exams were unremarkable. Lab workup was noteworthy for an elevated troponin of 2.02, which increased from 1.820 yesterday upon discharge, brain natriuretic peptide (BNP) of 2,340, and urine catecholamines within normal limits. ECG showed new ST elevation in the anterolateral leads. Chest X-ray was unremarkable. Cardiac catheterization revealed improved left ventricular function with only mild apical hypokinesis and an ejection fraction of 50% without any mitral regurgitation, consistent with healing Takotsubo cardiomyopathy (Fig. 3). An ICD was eventually placed during this hospital course and the patient was discharged on aspirin, clopidogrel, carvedilol, ramipril, atorvastatin, isosorbide mononitrate, ranolazine, and amiodarone.
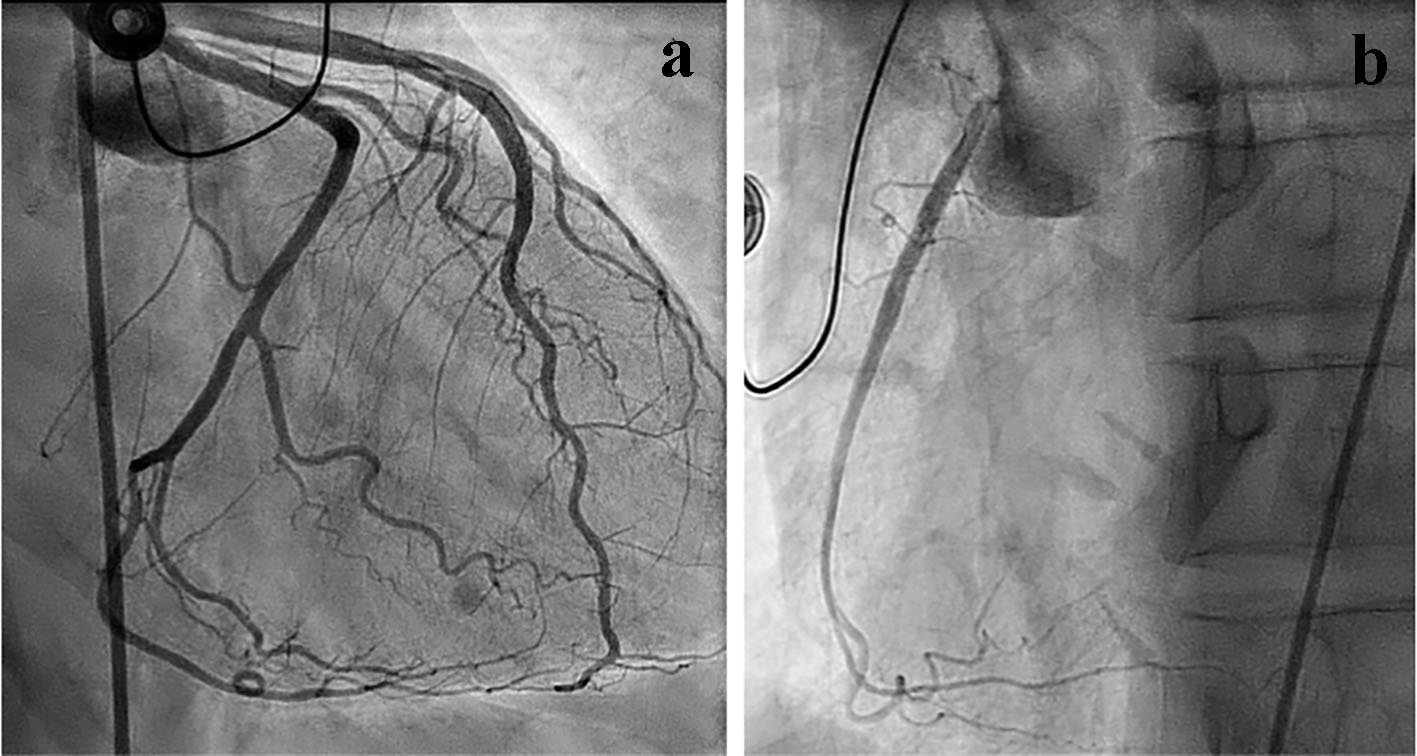 Click for large image | Figure 3. Cardiac catheterization showing normal coronary arteries (a). Evidence of improved left ventricular function with only mild apical hypokinesis, consistent with resolving Takotsubo cardiomyopathy (b). |
| Discussion | ▴Top |
Takotsubo cardiomyopathy is typically characterized by transient left ventricular wall motion abnormalities and normal coronary arteries. It can present with ECG changes and elevated cardiac enzymes. It appears to have a predilection towards postmenopausal women as the International Takotsubo Registry found 89.8% of patients were women with a mean age of 66.8 years [5].
Takotsubo cardiomyopathy has been found to be associated with physical and emotional triggers. Some of these stressors include pheochromocytoma, myocarditis, psychiatric illnesses, prolonged QT syndromes, COPD exacerbations, albuterol, hyperthyroidism, seizure disorders, electroconvulsive therapy, acute brain injury, and sepsis [6-15]. For this reason, the syndrome has also been referred to as “stress-induced” cardiomyopathy. Of the cases associated with triggers, 27.7% had emotional triggers, and 36% had physical triggers [5]. However, this is not always the case. Recent studies have shown up to 28.5% of patients have no evident trigger [5].
Although the pathogenesis of Takotsubo cardiomyopathy is still not well understood, there are currently three leading theories: 1) catecholamine release, 2) coronary artery spasm, and 3) microvascular dysfunction. The leading hypothesis involves catecholamine-induced microvascular spasm/dysfunction resulting in myocardial stunning [16]. Reports have shown exposure to supratherapeutic doses of catecholamines and beta-agonists can precipitate all the features of Takotsubo cardiomyopathy [17]. For such reasons, this syndrome has also been associated with other conditions, such as pheochromocytoma and acute brain injury, both of which are related to catecholamine excess [18, 19]. One study found 74% of patients with Takotsubo cardiomyopathy had elevated norepinephrine levels on presentation [2]. Another study found an apical-basal gradient of beta-2 adrenergic receptors in rats, which may explain the regional responses that generate the apical ballooning [20]. However, Madhavan et al found little-to-no diagnostic utility in the measurement of catecholamine or cortisol levels [21].
The diagnosis of Takotsubo cardiomyopathy should be suspected in all patients who present with ACS. Mayo Clinic has proposed four diagnostic criteria: 1) transient left ventricular dysfunction, 2) absence of coronary artery disease, 3) new ECG changes or elevated troponin levels, and 4) absence of pheochromocytoma or myocarditis [22]. Furthermore, not only do elevated BNP levels support the diagnosis, but the extent of BNP elevation can also be supportive. More than 80% of patients have been found to have elevated BNP levels at nearly twice the levels of those found in patients with CAD [5]. This patient met all four of the Mayo Clinic’s proposed diagnostic criteria and had an elevated BNP of 2,340, nearly twice the levels seen in CAD. While the patient’s urine catecholamines were normal, they were not taken during a period of documented active disease and may not rule out underlying catecholamine-induced microvascular dysfunction.
Due to the infrequent occurrence of recurrent Takotsubo cardiomyopathy, optimal management remains relatively unclear. Management is generally conservative as most patients will make a full recovery. Left ventricular dysfunction tends to normalize after 7 days [6]. Treatment should begin with removal of any precipitating emotional, physical, and/or inciting stressor(s). In cases of recurrent Takotsubo cardiomyopathy, treatment with angiotensin-converting-enzyme inhibitors (ACE-Is) and angiotensin II receptor blockers (ARBs) have been shown to reduce recurrence rates [4]. However, this patient had two episodes while on ramipril 10 mg oral daily. The use of beta-blockers has shown no significant difference in recurrence rates [4]. This suggests a potential protective role of ACE-Is and ARBs, and the possible involvement of these mechanisms in the underlying pathophysiology of the disease.
Takotsubo cardiomyopathy tends to have a favorable prognosis with most patients making a full recovery. Recurrence is relatively uncommon and has been reported in only 5-6% of cases, with a recurrence risk within the following year of 1.8% [3, 4]. Arterial hypertension has shown a positive correlation with recurrence rates [5]. While Takotsubo cardiomyopathy is often considered a benign entity, the overall risk of complications including cardiogenic shock, need for invasive or non-invasive ventilation, cardiopulmonary resuscitation, and death was found to be 19.1%, which is similar to that of patients with ACS [5]. The incidence of ventricular arrhythmias has been reported in 3.4% of cases and in 1.1% of cases upon initial presentation [23]. Refractory ventricular arrhythmias resulted in the death of 15% of patients with Takotsubo cardiomyopathy [24].
It is evident that Takotsubo cardiomyopathy is not a benign entity. While patients may recover normal cardiac function based on measured parameters, there appears to be a pathologic insult that may not be reversible. Given the significant complications associated with this syndrome, there may be underlying defects to the heart’s electrical conduction system or structure. Therefore, for some patients, insertion of an ICD may help manage the ventricular arrhythmia risk and prevent sudden cardiac death.
This patient with recurrent stress-induced Takotsubo cardiomyopathy complicated by recurrent and refractory ventricular arrhythmias further demonstrates that Takotsubo cardiomyopathy is not a benign entity; rather, it is a disease process with significant and potentially fatal complications. Even though the majority of patients make a full recovery, the thought that no myocardial injury occurred during its course is less likely. The transient left ventricular dysfunction may actually cause undetected permanent damage and be the reason for some of the described complications. Because ventricular arrhythmias are a known reported complication of Takotsubo cardiomyopathy, management plans should consider ICD placement. We encourage other clinicians to no longer look at Takotsubo cardiomyopathy as a benign, reversible disease process, but rather as a pathological entity with real, life-threatening complications.
Disclosure
Authors have no conflict of interest, and the work was not supported or funded by any drug company.
| References | ▴Top |
- Kurowski V, Kaiser A, von Hof K, Killermann DP, Mayer B, Hartmann F, Schunkert H, et al. Apical and midventricular transient left ventricular dysfunction syndrome (tako-tsubo cardiomyopathy): frequency, mechanisms, and prognosis. Chest. 2007;132(3):809-816.
doi pubmed - Gianni M, Dentali F, Grandi AM, Sumner G, Hiralal R, Lonn E. Apical ballooning syndrome or takotsubo cardiomyopathy: a systematic review. Eur Heart J. 2006;27(13):1523-1529.
doi pubmed - El-Battrawy I, Ansari U, Behnes M, Hillenbrand D, Schramm K, Haghi D, Hoffmann U, et al. Clinical and echocardiographic analysis of patients suffering from recurrent takotsubo cardiomyopathy. J Geriatr Cardiol. 2016;13(11):888-893.
pubmed - Singh K, Carson K, Usmani Z, Sawhney G, Shah R, Horowitz J. Systematic review and meta-analysis of incidence and correlates of recurrence of takotsubo cardiomyopathy. Int J Cardiol. 2014;174(3):696-701.
doi pubmed - Templin C, Ghadri JR, Diekmann J, Napp LC, Bataiosu DR, Jaguszewski M, Cammann VL, et al. Clinical features and outcomes of takotsubo (stress) cardiomyopathy. N Engl J Med. 2015;373(10):929-938.
doi pubmed - Chiang YL, Chen PC, Lee CC, Chua SK. Adrenal pheochromocytoma presenting with Takotsubo-pattern cardiomyopathy and acute heart failure: A case report and literature review. Medicine (Baltimore). 2016;95(36):e4846.
doi pubmed - Eliades M, El-Maouche D, Choudhary C, Zinsmeister B, Burman KD. Takotsubo cardiomyopathy associated with thyrotoxicosis: a case report and review of the literature. Thyroid. 2014;24(2):383-389.
doi pubmed - Elkhateeb OE, Beydoun HK. Recurrent long QT syndrome and syncope in transient apical ballooning syndrome (takotsubo cardiomyopathy). Can J Cardiol. 2008;24(12):917-919.
doi - Dastidar AG, Frontera A, Palazzuoli A, Bucciarelli-Ducci C. TakoTsubo cardiomyopathy: unravelling the malignant consequences of a benign disease with cardiac magnetic resonance. Heart Fail Rev. 2015;20(4):415-421.
doi pubmed - Corrigan FE, 3rd, Kimmel MC, Jayaram G. Four cases of takotsubo cardiomyopathy linked with exacerbations of psychiatric illness. Innov Clin Neurosci. 2011;8(7):50-53.
pubmed - Katsa I, Christia P, Massera D, Faillace R. Recurrent stress cardiomyopathy during COPD exacerbation: are beta-adrenergic agonists only to blame? Cureus. 2017;9(4):e1166.
doi - Patel B, Assad D, Wiemann C, Zughaib M. Repeated use of albuterol inhaler as a potential cause of Takotsubo cardiomyopathy. Am J Case Rep. 2014;15:221-225.
doi pubmed - Rossi P, Bernard F, Aissi K, Bonello L, Demoux AL, Bagneres D, Frances Y, et al. Takotsubo cardiomyopathy after seizure. BMJ Case Rep. 2010;2010.
- Cheah CF, Kofler M, Schiefecker AJ, Beer R, Klug G, Pfausler B, Helbok R. Takotsubo cardiomyopathy in traumatic brain injury. Neurocrit Care. 2017;26(2):284-291.
doi pubmed - Sato R, Nasu M. A review of sepsis-induced cardiomyopathy. J Intensive Care. 2015;3:48.
doi pubmed - Park JH, Kang SJ, Song JK, Kim HK, Lim CM, Kang DH, Koh Y. Left ventricular apical ballooning due to severe physical stress in patients admitted to the medical ICU. Chest. 2005;128(1):296-302.
doi pubmed - Abraham J, Mudd JO, Kapur NK, Klein K, Champion HC, Wittstein IS. Stress cardiomyopathy after intravenous administration of catecholamines and beta-receptor agonists. J Am Coll Cardiol. 2009;53(15):1320-1325.
doi pubmed - Kassim TA, Clarke DD, Mai VQ, Clyde PW, Mohamed Shakir KM. Catecholamine-induced cardiomyopathy. Endocr Pract. 2008;14(9):1137-1149.
doi pubmed - Ako J, Sudhir K, Farouque HM, Honda Y, Fitzgerald PJ. Transient left ventricular dysfunction under severe stress: brain-heart relationship revisited. Am J Med. 2006;119(1):10-17.
doi pubmed - Paur H, Wright PT, Sikkel MB, Tranter MH, Mansfield C, O’Gara P, Stuckey DJ, et al. High levels of circulating epinephrine trigger apical cardiodepression in a beta2-adrenergic receptor/Gi-dependent manner: a new model of Takotsubo cardiomyopathy. Circulation. 2012;126(6):697-706.
doi pubmed - Madhavan M, Borlaug BA, Lerman A, Rihal CS, Prasad A. Stress hormone and circulating biomarker profile of apical ballooning syndrome (Takotsubo cardiomyopathy): insights into the clinical significance of B-type natriuretic peptide and troponin levels. Heart. 2009;95(17):1436-1441.
doi pubmed - Prasad A, Lerman A, Rihal CS. Apical ballooning syndrome (Tako-Tsubo or stress cardiomyopathy): a mimic of acute myocardial infarction. Am Heart J. 2008;155(3):408-417.
doi pubmed - Hasdemir C, Vuran O, Yuksel A, Yavuzgil O. Stress cardiomyopathy (Tako-Tsubo) associated with sustained polymorphic ventricular tachycardia. Pacing Clin Electrophysiol. 2013;36(4):e111-114.
doi pubmed - Bonello L, Com O, Ait-Moktar O, Theron A, Moro PJ, Salem A, Sbragia P, et al. Ventricular arrhythmias during Tako-tsubo syndrome. Int J Cardiol. 2008;128(2):e50-53.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


