| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 8, Number 5, May 2017, pages 159-162
Sneezing: A Rare Cause of Sacral Insufficiency Fracture in a Young Osteoporotic Woman
Yusuf Erdema, b, Cagri Neyiscia
aOrthopedics and Traumatology Department, Gulhane Training and Research Hospital, Ankara, Turkey
bCorresponding Author: Yusuf Erdem, Orthopedics and Traumatology Department, Gulhane Training and Research Hospital, Ankara, Turkey
Manuscript accepted for publication April 18, 2017
Short title: Sacral Osteoporotic Fracture
doi: https://doi.org/10.14740/jmc2810w
| Abstract | ▴Top |
Sacral insufficiency fractures are rare and usually overlooked in patients presenting with low back pain without any trauma. The history and physical examination are not specific, and conventional radiographs are inadequate, thus requiring further radiological imaging as MRI, bone scintigraphy and CT. The treatment includes rest, pain control and physiotherapy. In this report, sneezing is stated as the cause of sacral insufficiency fracture in a young osteoporotic woman.
Keywords: Sneezing; Sacral insufficiency fracture; Osteoporosis; Young
| Introduction | ▴Top |
Sacral insufficiency fractures (SIFs) are a well-defined subgroup of insufficiency fractures and most commonly seen in the elderly, particularly without a history of trauma. The incidence of SIFs is still unknown, but it is clear that SIFs are more common than estimated. The most common cause is postmenopausal osteoporosis [1, 2]. Osteoporotic SIFs are rare and may present with symptoms similar to those low back and sciatic pain. Corticosteroid use, radiotheraphy, rheumatoid arthritis, long-term use of bisphosphonates, renal osteodystrophy, Paget disease, osteomalacia, hyperparathyroidism, and pilimary bilier cirrhosis are reported as the other risk factors [2, 3].
The purpose of this paper was to report an SIF in a young lady who was followed for years with a diagnosis of idiopathic primary osteoporosis. To our knowledge, this is the first report in the evidence-based medical literature of this kind of fracture in a young osteoporotic patient.
| Case Report | ▴Top |
A 29-year-old, 176 cm height and 62 kg weight woman, was admitted to outpatient clinic with low back pain, on the left side, radiating to the gluteus region and posterior surface of the proximal thigh which began suddenly after sneezing 4 days ago. There was no history of trauma. The patient was diagnosed idiopathic primary osteoporosis 5 years ago; however, she did not take bisphosphonates, but was given only supplemental calcium (2,000 mg/day) and vitamin D (400 IU/day) since the initial diagnosis. The recent bone mineral density (BMD) of the lumbar vertebra (L1-L4) was assessed in the “hip” and “spine” programs. The spine T-score was -2.7, and the hip T-score was -2.1. When we examined the reason why the doctor did not prescribe bisphosphonates, the use of bisphosphonates was considered early for such a young lady.
At the physical examination, palpation over the left buttock was painful, and the hip range of motion (ROM) was normal but little painful. Global palpation of the left sacroiliac joint region was also painful, however with no spesific point being found. The sacroiliac compression test was positive on the left side, whereas the Lasegue maneuver was negative bilaterally. She had an antalgic gait with pain on left side which she had never previously suffered. Neurological examination revealed no abnormality.
Plain radiographs of the thoracolumbar, lumbosacral and pelvis showed no osseos pathology (Fig. 1). Magnetic resonance imaging (MRI) revealed a vertically oriented fracture line on the left side of the iliac ala, with prominent bone marrow edema at T2 sequence, characterizing a stress fracture (Fig. 2).
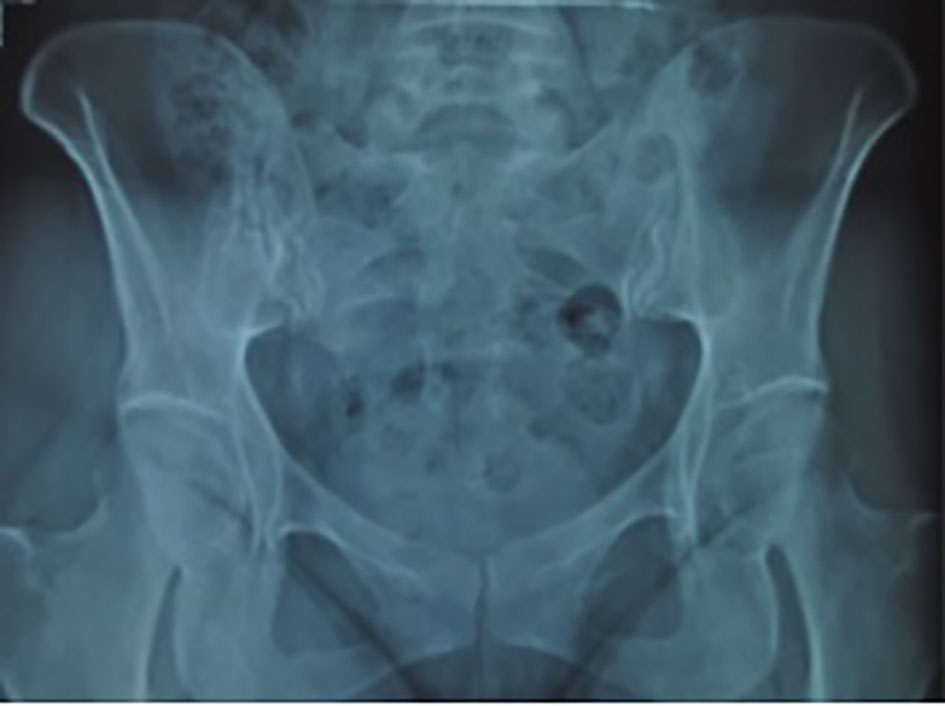 Click for large image | Figure 1. Anteroposterior pelvic radiograph showing no abnormality in the left sacral ala. |
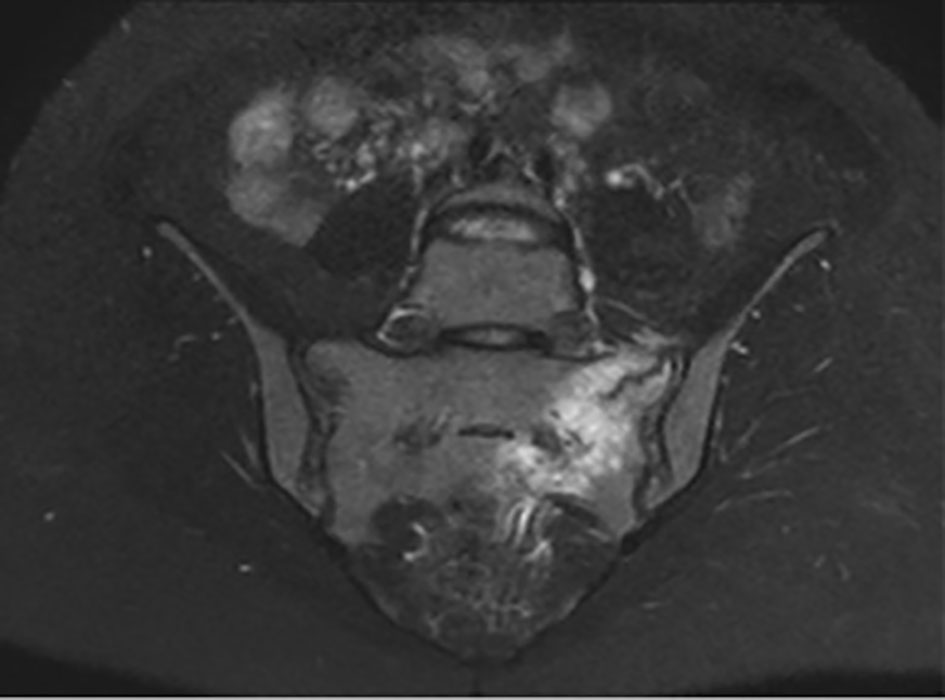 Click for large image | Figure 2. Coronal-sectional MRI of the pelvis showing increased signal intensity of the left sacral ala consistent with a vertical stress fracture in coronal T2 scan. |
Laboratory tests including serum calcium, phosphate, alkaline phosphatase, Vit D, thyroid and parathyroid hormone levels were assessed to compare to initial levels; counterintuitively, we had no data of bone metabolic markers at the time of initiation of osteoporotic treatment. Laboratory results were all normal thus new BMD levels were required, whereas it was expected an increase in biochemical bone turnover markers in such situations.
A diagnosis of a sacral stress fracture was established on the basis of both clinical and radiological tests. Non-steroidal anti-inflammatory drugs were initiated for a week in association with a physiotheraphy programme which was focused on stretching of the posterior thigh, strengthening of the abdominal muscle and core stabilization maneuvers. Though pain was reduced after a week of medication and bed rest, physiotheraphy program lasted 4 weeks. The patient returned to work after 4 weeks of treatment. At the sixth week’s clinical examination, there was no pain on palpation of the left buttock and sacroiliac joint region. Subsequent pelvic radiography and pelvic MRI revealed reduced bone marrow edema and distally healed fracture line (Fig. 3).
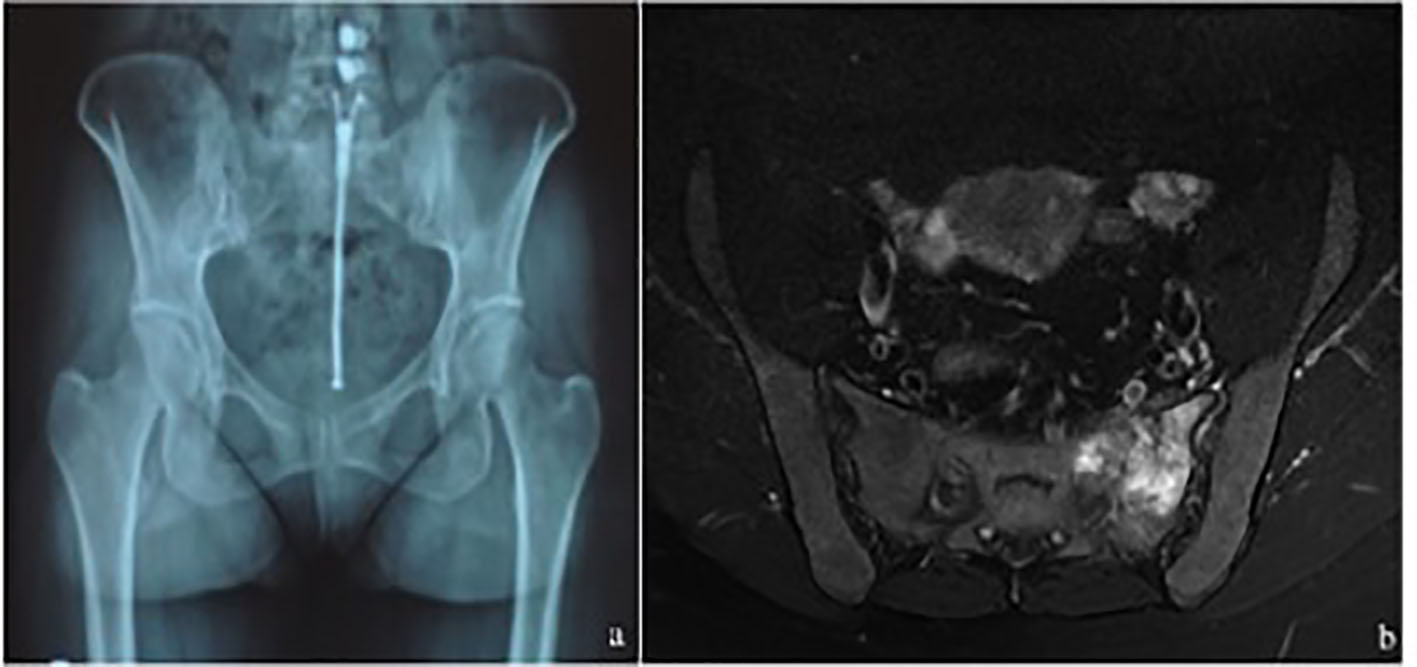 Click for large image | Figure 3. (a) There is no abnormality on the pelvic graph at 1 month. (b) Axial-sectional MRI of the pelvis at 1 month showing reduced signal intensity in left sacral ala with distally healed fracture line. |
| Discussion | ▴Top |
Pentecost et al have classified sacral stress fractures into two groups as fatigue and insufficiency fractures [4]. Fatigue fractures occur in healthy bones under abnormal stresses, while the latter occurs in weakened bones under normal stresses. Sacral stress fractures are mostly seen in athletes, especially long-distance runners, due to unusual loads with repetitive activity [5].
Sacral fatigue fractures have been reported in athletes and during postpartum and intrapartum periods most of which were related to excessive weight gain, hyperlordosis, pelvic ligament weakness and osteopenia during pregnancy, whereas insufficiency fractures have been mostly reported in the elderly postmenopausal osteoporotic patients [5, 6].
The common underlying cause of the SIFs is osteoporosis. Osteoporosis mostly affects trabecular bone than cortical bone where the ratio of trabecular bone is highest in the sacral ala. Additionally osteoporosis lowers bone strength, thus resulting in greater susceptibility to injury with normal repetitive activites and minor traumas. Hence, the stress on the weight-bearing bones such as vertebral bodies, pelvis and sacrum is particularly affected as insufficiency fractures [7, 8].
Moreover, the clinical presentation is often variable and considered to be an acute low back pain. Patients usually present with insidious low back pain which is exacerbated by weight-bearing activities and improved with rest. Back pain may radiate to the gluteal region, hips and lower extremities which may be confused with spinal stenosis and lumbar disc herniations [9]. However, neurological symptoms are generally absent.
In initial anamnesis, patients’ activity levels related to trauma and any relevant risc factors (e.g. osteoporosis, prolonged corticosteroid use, cancer or rheumatlogical disease) should be questioned. Physical examination may reveal sacral tenderness on lateral compression and sacroiliac joint tests. Patients have usually antalgic and slow gate pattern.
In laboratory assessment, at first a slightly raised bone alkaline phosphatase (ALP) as a bone formation marker can be valuable adjunct in directing the clinican towards a diagnosis of SIFs in the beginning period of the sympyoms. Then urine cross-linked N-telopeptides of type 1 collagen, cross-linked C-telopeptides of type 1 collagen can be detected in urine [2].
Conventional radiographs are usually inadequate to demonstrate the SIFs due to many reasons as overlying gas shadows, fecal matter and geometry of the sacrum [10]. MRI is the by far most sensitive diagnostic method. Low signal intensity at T1 and high signal intensity at T2-weighted sequences demonstrate the edema at the fracture line. Further investigation can be achieved with intravenous gadolinium if needed [11]. Moreover, CT and bone scintigraphy can be performed in differential diagnosis. In our case, MRI helped us to understand the nature of the fracture pattern, thus confirming the diagnosis.
Treatment of SIFs is generally conservative. Rest, short-term pain control with analgesics and allowing partial weight-bearing are the first choices, whereas stretching of the posterior thigh, strengthening of the abdominal muscle and core stabilization maneuvers regarding early rehabilitation should be applied as much as can be tolerated by patient. Refractory cases may require more rest and follow-up imaging [12, 13]. Surgical intervention is only needed when the conservative treatment fails or in case of a pelvic instability. Rishi et al reported a case of rheumatoid patient who has an unstable sacral insufficiency with translation at sacroiliac joint treated with in situ iliosacral screw fixation. In this report, it is emphasized that early intervention in such cases should be managed by surgical fixation [14].
On the contrary, management of osteoporosis in young premenopausal women should focus on the treatment of any secondary cause such as weight-bearing exercise, calcium and vitamin D intake, and avoidance of tobacco and alcohol [15]. However, in a situation of major fracture due to osteoporosis, pharmacological therapy is required. Biphosphonates are usually preferred for the first choice of treatment, whereas they should be avoided in women of childbearing potential not to have adverse effects on the fetal skeleton [16, 17]. Selective estrogen receptor agonists are not recommended in young women due to bone loss. On the other hand, teriparatide use is recommended in such cases in many recent literatures [18]. Any fracture history was not reported in this case before, only intake of calcium and vitamin D has been hitherto applied. The patient should take pharmacological therapy from now on.
In conclusion, clinicians should suspect a possible SIF in differential diagnosis of osteoporotic patient with low back and buttock pain even in young patients without any trauma. Low back pain exaggerated by long-term activities and even sneezing as in our case should not be overlooked in the anamnesis; otherwise non-specific symptoms may delay the diagnosis which improves the disability by dislocating the fracture line.
Conflicts of Interest
The authors declare that there are no conflicts of interest regarding the publication of this article.
Funding
No funds have been received for this study.
Consent
Informed consent was obtained from the patient to present and publish the medical documents.
| References | ▴Top |
- Silva RT, De Bortoli A, Laurino CF, Abdalla RJ, Cohen M. Sacral stress fracture: an unusual cause of low back pain in an amateur tennis player. Br J Sports Med. 2006;40(5):460-461.
doi pubmed - Tsiridis E, Upadhyay N, Giannoudis PV. Sacral insufficiency fractures: current concepts of management. Osteoporos Int. 2006;17(12):1716-1725.
doi pubmed - Ayanaoglu T, Atik OS, Tokgoz N, Ucar M. Sacral and pubic insufficiency fractures due to bisphosphonate treatment. Eklem Hastalik Cerrahisi. 2015;26(2):120-124.
doi pubmed - Pentecost RL, Murray RA, Brindley HH. Fatigue, Insufficiency, and Pathologic Fractures. JAMA. 1964;187:1001-1004.
doi pubmed - Giannoulis DK, Koulouvaris P, Zilakou E, Papadopoulos DB, Lykissas MG, Mavrodontidis AN. Atraumatic Sacral Fracture in Late Pregnancy: A Case Report. Global Spine J. 2015;5(3):248-251.
doi pubmed - Speziali A, Tei MM, Placella G, Chillemi M, Cerulli G. Postpartum Sacral Stress Fracture: An Atypical Case Report. Case Rep Orthop. 2015;2015:704393.
doi - Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res. 2007;22(3):465-475.
doi pubmed - Linstrom NJ, Heiserman JE, Kortman KE, Crawford NR, Baek S, Anderson RL, Pitt AM, et al. Anatomical and biomechanical analyses of the unique and consistent locations of sacral insufficiency fractures. Spine (Phila Pa 1976). 2009;34(4):309-315.
doi pubmed - Baldwin MJ, Tucker LJ. Sacral insufficiency fractures: a case of mistaken identity. Int Med Case Rep J. 2014;7:93-98.
doi pubmed - Southam JD, Silvis ML, Black KP. Sacral stress fracture in a professional hockey player: a case report. Orthopedics. 2010;33(11):846.
doi - Ahovuo JA, Kiuru MJ, Visuri T. Fatigue stress fractures of the sacrum: diagnosis with MR imaging. Eur Radiol. 2004;14(3):500-505.
doi pubmed - Askin A, Korkmaz M, Bayram K, Kocyigit H, Demirdal S, Kizilay A, Tosun O. Atypical Sacral And Iliac Bone Insufficiency Fractures In A Patient Receiving Long-Term Bisphosphonate Therapy. Turkish Journal of Geriatrics. 2015;18(2):171-175.
- Lee YJ, Bong HJ, Kim JT, Chung DS. Sacral insufficiency fracture, usually overlooked cause of lumbosacral pain. J Korean Neurosurg Soc. 2008;44(3):166-169.
doi pubmed - Thakral R, Patrick JK, Mahalingham K. Unstable pelvic insufficiency fracture of the pelvis in rheumatoid arthritis patient: evaluation and treatment. Eur J Orthop Surg Traumatol. 2010;20:237-240.
doi - Cohen A, Shane E. Treatment of premenopausal women with low bone mineral density. Curr Osteoporos Rep. 2008;6(1):39-46.
doi pubmed - Vehmanen L, Elomaa I, Blomqvist C, Saarto T. Tamoxifen treatment after adjuvant chemotherapy has opposite effects on bone mineral density in premenopausal patients depending on menstrual status. J Clin Oncol. 2006;24(4):675-680.
doi pubmed - Cohen A. Should bisphosphonates be used in premenopausal women? Maturitas. 2010;66(1):3-4.
doi pubmed - Cohen A, Stein EM, Recker RR, Lappe JM, Dempster DW, Zhou H, Cremers S, et al. Teriparatide for idiopathic osteoporosis in premenopausal women: a pilot study. J Clin Endocrinol Metab. 2013;98(5):1971-1981.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


