| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 2, Number 4, August 2011, pages 169-171
Listening to Heart Rate for Myocardial Ischemic Site
Tatsuya Kawasakia, d, Akihiro Azumab, Toshiro Kuribayashic, Hiroki Sugiharaa
aDepartment of Cardiology, Matsushita Memorial Hospital, Osaka, Japan
bAzuma Hospital, Chiba, Japan
cKuribayashi Clinic of Cardiology, Fukuoka, Japan
dCorresponding author: Department of Cardiology, Matsushita Memorial Hospital, Sotojima 5-55, Moriguchi, Osaka 570-8540, Japan
Manuscript accepted for publication March 25, 2011
Short title: Listening to Heart Rate
doi: https://doi.org/10.4021/jmc241e
| Abstract | ▴Top |
We describe a 63-year-old woman with severe stenosis in the right coronary artery. During the recovery phase of exercise testing, the monitor sound of heart rate changed rhythmically in a delicate fashion. Heart rate variability analysis revealed the association of the rhythm fluctuation with transient vagal enhancement. This phenomenon is known as Bezold-Jarisch reflex, which has been explained by the preferential distribution of cardiac receptors along afferent vagal pathways in the inferior wall of the left ventricle. After coronary angioplasty, the examiner could not notice the fluctuation of heart rate during the recovery phase of a restudy of exercise testing. Listening to heart rate fluctuation during exercise testing, although it may be rare, possibly helps examiners to estimate the site of ischemia to be in the inferior myocardium.
Keywords: Heart rate; Vagus nerve; Ischemia; Inferior wall; Bezold-Jarisch reflex
| Introduction | ▴Top |
ST-segment depression during exercise testing is a simple and useful noninvasive indicator of myocardial ischemia in coronary heart disease, but it cannot provide reliable information as to the site of myocardial ischemia [1]. We present a patient with angina pectoris, in whom listening to the monitor sound of heart rate during exercise testing helped examiners to estimate the site of ischemia.
| Case Report | ▴Top |
A 63-year-old woman was referred to our hospital because of chest discomfort on exertion. Her symptoms had begun 3 months before and worsened gradually, often occurred during jogging early in the morning, and resolved within a few minutes after the cessation of exercise. She had hypertension, well controlled with Ca-antagonist and diuretics. She was a lifelong non-smoker and had no other coronary risk factors, e.g., diabetes mellitus or dyslipidemia.
On admission, blood pressure and heart rate were normal. Physical examinations, electrocardiogram, chest radiograph, and echocardiogram were unremarkable. She underwent an exercise testing using a supine bicycle ergometer after all medications were withdrawn. The exercise workload began with 25 watts and was increased by 25 watts every 2 minutes. At the stage of 75 watts she complained of chest discomfort along with ST-segment depression of 0.15 mV in leads V5 and V6, blood pressure of 210/94 mmHg, and heart rate of 117 beats per minute. The exercise was finished after 1 minute cool-down period maintained at exercise grade of 30 watts. After the peak workload was achieved, heart rate decreased gradually and her symptoms disappeared soon. The examiner noticed during the recovery phase that the monitor sound of heart rate was not regular but changed rhythmically in a delicate fashion; heart rate slowed down slightly and restored in a few seconds. The rhythm fluctuation, persisting several minutes, was not an expression of an established arrhythmia visually on the electrocardiographic monitor. Coronary angiograms showed severe stenosis in the middle portion of right coronary artery. After coronary angioplasty by means of coronary stent implantation, she had been free from chest symptoms. Half a year later, she underwent coronary angiogram, showing neither in-stent restenosis nor de novo lesion. During a restudy of exercise testing under the same condition, she attained the stage of 75 watts without any chest symptoms or ST-segment depression. Unlike exercise testing 6 months before, the examiner could not notice the fluctuation of heart rate during the recovery phase.
To examine the influence of autonomic nerve activity on the heart rate fluctuation, RR intervals were sampled at a frequency of 500 Hz and heart rate variability was analyzed using the archived data during exercise testing before and after coronary intervention. High frequency component (HF, 0.15 - 0.40 Hz) and the coefficient of HF component variance (CCVHF), which is the square root of HF divided by the mean RR interval, were used in the estimation of vagal modulation from short-duration recordings [2, 3]. In the present case, HF and CCVHF before angioplasty reached the minimum already 2 minutes before the peak exercise and peak heart rate, and increased thereafter (Fig. 1, arrow heads), indicating transient vagal enhancement during the recovery phase. This unique response after exercise was not recognized after angioplasty.
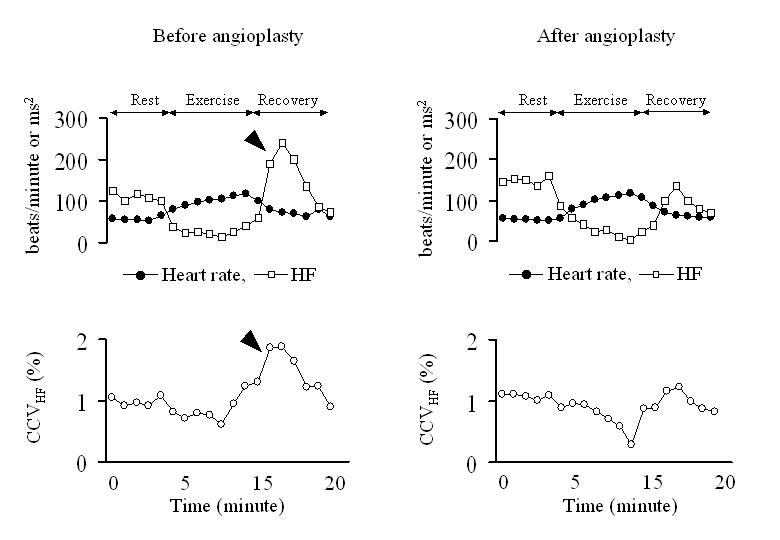 Click for large image | Figure 1. High frequency (HF) and coefficient of high frequency component variance (CCVHF), indexes of vagal activity, transiently increased during the recovery phase before angioplasty (arrow heads), with the unique increment being unclear after angioplasty. |
| Discussion | ▴Top |
Acute inferior myocardial infarction often provokes transient bradycardia and hypotension. This phenomenon is known as Bezold-Jarisch reflex, which has been explained by the preferential distribution of cardiac receptors along afferent vagal pathways in the inferior wall of the left ventricle [4]. We previously reported that the vagal modulation as assessed by HF and CCVHF was enhanced through exercise-induced myocardial ischemia of the inferoposterior myocardium [5]. Thus, in the present case, the combination of vagal enhancement provoked by exercise-induced inferior ischemia and sustainment of sympathetic activation after exercise possibly led to audibly perceptible heart rate fluctuation without bradycardia or hypotension.
Miller et al. [6] reported that 7 patients with significant narrowing of the right coronary artery displayed sinus deceleration defined as ≥ 5 beats/min during exercise (possibly leading to the rhythm fluctuation as with our case) in approximately 40,000 consecutive exercise tests. Considering that far more numerous patients with right coronary lesions must have been included in the study by Miller et al. [6], the prevalence of sinus deceleration or the rhythm fluctuation during exercise testing may be very low even in patients with right coronary lesions. The present case indicates that careful listening to heart rate fluctuation during exercise testing may provide additional information, i.e., the site of ischemia, although the fluctuation may not have a high sensitivity for myocardial ischemia of the inferoposterior myocardium.
Conflict of Interest
None declared.
| References | ▴Top |
- Chaitman BR. Exercise stress testing. In: Zipes DP, Libby P, Bonow RO, Braunwald E, eds. Braunwald’s Heart disease: A Textbook of Cardiovascular Medicine 7th ed. Philadelphia: Saunders, 2005:158 .
- Heart rate variability: standards of measurement, physiological interpretation and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology.Circulation. 1996;93(5):1043-1065.
pubmed - Hayano J, Sakakibara Y, Yamada A, Yamada M, Mukai S, Fujinami T, Yokoyama K, et al. Accuracy of assessment of cardiac vagal tone by heart rate variability in normal subjects. Am J Cardiol. 1991;67(2):199-204.
pubmed doi - Mark AL. The Bezold-Jarisch reflex revisited: clinical implications of inhibitory reflexes originating in the heart. J Am Coll Cardiol. 1983;1(1):90-102.
pubmed doi - Kawasaki T, Azuma A, Kuribayashi T, Taniguchi T, Asada S, Kamitani T, Kawasaki S, et al. Enhanced vagal modulation and exercise induced ischaemia of the inferoposterior myocardium. Heart. 2006;92(3):325-330.
pubmed doi - Miller TD, Gibbons RJ, Squires RW, Allison TG, Gau GT. Sinus node deceleration during exercise as a marker of significant narrowing of the right coronary artery. Am J Cardiol. 1993;71(4):371-373.
doi
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


