| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 2, Number 5, October 2011, pages 197-200
Paraneoplastic Acanthosis Nigricans, Leser-Trélat and Tripe Palms Associated With Gastro-Esophageal Junction Adenocarcinoma: A Case Report
Pieter van Hagena, c, Bas P.L. Wijnhovena, Lizenka A. Torcqueb, Huug W. Tilanusa, J. Jan B van Lanschota, Errol P. Prensb
aDepartment of Surgery, Erasmus University Medical Center Rotterdam, ‘s Gravendijkwal 230, 3015 CE Rotterdam, The Netherlands
bDepartment of Dermatology, Erasmus University Medical Center Rotterdam, ‘s Gravendijkwal 230, 3015 CE Rotterdam, The Netherlands
cCorresponding author: Pieter van Hagen, Department of Surgery, Erasmus University Medical Center Rotterdam,’s Gravendijkwal 230, Room Z-836, 3015 CE Rotterdam, The Netherlands
Manuscript accepted for publication May 11, 2010
Short title: Gastro-Esophageal Junction Adenocarcinoma
doi: https://doi.org/10.4021/jmc217w
| Abstract | ▴Top |
Acanthosis nigricans is a skin condition that is characterized by velvety, hyperpigmented and occasionally pruritic plaques, mostly seen in the flexural areas. It can occur as a paraneoplastic phenomenon, most frequently in association with an adenocarcinoma of gastrointestinal origin. The sign of Leser-Trélat is defined as an eruption of numerous seborrheic keratoses, and can be associated with acanthosis nigricans. Also, acanthosis nigricans can be associated with tripe palms, a velvety, warty thickening of the palms’ surface with exaggerated dermatoglyphics, and with papillomatosis of the oral mucosa. A 62-year old woman presented with a rapid onset of hyperpigmented plaques, multiple (seborrheic) warts, tripe palms and papillomatous hyperplasia of her oral mucosa. A skin biopsy confirmed acanthosis nigricans. Because of her age and the quite sudden development of the skin lesions, the paraneoplastic variant of this condition was suspected and the patient was referred to a medical oncologist. As part of extensive diagnostic screening, an upper gastro-intestinal endoscopy was performed revealing an esophageal tumor at 30 to 35 cm from the incisors. She underwent an esophagectomy after neoadjuvant chemoradiotherapy. The tumor was staged as ypT2N1M0 adenocarcinoma, which had been radically resected (R0). The tumor showed extensive histomorphological regression. During the neoadjuvant therapy the skin lesions and the mucosal swelling with which the patient initially presented regressed, and disappeared almost completely six months after surgery. The presented case shows the combination of acanthosis nigricans, the sign of Leser-Trélat, tripe palms and extensive oral papillomatosis, which led to the detection of an adenocarcinoma of the gastro-esophageal junction, a tumor that has been reported in association with malignant acanthosis nigricans.
Keywords: Acanthosis nigricans; Paraneoplastic syndromes; Esophagogastric junction; Esophageal neoplasms
| Introduction | ▴Top |
Acanthosis nigricans (AN) is a skin disorder that is characterized by velvety, papillomatous, hyperpigmented and occasionally pruritic plaques, mostly seen in the flexural areas. The disorder in itself is benign and associated with insulin resistance, obesity, erythema nodosum and medication (sex hormones, nicotinic acid). AN can also present as a paraneoplastic syndrome and is associated with several malignancies, mostly adenocarcinomas of gastrointestinal origin [1].
AN is most often associated with (distal) gastric cancer, followed by cancers originating from pancreas, ovaries, kidneys, bladder, bronchi, thyroid gland, bile duct and breast. AN is rarely associated with non-epithelial malignancies [2].
In combination with the skin lesions that are typical for AN, the sudden appearance of seborrheic keratosis (the sign of Leser-Trélat) can be seen, resulting in an eruption of multiple seborrheic warts on the trunk. Another skin condition associated with AN is tripe palms, a thickened, velvety, warty surface of the hands with exaggerated dermatoglyphics [3].
Furthermore, AN is the only paraneoplastic syndrome that can involve the oral mucosa, sometimes leading to papillomatosis of the oropharyngeal epithelium [4]. Moreover, multiple wart-like lesions, mostly on the extremities, called florid cutaneous papillomatosis can occur in association with AN. As the paraneoplastic variant of AN frequently has an onset before patients have any other complaints, it is not uncommon that an underlying malignancy is discovered long after AN has been diagnosed [5]. This case report presents the combination of all the paraneoplastic syndromes mentioned above in a patient with a gastro-esophageal junction carcinoma.
| Case Report | ▴Top |
A 62-year-old Caucasian woman presented at the Department of Dermatology with hyperpigmented plaques in the flexural areas (Fig. 1A) and multiple itching, seborrheic verrucous lesions (Fig. 2A) suddenly originating over her entire body. The flexural plaques had been present for less than one year. Furthermore, she noticed a thickening of the surface of her palms with a cobbled appearance. Moreover, she had complaints of a severely swollen oral mucosa, which restricted normal food intake (Fig. 3A).
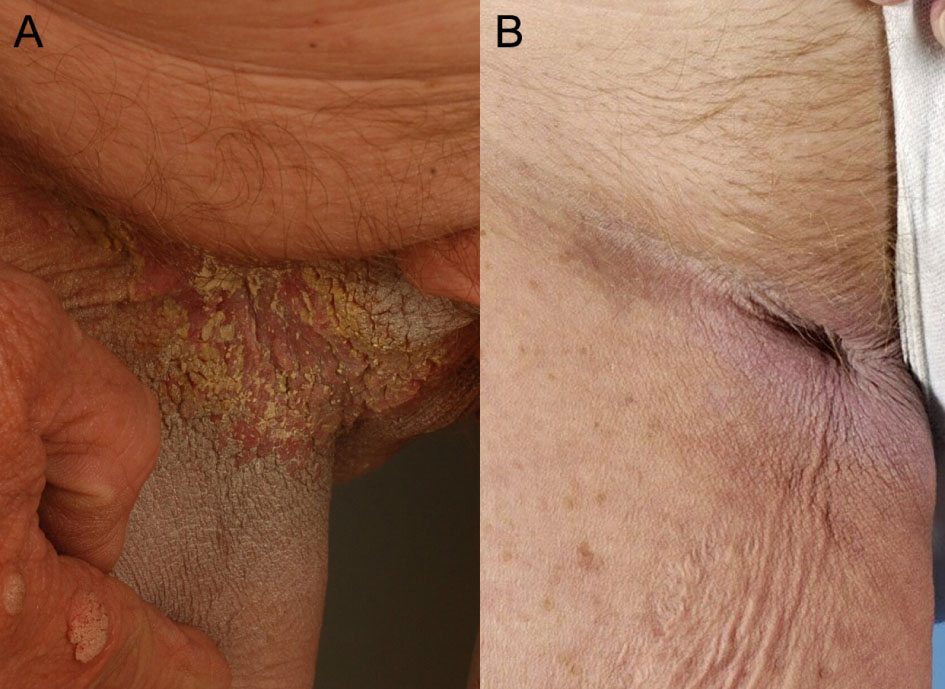 Click for large image | Figure 1. Acanthosis nigricans in the right groin. Typical acanthosis nigricans in the right groin at presentation (A). Regression of acanthosis nigricans, six months after surgery (B). |
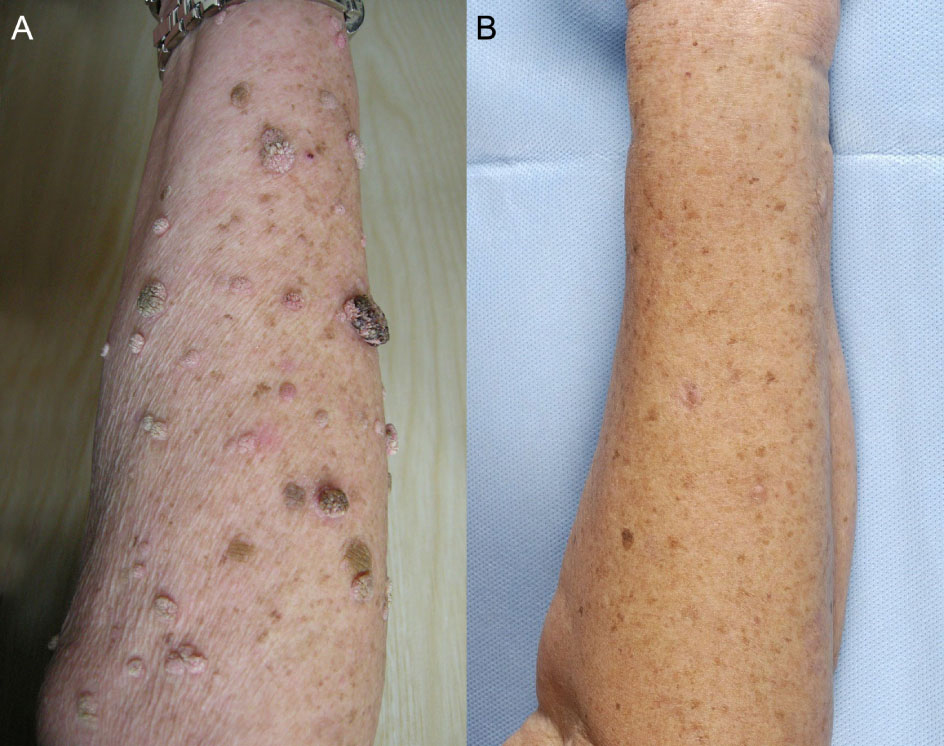 Click for large image | Figure 2. Florid cutaneous papillomatosis on the right arm. Florid cutaneous papillomatosis on the right arm at presentation, showing multiple seborrheic lesions on the skin (A). Almost complete regression, six months after surgery (B). |
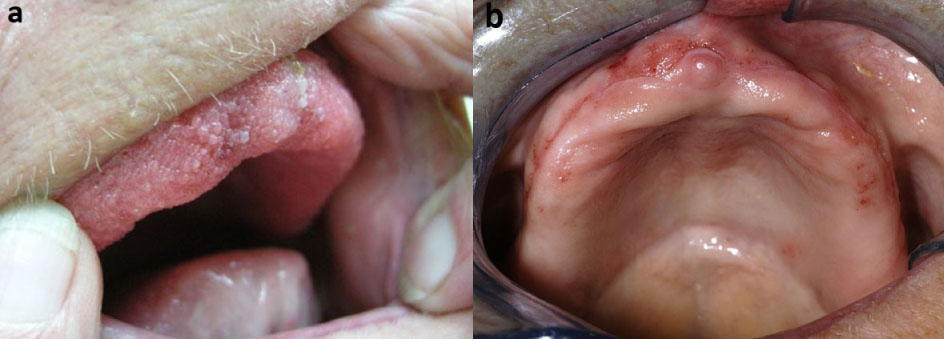 Click for large image | Figure 3. Extensive oral papillomatosis at presentation (A). Almost complete regression, six months after surgery (B). |
Her past medical history consisted of a sliding diaphragmatic hernia, gastro-esophageal reflux disease, diverticulosis of the colon and endometriosis for which a hysterectomy had been performed 30 years earlier. Further history taking revealed that she had complaints of mild dysphagia, weight loss (eight kilograms over the last six months), pyrosis and a highly sensitive scalp, accompanied by hair loss. Her father died of an esophageal carcinoma at age 67. A skin biopsy taken from the left groin area confirmed the suspected diagnosis of acanthosis nigricans (Fig. 4). Because of patient’s age, the sudden onset of her symptoms and the reported weight loss, the paraneoplastic variant of AN was suspected and she was referred to a medical oncologist for further analysis of a possible underlying malignancy.
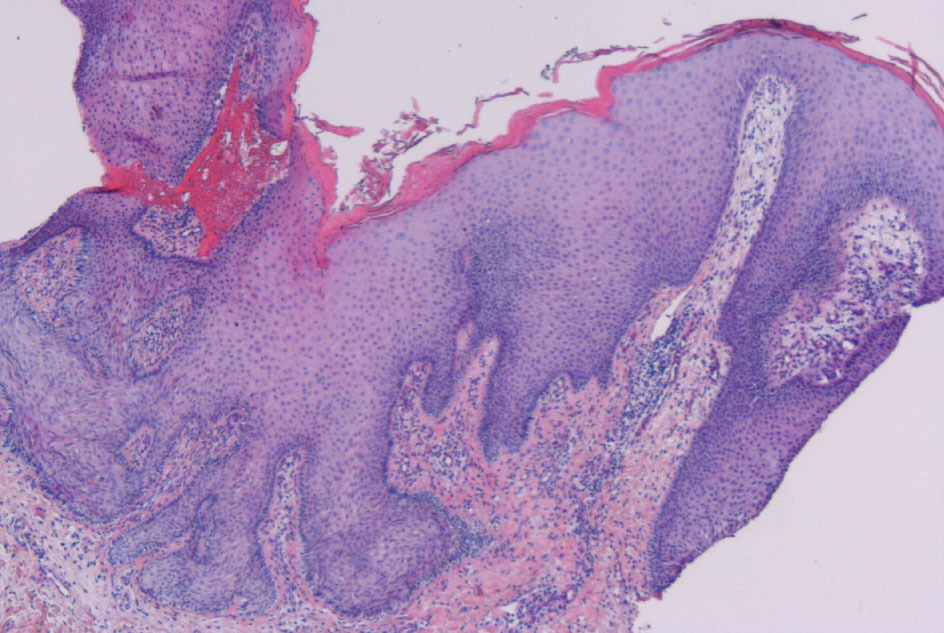 Click for large image | Figure 4. Microscopic image of skin biopsy of the groin. H&E-staining of a biopsy of the groin at presentation, showing acanthosis, slightly irregular epidermal thickening, papillomatosis and inflammation. |
Physical examination showed, apart from the skin-lesions and mucosal papillomatosis as described above, no abnormalities. No lymphadenopathy was present. An upper gastro-intestinal endoscopy was performed, showing a tumor in the distal esophagus, at 30 to 35 cm from the incisors, proximal to a sliding diaphragmatic hernia. No Barrett’s metaplasia was seen. Also, multiple verrucous polyps were seen, spread throughout the esophagus. Biopsies from the tumor and polyps were taken and histopathology revealed a poorly differentiated adenocarcinoma and multiple hyperplastic polyps without dysplasia, respectively. In the tumor cells, no epidermal growth factor receptor expression was found. At endo-ultrasonography, the tumor was staged as uT3N0M0. A CT-scan of neck, chest, and abdomen was performed, showing no additional abnormalities.
After discussion in a multidisciplinary tumor board, the patient underwent neoadjuvant chemotherapy (carboplatin/paclitaxel) with concurrent radiotherapy (41.4 Gy in 23 fractions), followed by a transthoracic esophagectomy with gastric tube reconstruction.
Already during the neoadjuvant chemoradiotherapy, the AN showed clear signs of regression. Apart from a superficial wound infection, the postoperative recovery was uneventful and the patient was discharged on postoperative day 14. Histopathologic examination of the resection specimen showed an ypT2N1M0, poorly differentiated adenocarcinoma (G3) that had been radically removed (R0). After six months of follow-up, the acanthosis nigricans (Fig. 1B), as well as the Leser-Trélat sign (Fig. 2B), the tripe palms, the oral (Fig. 3B) and cutaneous papillomatosis were in complete regression, without any specific dermatological therapy.
| Discussion | ▴Top |
Acanthosis nigricans is a disorder characterized by hyperpigmented, papillomatous, velvety plaques, located in the skin folds. The disorder can be roughly divided into a benign and a paraneoplastic type, which can be distinguished from each other neither by dermatologic investigation nor by histopathologic examination [6]. The benign form is often familial, associated with endocrine pathology (for example insulin resistance or hyperandrogenism) or hormonal substitution therapy but can also be congenital. ‘Malignant’ AN is a paraneoplastic syndrome and not a malignancy in itself. It is not unusual for AN to precede the diagnosis of the primary tumor [5]. If the diagnosis of paraneoplastic AN is not suspected immediately, and a patient is treated as having benign AN, a serious delay in the diagnosis and treatment of the underlying malignancy can occur [1].
Patients presenting with a rapid onset of extensive AN or coexisting unintentional weight loss should be suspected of having paraneoplastic AN. Also, patients who present with AN in combination with the sign of Leser-Trélat, tripe palms or mucosal involvement have a higher risk of having paraneoplastic AN [7]. When paraneoplastic AN is suspected, a wide variety of primary malignancies should be considered. Most common are (distal) gastric carcinomas, but also pancreatic, ovarian, renal and other abdominal carcinomas are common [8]. Patients who are suspected of having paraneoplastic AN should therefore undergo extensive investigations, covering all possible tumors associated with AN, preferably in order of suspicion.
This means that patients should be interviewed extensively about all possible complaints, and that a thorough physical examination should be performed. When after these first investigations a certain malignancy is suspected, this should of course be the focus of further investigation. If, however, a malignancy is not found on the suspected location, investigations should proceed until it is confirmed that on all possible locations where a malignancy could be present, there is none.
In the present case, AN was associated with a GE-junction adenocarcinoma. The present case is especially interesting because AN was associated with the sign of Leser-Trélat and tripe palms and extensive oral papillomatosis. The sign of Leser-Trélat is defined as the appearance of multiple seborrheic verrucous keratoses, and is regularly seen in combination with paraneoplastic AN. It can however also occur without the presence of AN, can be associated with malignant and benign conditions, but has never been reported in combination with benign AN [9, 10]. To our knowledge, the combination of AN, Leser-Trélat, tripe palms plus extensive papillomatosis of the oral mucosa in association with a carcinoma of the gastro-esophageal junction has never been described before.
The pathologic mechanism that causes paraneoplastic AN is unknown. It has been hypothesized that tumor-produced growth factors such as epidermal growth factor, transforming growth factor-α, insulin-like growth factor-1, fibroblast growth factor and melanocyte stimulating hormone-α play a central role [11]. It is believed that when these growth factors are produced by the primary tumor and circulate in large quantities, they can cause epidermal cells to proliferate [11]. Other possibilities, such as a systemic immunologic response to the primary tumor as a cause of the disorder, cannot be discarded.
The optimal treatment of paraneoplastic AN differs between individual cases. Some cases are resistant to any form of therapy, even if the patient is successfully treated for the associated malignancy [12]. Fortunately, in some cases, no separate treatment is needed for AN, as it fully regresses when the associated tumor is effectively treated [7, 13]. This was also the case in the presented patient. However, symptomatic treatment (e.g. anti-pruritic therapy) of the skin lesions can be needed while the patient waits for treatment of the underlying tumor [1]. It has been described that benign AN recurs after the treatment of an underlying endocrine disorder is stopped [14-16]. To our knowledge, no cases of recurrent AN due to a recurrence of the primary tumor have been described. If AN is a general prognosticator for long term survival is unknown. Only in ovarian cancer, it has been described as an indicator of poor prognosis [17].
The esophageal polyps that were found in the present case, could be considered as another expression of AN, which has been described previously [18]. Also, the hair loss from which the patient suffered has been described in literature as an accompanying symptom of AN [4].
The present case shows the rare combination of acanthosis nigricans, sudden appearance of seborrheic keratosis with verrucae (the sign of Leser-Trélat), tripe palms and extensive oral and cutaneous papillomatosis, which led to the diagnosis of (asymptomatic) cancer at the gastro-esophageal junction, a tumor that is rarely associated with paraneoplastic AN. A patient over 40 years old presenting with sudden onset of AN should always be suspected of having paraneoplastic AN, especially when AN is accompanied with the sign of Leser-Trélat, tripe palms and/or oral papillomatosis. When a patient is suspected of having paraneoplastic AN, extensive investigation should take place to find a possible underlying malignancy.
Acknowledgments
PvH, BW, LT, HT, JvL and EP wrote and/or revised the manuscript. PvH, LT and EP provided the clinical data and the photographs. There is no grant support.
Conflicts of Interest
The authors declare no conflict of interest. Written informed consent was obtained from the patient for publication of this case report and all accompanying images.
| References | ▴Top |
- Krawczyk M, Mykala-Ciesla J, Kolodziej-Jaskula A. Acanthosis nigricans as a paraneoplastic syndrome. Case reports and review of literature. Pol Arch Med Wewn. 2009;119(3):180-183.
pubmed - Curth HO, Hilberg AW, Machacek GF. The site and histology of the cancer associated with malignant acanthosis nigricans. Cancer. 1962;15:364-382.
pubmed - Cohen PR, Grossman ME, Silvers DN, Kurzrock R. Tripe palms and cancer. Clin Dermatol. 1993;11(1):165-173.
pubmed doi - Steen AE, Steen KH, Bieber T. Multiple paraneoplasia in the absence of a detectable tumour. Acta Derm Venereol. 2001;81(2):150-151.
pubmed doi - Odom RB, James WD, Berger TG. Andrews' diseases of the skin : clinical dermatology. 9th ed. Philadelphia: W.B. Saunders, 2000.
- Flier JS. Metabolic importance of acanthosis nigricans. Arch Dermatol. 1985;121(2):193-194.
pubmed doi - Higgins SP, Freemark M, Prose NS. Acanthosis nigricans: a practical approach to evaluation and management. Dermatol Online J. 2008;14(9):2.
pubmed - Rigel DS, Jacobs MI. Malignant acanthosis nigricans: a review. J Dermatol Surg Oncol. 1980;6(11):923-927.
pubmed - Heaphy MR, Jr., Millns JL, Schroeter AL. The sign of Leser-Trelat in a case of adenocarcinoma of the lung. J Am Acad Dermatol. 2000;43(2 Pt 2):386-390.
pubmed doi - Yeh JS, Munn SE, Plunkett TA, Harper PG, Hopster DJ, du Vivier AW. Coexistence of acanthosis nigricans and the sign of Leser-Trelat in a patient with gastric adenocarcinoma: a case report and literature review. J Am Acad Dermatol. 2000;42(2 Pt 2):357-362.
pubmed doi - Koyama S, Ikeda K, Sato M, Shibahara K, Yuhara K, Fukutomi H, Fukunaga K, et al. Transforming growth factor-alpha (TGF alpha)-producing gastric carcinoma with acanthosis nigricans: an endocrine effect of TGF alpha in the pathogenesis of cutaneous paraneoplastic syndrome and epithelial hyperplasia of the esophagus. J Gastroenterol. 1997;32(1):71-77.
pubmed doi - Lenzner U, Ramsauer J, Petzoldt W, Meigel W. Acanthosis nigricans maligna. Case report and review of the literature. Hautarzt. 1998;49(1):41-47.
pubmed - Anderson SH, Hudson-Peacock M, Muller AF. Malignant acanthosis nigricans: potential role of chemotherapy. Br J Dermatol. 1999;141(4):714-716.
pubmed doi - Katz RA. Treatment of acanthosis nigricans with oral isotretinoin. Arch Dermatol. 1980;116(1):110-111.
pubmed doi - Ozdemir M, Toy H, Mevlitoglu I, Demirkesen C. Generalized idiopathic acanthosis nigricans treated with acitretin. J Dermatolog Treat. 2006;17(1):54-56.
pubmed doi - Walling HW, Messingham M, Myers LM, Mason CL, Strauss JS. Improvement of acanthosis nigricans on isotretinoin and metformin. J Drugs Dermatol. 2003;2(6):677-681.
pubmed - Scheinfeld N. A review of the cutaneous paraneoplastic associations and metastatic presentations of ovarian carcinoma. Clin Exp Dermatol. 2008;33(1):10-15.
pubmed - Kozlowski LM, Nigra TP. Esophageal acanthosis nigricans in association with adenocarcinoma from an unknown primary site. J Am Acad Dermatol. 1992;26(2 Pt 2):348-351.
pubmed doi
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


