| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 6, Number 1, January 2015, pages 14-16
Severe Septicemic Melioidosis in a Patient With Lung Adenocarcinoma Following Cytotoxic Chemotherapy
Kuo-Hwa Chianga, c, Kuo-Chen Chenga, Hsi-Hsing Yangb
aDivision of Chest Medicine, Department of Internal Medicine, Chi Mei Medical Center, Tainan, Taiwan
bDepartment of Intensive Care Medicine, Chi Mei Medical Center, Tainan, Taiwan
cCorresponding Author: Kuo-Hwa Chiang, Division of Chest Medicine, Department of Internal Medicine, Chi Mei Medical Center, No. 901, Chun-Hua Rd, Yong Kang Dist., Tainan City 710, Taiwan
Manuscript accepted for publication December 03, 2014
Short title: Melioidosis After Chemotherapy in Lung Cancer
doi: http://dx.doi.org/10.14740/jmc2012w
| Abstract | ▴Top |
Melioidosis is an endemic disease in Southeast Asia and northern Australia, caused by Burkholderia pseudomallei. Severe melioidosis pneumonia is typically life-threatening condition. It is relatively uncommon in patients with lung cancer. We report a case of melioidosis pneumonia with blood culture proved Burkholderia pseudomallei in a patient with advanced stage lung adenocarcinoma following treatment with a gemcitabine containing regimen. To our knowledge, this is the first report on septicemic melioidosis pneumonia in lung adenocarcinoma patients following administration of cytotoxic chemotherapy.
Keywords: Burkholderia pseudomallei; Septicemic melioidosis; Pneumonia; Lung adenocarcinoma; Cytotoxic chemotherapy
| Introduction | ▴Top |
Melioidosis is a disease of public health importance in Southeast Asia and northern Australia, which has the potential for epidemic spread to areas where it is not endemic [1, 2]. Pneumonia is the most common presenting feature of melioidosis, the disease caused by infection with Burkholderia pseudomallei [1, 2]. Melioidosis pneumonia can be the primary presenting feature, can develop secondary to initial illness at a distant site, and can develop in patients with bacteremia without an initial evident focus [3]. Clinical progression of acute melioidosis pneumonia is often rapid, and septic shock and death are common outcomes, while severe septicemic melioidosis pneumonia is typically life-threatening [4]. Conditions predisposing to immunosuppression such as DM, liver cirrhosis, etc., can associate with septicemic melioidosis [4, 5]. Severe septicemic melioidosis following chemotherapy with gemcitabine containing regimen in advanced lung adenocarcinoma patient is extremely rare and has never been reported. We present a case of lung adenocarcinoma who received one course of chemotherapy with gemcitabine and cislatin, and developed life-threatening pneumonia with blood culture proved Burkholderia pseudomallei, while no neutropenia was noted at presentation. The patient was successfully treated with antibiotics treatment.
| Case Report | ▴Top |
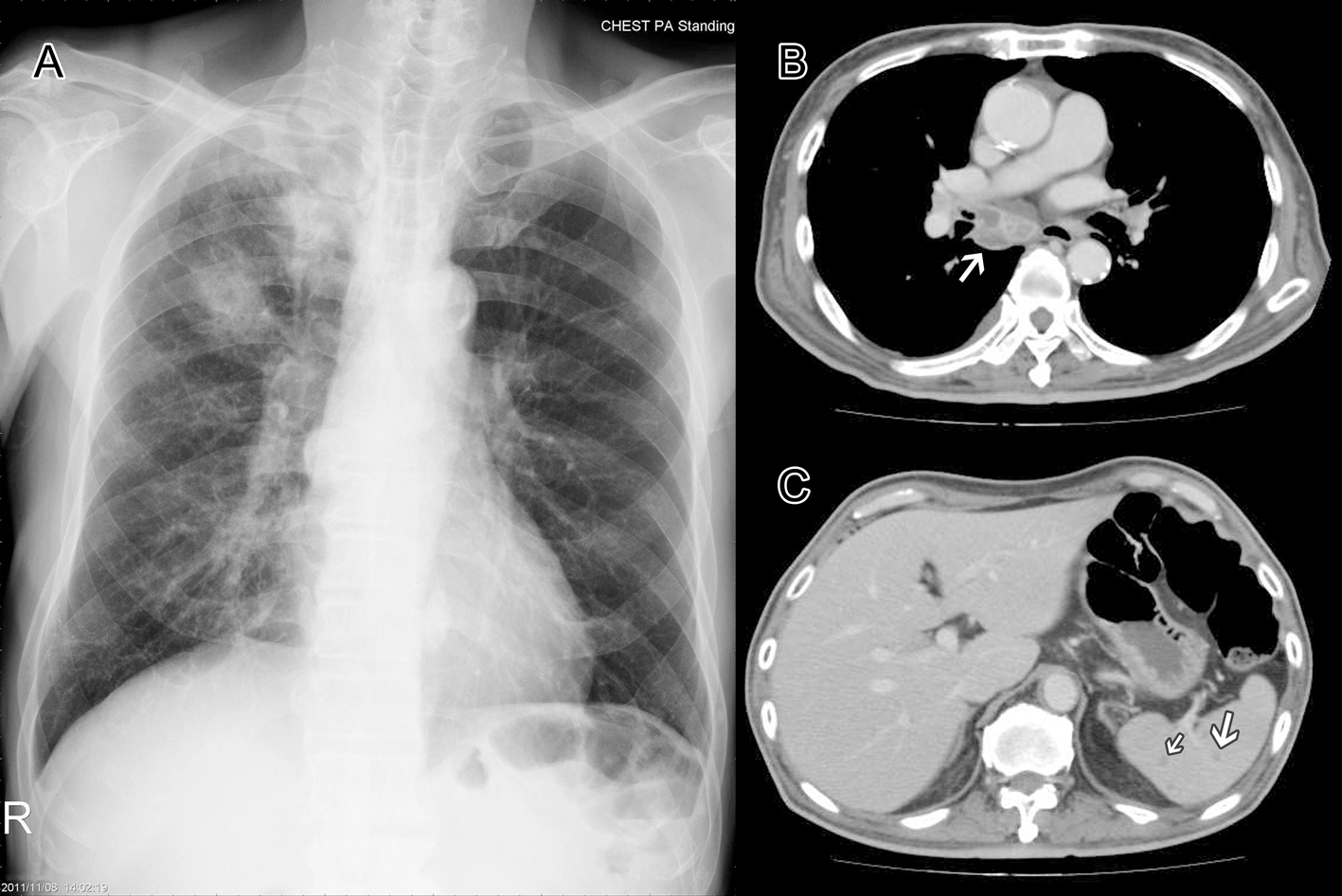
We present a 70-year-old male, who was diagnosed as adenocarcinoma of lung right upper lobe with lung to lung metastasis 2 months prior to this admission, ever received chemotherapy with gemcitabine and cisplatin for one course and was discharged from our center with a stable disease condition, admitted to our ER due to fever, productive cough and progressive shortness of breath for days. The patient denied travelling history, nor contact history of influenza, etc. A complete blood count showed WBC of 11.7 × 103/μ, platelet of 655 × 103/μ, and a chest film showed nodular opacities over right upper lung and infiltrate over right lower lung field (Fig. 1A). A chest CT showed right hilar and mediastinum lymph node enlarged with severe necrotic change (Fig. 1B) and multiple tiny splenic low attenuation lesions (Fig. 1C), more in favor of tumor progression after chemotherapy. However, high fever with chill developed rapidly, a follow-up complete blood count showed leukocytosis with WBC of 17.4 × 103/μ and platelet of 282 × 103/μ, C-reactive protein showed 202 mg/L, the patient developed progressive worsening dyspnea shortly after admission, while an arterial blood gas analysis revealed severe hypoxemia with respiratory acidosis, he then received endotracheal intubation with mechanical ventilation, and transferred to ICU for further intensive care. A series of CXR (Fig. 2) showed progressive change from right upper lung nodular density (Fig. 2A) to right upper lobe consolidation and right lower lobe infiltrate (Fig. 2B) and then rapidly deteriorated to bilateral diffuse infiltrate with ARDS pattern (Fig. 2C). Unexpectedly, the blood culture indicated the presence of a strain of Burkholderia pseudomallei that was susceptible to ceftazidime, imipenem, and minocycline. He received intravenous ceftazidime 2 g every 8 h for 2 weeks, his general condition improved with successful extubated on the eighth ICU day and was transferred to general ward the next day. Then he received antibiotics treatment with ceftazidime 2 g q8h and minocycline 100 mg q12h for additional 3 weeks. His condition improved and the follow-up blood culture showed no growth, while follow-up CXR revealed substantial improvement of the consolidation, and he then was discharged with stable condition. He was keep on oral antibiotic with a combination of doxycycline 100 mg twice a day, trimethoprim/sulfamethoxazole 80 mg/400 mg two tablets twice a day along with target therapy with gefitinib 250 mg qd for his lung adenocarcinoma. The patient condition improved and he completed the antibiotics treatment 20 weeks after discharge, with a smooth and stable disease condition.
| Discussion | ▴Top |
Lung infections can be severe consequences of chemotherapy-induced immune defects. Most of the cases are related to neutropenic condition. During the past decades, the attention in management of infections in cancer patients has focused on fever and neutropenia [6-8]. However, latest guidelines by the National Comprehensive Cancer Network recommend that immunocompromised non-neutropenic cancer patients should receive equal attention as those with neutropenia [9]. Cytotoxic drugs used for the treatment of lung cancer can affect chemotactic and phagocytic function, without reflecting on the total cell count. The functional capabilities of phagocytes such as neutrophils, eosinophils and mononuclear cells may be intrinsically defective even before the initiation of chemotherapy [6].
Severe septicemic melioidosis pneumonia with respiratory failure following administration of cytotoxic chemotherapy in lung adenocarcinoma patient is very rare; to our knowledge, this is the first case in English literature. Patients with septicemic melioidosis pneumonia can present severely unwell with fever and prostration, sometimes with few clinical features to suggest a focus of infection but with chest radiography revealing abnormalities consistent with bacteremic pneumonia, typically multiple nodular opacities or multiple patches of alveolar infiltration [3-5]. These cases often progress rapidly with coalescence of lesions, development of new lesions, and cavitation. Clinical progression of acute melioidosis pneumonia is often rapid, and septic shock and death are common outcomes [3-5]. Acute pneumonia with upper lobe consolidation in endemic regions warrants consideration of melioidosis.
Previous study demonstrated that acute septicemic melioidosis has an upper lobe predominancy in endemic regions, and may be initially misdiagnosed as having tuberculosis [10, 11]. The initial clinical presentations of pulmonary melioidosis can mimic tuberculosis, which exhibits fever, dyspnea, a loss of body weight, and fatigue [10]. It might be difficult to distinguish one from the other, unless microbiological information is confirmed [10, 11]. Previous study demonstrated that multisystemic involvement, particularly multiple splenic abscesses, provides an important clue for melioidosis [12]. However, if the lesion coexists with lung tumor, as in our case, it represents a diagnostic and therapeutic challenge in the course of chemotherapy following diagnosis of lung cancer. In image study of a patient with lung adenocarcinoma under stable disease after chemotherapy, it might be mistakenly diagnosed as progressive disease with multiple spleen metastasis, or hilar lymph node metastasis especially when the melioidosis pneumonia developed initially. It is possible that the Burkholderia pseudomallei infection in our patient was community-acquired, and it is likely that the environment may play a role in Burkholderia pseudomallei infection in cancer patients, even those receiving less toxic chemotherapy. In some endemic area, melioidosis pneumonia should be considered in differential diagnosis of severe pneumonia after cytotoxic chemotherapy. This is a very important lesson in the care and management of patients on chemotherapy. The subtle and complicated nature of the course of this patient merits our emphasis on unusual presentation of severe pneumonia in newly diagnosed lung cancer patient. Physicians should be cautious to differentiate progressive disease or superimposed infection with an unusual presentation of severe community-acquired pneumonia in chemotherapy-treated patients.
Declaration of Interest
We declare no conflict of interest. This article did not receive any funding from any institution.
| References | ▴Top |
- Currie BJ. Melioidosis: an important cause of pneumonia in residents of and travellers returned from endemic regions. Eur Respir J. 2003;22(3):542-550.
doi pubmed - White NJ. Melioidosis. Lancet. 2003;361(9370):1715-1722.
doi - Meumann EM, Cheng AC, Ward L, Currie BJ. Clinical features and epidemiology of melioidosis pneumonia: results from a 21-year study and review of the literature. Clin Infect Dis. 2012;54(3):362-369.
doi pubmed - Cheng AC, Currie BJ. Melioidosis: epidemiology, pathophysiology, and management. Clin Microbiol Rev. 2005;18(2):383-416.
doi pubmed - Chan KP, Low JG, Raghuram J, Fook-Chong SM, Kurup A. Clinical characteristics and outcome of severe melioidosis requiring intensive care. Chest. 2005;128(5):3674-3678.
pubmed - Aliberti S, Myers JA, Peyrani P, Blasi F, Menendez R, Rossi P, Cosentini R, et al. The role of neutropenia on outcomes of cancer patients with community-acquired pneumonia. Eur Respir J. 2009;33(1):142-147.
doi pubmed - Vento S, Cainelli F, Temesgen Z. Lung infections after cancer chemotherapy. Lancet Oncol. 2008;9(10):982-992.
doi - Yoo SS, Cha SI, Shin KM, Lee SY, Kim CH, Park JY, Jung TH. Bacterial pneumonia following cytotoxic chemotherapy for lung cancer: clinical features, treatment outcome and prognostic factors. Scand J Infect Dis. 2010;42(10):734-740.
doi pubmed - National Comprehensive Cancer Network. Prevention and treatment of cancer-related infections. 2007. www.nccn.org/about/newsinfo.asp?newsID =107.
- Chou DW, Chung KM, Chen CH, Cheung BM. Bacteremic melioidosis in southern Taiwan: clinical characteristics and outcome. J Formos Med Assoc. 2007;106(12):1013-1022.
doi - Mukhopadhyay A, Lee KH, Tambyah PA. Bacteraemic melioidosis pneumonia: impact on outcome, clinical and radiological features. J Infect. 2004;48(4):334-338.
doi pubmed - Muttarak M, Peh WC, Euathrongchit J, Lin SE, Tan AG, Lerttumnongtum P, Sivasomboon C. Spectrum of imaging findings in melioidosis. Br J Radiol. 2009;82(978):514-521.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.