| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 4, Number 11, November 2013, pages 753-757
Cystic Pheochromocytoma Discovered as an Adrenal Incidentaloma
Daisuke Takarabea, e, Yoshihiko Takahashib, Tetsuro Tsujimotoa, Hiroshi Notoa, c, Miyako Kishimotoa, c, Shigeru Minowadad, Mitsuhiko Nodaa, c, f
aDepartment of Diabetes and Metabolic Medicine, National Center for Global Health and Medicine, Tokyo, Japan
bDivision of Diabetes and Metabolism, Iwate Medical University School of Medicine, Morioka, Japan
cDiabetes Research Center, National Center for Global Health and Medicine, Tokyo, Japan
dDepartment of Urology, National Center for Global Health and Medicine, Tokyo, Japan
eDepartment of Endocrinology and Metabolism, Tama-Hokubu Medical Center, Tokyo, Japan
fCorresponding author: Mitsuhiko Noda, Department of Diabetes and Metabolic Medicine, National Center for Global Health and Medicine, Toyama 1-21-1, Shinjuku-ku, Tokyo, 162-8655, Japan
Manuscript accepted for publication September 20, 2013
Short title: Cystic Pheochromocytoma
doi: https://doi.org/10.4021/jmc1610e
| Abstract | ▴Top |
Cystic pheochromocytomas are uncommon. Patients with cystic pheochromocytomas are more likely to be asymptomatic and to have a negative biochemical evaluation than those with classic solid tumors, which may lead to misdiagnosis. We describe herein a case of cystic pheochromocytoma that was discovered as an adrenal incidentaloma. The patient did not have any major symptoms, apart from occasional mild headaches and palpitations at night. Pheochromocytomas should be considered in the differential diagnosis of cystic adrenal lesions.
Keywords: Pheochromocytoma; Adrenal cyst; Cystic pheochromocytoma; Adrenal incidentaloma; Asymptomatic pheochromocytoma
| Introduction | ▴Top |
Cystic adrenal lesions are uncommon and reportedly have an incidence of 0.064-0.18% in autopsy series; about 4-22% of all adrenal incidentalomas are cystic [1]. The majority of previously reported adrenal cysts have been nonfunctioning and asymptomatic [2]. However, a few cases of cystic pheochromocytomas, which are typically solid tumors, have been described [2-10]. We describe herein a case of cystic pheochromocytoma that was discovered as an adrenal incidentaloma. We obtained written informed consent from the patient for this report.
| Case Report | ▴Top |
A right upper abdominal cystic mass was incidentally detected in a 64-year-old woman during an abdominal ultrasonography examination performed as part of a medical checkup. An enhanced computed tomography (CT) scan revealed a round cystic lesion with an enhanced thick wall, approximately 4 cm in diameter, which was located in the right adrenal gland (Fig. 1). The patient had no specific signs or symptoms. Because the previous doctor could not ascertain whether the patient’s adrenal tumor was functioning or malignant, an annual CT scan was recommended to the patient. Thereafter, she was referred to our hospital for a second opinion.
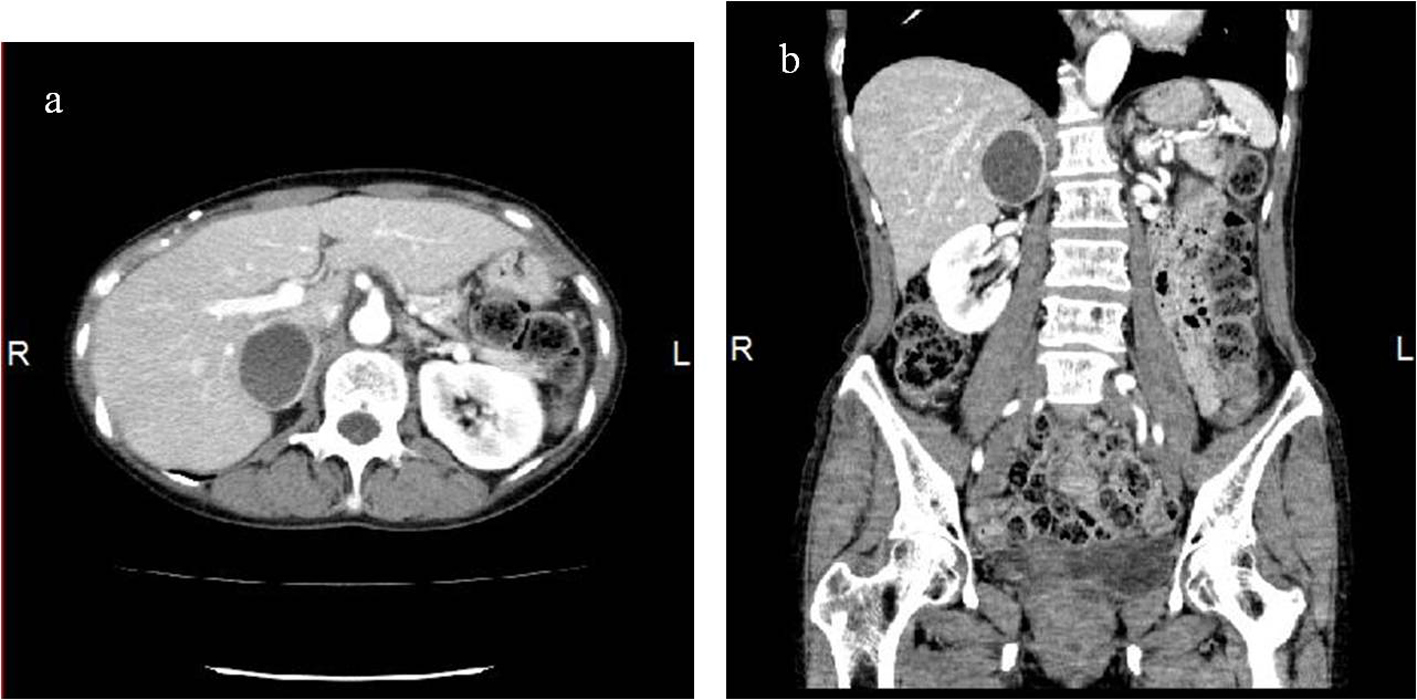 Click for large image | Figure 1. Abdominal CT scan in the axial plane (a) and coronal reconstitution (b). The images show a round cystic lesion with an enhanced thick wall, approximately 4 cm in diameter, in the right adrenal gland. |
The patient had a history of the removal of a pineal tumor and the placement of a ventriculoperitoneal shunt at 63 years of age. She had never been diagnosed as having hypertension, and there was no relevant family history. During a medical review, we noted that the patient had occasional mild headaches and palpitations at night. She was 153.6 cm tall and weighed 43.5 kg, with a body temperature of 36.6°C, a pulse rate of 71 beats per minute, and a blood pressure of 112/65 mm Hg. A physical examination revealed no abnormal findings.
When the patient first came to our hospital, her blood cell count and blood chemistry examination were within the normal ranges (Table 1). Chest X-ray and electrocardiography did not show cardiomegaly or other abnormal findings. A screening hormone test related to the adrenal gland, however, revealed elevated plasma catecholamine levels, epinephrine, 0.41 ng/mL(N: 0.00 - 0.10); norepinephrine, 1.88 ng/mL (N: 0.10 - 0.50). Furthermore, detailed 24-hour urinalyses during hospitalization showed elevated urinary catecholamine levels, epinephrine, 169.3 mg/24 h (N: 3.0 - 41.0); norepinephrine, 697.8 mg/24 h (N: 31.0 - 160.0), metanephrine levels with metanephrine, 1.31 mg/24 h (N: 0.04 - 0.18); normetanephrine, 1.55 mg/24 h (N: 0.10 - 0.28) and vanillylmandelic acid level, 9.84 mg/24 h (N: 1.50 - 4.90) (Table 2). Other hormonal tests, including serum cortisol, plasma aldosterone concentration, plasma renin activity, plasma dehydroepiandrosterone sulfate, serum calcitonin and intact parathyroid hormone, were within the normal ranges (Table 2). Because we suspected that the tumor was a pheochromocytoma, we performed iodine-123 (123I)-labeled metaiodobenzylguanidine (MIBG) scintigraphy as an additional examination to confirm the diagnosis. The results showed the accumulation of 123I-MIBG in the margin of the patient’s right adrenal tumor; no metastatic lesions were detected (Fig. 2). A magnetic resonance imaging (MRI) scan would have been useful to diagnose the mass, but we were unable to perform such an examination because of the possible adverse effect on her ventriculoperitoneal shunt.
 Click to view | Table 1. Laboratory Data |
 Click to view | Table 2. Endocrinological Data |
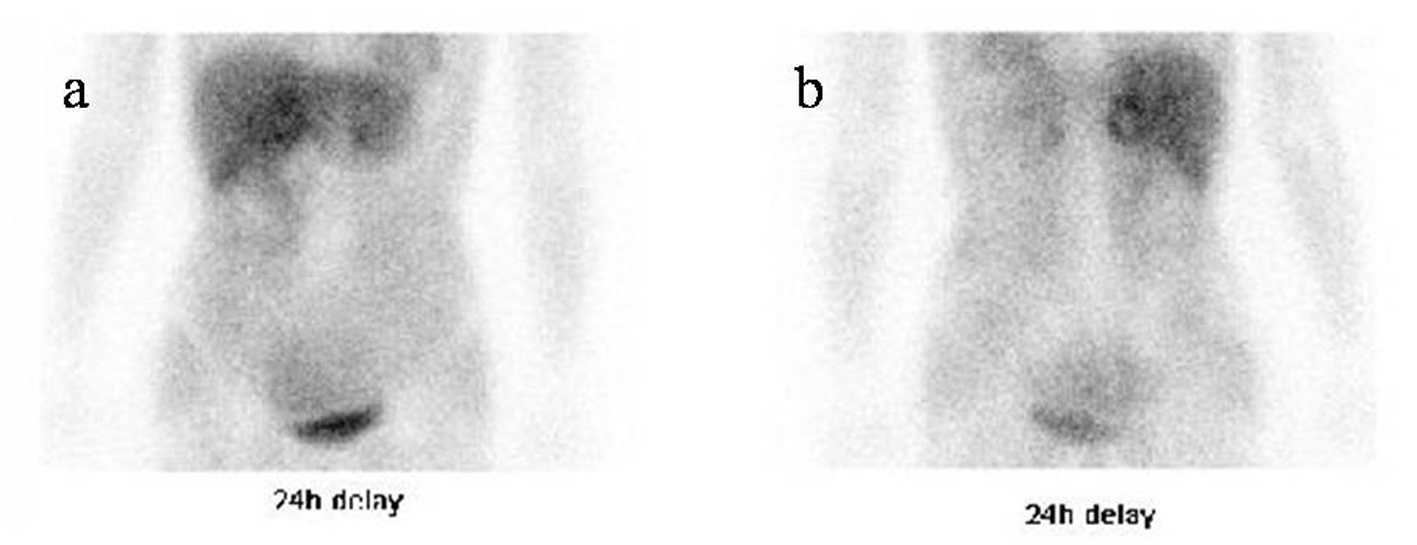 Click for large image | Figure 2. 123I-MIBG scintigraphy images from an anterior view (a) and a posterior view (b), obtained 24 hours after the injection of 123I-MIBG, show a ring-accumulated lesion in the right adrenal gland. |
Based on the findings of the excessive production of catecholamines and the positive result of the 123I-MIBG scintigraphy examination, which has a high specificity (95-100%) [11], we diagnosed the patient’s right adrenal tumor as a pheochromocytoma.
The patient was prescribed a a-adrenergic blocker (prazosin hydrochloride 0.5 mg three times daily) preoperatively. Thereafter, elective surgical removal of the right adrenal tumor was performed without complications, and the postoperative course was uneventful. Macroscopically, the mass was 38 mm × 32 mm × 25 mm, round, well-circumscribed, and encapsulated. It had a central cystic space filled with hemorrhagic fluid, and its marginal thick wall was solid and hemorrhagic (Fig. 3). Histologically, the tumor was confirmed as a pheochromocytoma, and no malignant foci were detected.
 Click for large image | Figure 3. A bisected surgical specimen shows a well-circumscribed mass with a central cystic space containing hemorrhagic fluid and a hemorrhagic thick wall. |
Her plasma and urinary catecholamine levels fell to within the normal ranges soon after the operation. Her daily blood pressure without a-adrenergic blocker decreased from a preoperative value of 110/65 mm Hg to a postoperative value of 100/60 mm Hg, suggesting that her blood pressure was slightly affected by the excessive production of catecholamines, and her mild headache and mild palpitations at night disappeared completely.
| Discussion | ▴Top |
Pheochromocytomas are catecholamine-producing neuroendocrine tumors arising from chromaffin cells of the adrenal medulla, which can cause various signs and symptoms such as headaches, palpitations, sweating, pallor, and hypertension; some patients with pheochromocytomas may, however, be normotensive and asymptomatic [11]. Cystic pheochromocytoma is rare, and its formation process might be intralesional hemorrhage, necrosis, and liquefaction. Patients with cystic pheochromocytomas are more likely to be asymptomatic and to have a negative biochemical evaluation than those with solid tumors [4, 5], which may lead to misdiagnosis. The reason why the present patient had no specific signs or symptoms despite the elevated levels of plasma catecholamines is unclear. However, it may be that the active catecholamines are converted into inactive metabolites within the tumor, and baroreceptor function decreases with age [12]. Although previous reports suggest that cystic or incidental pheochromocytoma may have non-specific abdominal symptoms [4, 12], the present patient did not have any such symptoms.
CT and MRI are commonly used modalities for studying the adrenal gland. Although the present patient had no hypertensive episode after an enhanced CT scan in medical checkup, it is well known that iodinated contrast media are associated with the risk of a hypertensive crisis and are essentially contraindicated for patients suspected of having pheochromocytoma. The typical imaging characteristics of pheochromocytoma are a round or oval, well-circumscribed, homogeneous or heterogeneous soft-tissue mass measuring over 3 cm, increased attenuation on unenhanced CT, prominent vascularity of the mass, delayed washout of contrast media, and an high signal intensity on T2-weighted MRI [3, 8]. In contrast, the CT features of cystic pheochromocytomas have been reported to be a relatively thick wall, the presence or absence of septa within the mass, and with persistent wall enhancement after the administration of contrast media [4], which is compatible with the findings in the present patient.
The surgical indications for the removal of an incidentally discovered adrenal mass have been published [13], but the indications for the surgical resection of purely cystic adrenal masses are less clear [9]. Unless surgically removed, pheochromocytomas can lead to hypertensive crises and several cardiovascular complications [4]. Therefore, surgical excision is thought to be the most definitive treatment of pheochromocytomas regardless of whether the tumor is cystic or not.
In conclusion, pheochromocytomas should be considered in the differential diagnosis of cystic adrenal lesions, even those with nonspecific signs or symptoms, and we recommend that endocrinological examinations and 123I-MIBG scintigraphy or MRI be added when performing a differential diagnosis. If a pheochromocytoma is diagnosed, surgical excision should be considered as the primary treatment to avoid any potential hypertensive crises and a variety of cardiovascular complications.
| References | ▴Top |
- Bellantone R, Ferrante A, Raffaelli M, Boscherini M, Lombardi CP, Crucitti F. Adrenal cystic lesions: report of 12 surgically treated cases and review of the literature. J Endocrinol Invest. 1998;21(2):109-114.
pubmed - Pradeep PV, Mishra AK, Aggarwal V, Bhargav PR, Gupta SK, Agarwal A. Adrenal cysts: an institutional experience. World J Surg. 2006;30(10):1817-1820.
doi pubmed - Munden R, Adams DB, Curry NS. Cystic pheochromocytoma: radiologic diagnosis. South Med J. 1993;86(11):1302-1305.
doi pubmed - Andreoni C, Krebs RK, Bruna PC, Goldman SM, Kater CE, Alves MT, Ortiz V. Cystic phaeochromocytoma is a distinctive subgroup with special clinical, imaging and histological features that might mislead the diagnosis. BJU Int. 2008;101(3):345-350.
doi pubmed - Erem C, Kocak M, OnderErsoz H, Ersoz S, Yucel Y. Epinephrine-secreting cystic pheochromocytoma presenting with an incidental adrenal mass: a case report and a review of the literature. Endocrine. 2005;28(2):225-230.
doi - Erickson LA, Lloyd RV, Hartman R, Thompson G. Cystic adrenal neoplasms. Cancer. 2004;101(7):1537-1544.
doi pubmed - Lal TG, Kaulback KR, Bombonati A, Palazzo JP, Jeffrey RB, Weigel RJ. Surgical management of adrenal cysts. Am Surg. 2003;69(9):812-814.
pubmed - Lee TH, Slywotzky CM, Lavelle MT, Garcia RA. Cystic pheochromocytoma.Radiographics. 2002;22(4):935-940.
pubmed - Klingler PJ, Fox TP, Menke DM, Knudsen JM, Fulmer JT. Pheochromocytoma in an incidentally discovered asymptomatic cystic adrenal mass. Mayo Clin Proc. 2000;75(5):517-520.
pubmed - Rozenblit A, Morehouse HT, Amis ES, Jr. Cystic adrenal lesions: CT features. Radiology. 1996;201(2):541-548.
pubmed - Lenders JW, Eisenhofer G, Mannelli M, Pacak K. Phaeochromocytoma. Lancet. 2005;366(9486):665-675.
doi - Grozinsky-Glasberg S, Szalat A, Benbassat CA, Gorshtein A, Weinstein R, Hirsch D, Shraga-Slutzky I, et al. Clinically silent chromaffin-cell tumors: Tumor characteristics and long-term prognosis in patients with incidentally discovered pheochromocytomas. J Endocrinol Invest. 2010;33(10):739-744.
pubmed - Young WF, Jr. Clinical practice. The incidentally discovered adrenal mass. N Engl J Med. 2007;356(6):601-610.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


